Abstract
Purpose
Atrial natriuretic peptide (ANP) has a variety of pharmacologic effects, including natriuresis, diuresis, vasodilatation, and suppression of the renin-angiotensin system. A recent study showed that ANP infusion improved hypoxemia and pulmonary hypertension in a lung injury model. On the other hand, the pulse contour cardiac output (PiCCO™) system (Pulsion Medical Systems, Munich, Germany) allows monitoring of the intravascular volume status and may be used to guide volume therapy in severe sepsis and critically ill patients.
Materials and Methods
We treated 10 pulmonary edema patients without heart disease with human ANP (HANP). The patients were divided into two groups: a group with normal Intrathoracic Blood Volume (ITBV) (900-1100 mL/m2) (n = 6), and a group with abnormal ITBV (n = 4), as measured by the PiCCO™ device; the extravascular lung water (EVLW) and pulmonary vascular permeability index (PVPI) in the two groups were compared.
Results
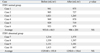
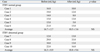
The average patient age was 63.9 ± 14.4 years. The normal ITBV group showed significant improvement of the EVLW (before, 16.7 ± 2.7 mL/kg; after, 10.5 ± 3.6 mL/kg; p = 0.0020) and PVPI (before, 3.2 ± 0.3; after, 2.1 ± 0.7; p = 0.0214) after the treatment. The abnormal ITBV group showed no significant improvement of either the EVLW (before, 16.3 ± 8.9 mL/kg; after, 18.8 ± 9.6 mL/kg; p = 0.8387) or PVPI (before, 2.3 ± 0.8; after, 2.7 ± 1.3; p = 0.2782) after the treatment. In both groups, the EVLW and PVPI were strongly correlated with the chest X-ray findings.
Plasma concentrations of atrial natriuetic peptide (ANP), one of the key hormones involved in the regulation of body fluid and blood pressure,1 have been shown to be correlated with the severity of acute lung injury.2 A recently published study reported that significant diuresis associated with an increase in the plasma ANP levels preceded the improvement of pulmonary function in patients with infantile respiratory distress syndrome.3,4 ANP has a variety of pharmacologic effects, including natriuresis, diuresis, vasodilatation, and suppression of the renin-angiotensin system. A previous study showed that ANP infusion improved hypoxemia and pulmonary hypertension in a lung injury model.5 In respect of clinical reports, Mitaka, et al.6 suggested that ANP infusion induces diuresis and improves the pulmonary gas exchange in patients with acute lung injury during mechanical ventilation using positive end-expiratory pressure. Sumi, et al.7 showed that ANP may be a useful therapeutic choice for the control of pulmonary circulation during abdominal aortic surgery.
On the other hand, the pulse contour cardiac output (PiCCO™) system (Pulsion Medical Systems) allows monitoring of the intravascular volume status and may be used to guide volume therapy in severe sepsis and critically ill patients. The extravascular lung water (EVLW) volume has also been demonstrated to be well correlated with the oxygenation level in septic shock patients with acute lung injury (ALI) and acute respiratory distress syndrome (ARDS).8
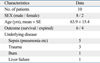
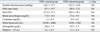
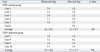
We treated 10 pulmonary edema patients without heart disease with human ANP (HANP). We administered HANP at the dose of 0.1 µg/kg/min by intravenous injection. All the patients were hemodynamically stabilized and mechanically ventilated and sedated. A thermo-fiber-optic catheter was inserted into the femoral or brachiocephalic artery in each patient (Pulsiocath 4F, PV 2024L, Pulsion Medical Systems, Munich, Germany), and the catheter was connected to a bed box and a computer system (Cold-Z021, Pulsion Medical Systems, Munich, Germany). The PiCCO system can be used to measure any physiological parameter, including Intrathoracic Blood Volume (ITBV), extravascular lung water (EVLW), and the pulmonary vascular permeability index (PVPI) (Table 1). Classification of pulmonary edema using PVPI as measured using the PiCCO system is shown in Fig. 1.
The patients were divided into two groups: a group with normal ITBV (900-1,100 mL/m2) (n = 6) and a group with abnormal ITBV (n = 4), as measured with the PiCCO™ device. The EVLW and PVPI in the two groups were compared. The study was conducted with the approval of our institution's ethics committee and informed consent from each patient was obtained prior to the start of the study. Differences were analyzed using the Wilcoxon's generalized test. p-values less than 0.05 were regarded as denoting statistical significance.
We treated 10 pulmonary edema patients without heart disease with HANP. The average patient age was 63.9 ± 14.4 years; 8 of the patients were men and 2 were women. The major underlying disease was sepsis in all the patients (Table 2). The pretreatment vital signs and laboratory data was not significantly different between the normal and abnormal ITBV groups (Table 3). The change of the ITBV after HANP administration in each case is shown in Table 4. The normal ITBV group showed significant improvement of the EVLW (before, 16.7 ± 2.7 mL/kg; after, 10.5 ± 3.6 mL/kg; p = 0.0020) and PVPI (before, 3.2 ± 0.3; after, 2.1 ± 0.7; p = 0.0214) after the HANP treatment (Tables 5 and 6). The abnormal ITBV group showed no significant improvement of either the EVLW (before, 16.3 ± 8.9 mL/kg; after, 18.8 ± 9.6 mL/kg; p = 0.8387) or PVPI (before, 2.3 ± 0.8; after, 2.7 ± 1.3; p = 0.2782) after the HANP treatment (Tables 5 and 6). None of the patients of the normal ITBV group were given any other diuretic agents. On the other hand, two patients (case 8 and 10) of the abnormal ITBV group were given the diuretic furosemide as needed. In regard to the administration of vasopressor agents, noradrenalin (0.1-0.05γ) was administered to 5 patients (Cases 2, 3, 4, 9 and 10). Dopamine, which may also have the effect of facilitating diuresis, was not administered to any of the patients.
In both groups, the EVLW and PVPI were strongly correlated with the chest X-ray findings. We confirmed that the normal ITBV cases showed improvement of the EVLW and that the PaO2/FiO2 ratio correlated well with the improvement of the chest X-ray permeability findings (Figs. 2 and 3). On the other hand, the abnormal ITBV cases showed no improvement of the EVLW, and the PaO2/FiO2 ratio was not correlated with the chest X-ray permeability findings (Figs. 4 and 5).
A previous study showed that HANP treatment improved the arterial oxygenation and lung injury score in patients with acute lung injury during mechanical ventilation using positive end-expiratory pressure (PEEP).6 The following mechanisms are speculated to underlie the effectiveness of HANP in cases of lung injury. HANP directly improves pulmonary edema by arachidonic acid,9 thrombin,10 and oxidant.11 A recent study reported that HANP treatment during aortic clamping and abdominal aortic aneurysmectomy attenuated the rises in pulmonary artery pressure and vascular resistance without producing severe systemic hypotension.7 However, several studies have also suggested that HANP treatment is not effective for pulmonary edema not associated with heart disease. Therefore, the criteria for the administration of HANP for pulmonary edema not associated with heart disease has not been established. This study showed that HANP supplementation may improve the EVLW and PVPI in pulmonary edema patients without heart disease with a normal ITBV. We propose that pulmonary edema patients without heart disease with an abnormal ITBV be treated using other strategies, namely water removal by continuous hemodiafiltration.
Pulmonary edema is one of the most common problems in critically ill patients and has a significant influence on the outcome of their health. However, it is difficult to precisely diagnose low permeability on the chest X-ray in patients with respiratory distress. The PiCCO™ system allows monitoring of the intravascular volume status and can be used to guide volume therapy in patients with pulmonary edema. We showed that the PiCCO™ system might be a useful device for the management of pulmonary edema using HANP.
The limitations of this study were its retrospective design, small sample size, and lack of a control group. Nonetheless, we demonstrated the efficacy of HANP and usefulness of the PiCCO™ system in pulmonary edema patients.
Many conditions limiting the usefulness of systems using dilution methods, such as the PiCCO™ system, under experimental conditions, have been described, which may lead to an underestimation of the EVLW. These conditions include large pulmonary vascular obstruction, focal lung injury, and lung resection.12 Patients with the above conditions were not included for our examination.
HANP supplementation may improve the EVLW and PVPI in pulmonary edema patients without heart disease with a normal ITBV. The PiCCO™ system seems to be a useful device for the management of pulmonary edema in critically ill patients.
Figures and Tables
 | Fig. 1Classification of pulmonary edema based on the IBPV as measured using the PiCCO system. Results of categorization by the PiCCO system, of pulmonary edema patients in whom a precise diagnosis of pulmonary edema could not be made. IBPV, Intrathoracic Blood Volume; PiCCO, pulse contour cardiacoutput. |
 | Fig. 2Changes of chest X-ray findings after carperitide therapy (case 1). Pre treatment: The chest X-ray permeability finding was abnormal. Post treatment: The normal ITBV cases showed improvement of the EVLW, and the PaO2/FiO2 ratio was correlated with the improvement of the chest X-ray permeability findings. |
 | Fig. 3Changes of chest X-ray findings after carperitide therapy (case 2). Pre treatment: The chest X-ray permeability finding was abnormal. Post treatment: The normal ITBV cases showed improvement of the EVLW, and the PaO2/FiO2 ratio was correlated with the improvement of the chest X-ray permeability findings just like case 1. |
 | Fig. 4Change of chest X-ray findings after HANP therapy (case 7). Pre treatment: The chest X-ray permeability finding was abnormal. Post treatment: The abnormal ITBV cases showed no improvement of the EVLW, and the PaO2/FiO2 ratio was not correlated with the chest X-ray permeability findings. |
 | Fig. 5Changes of chest X-ray findings after HANP therapy (case 8). Pre treatment: The chest X-ray permeability finding was abnormal. Post treatment: The abnormal ITBV cases showed no improvement of the EVLW, and the PaO2/FiO2 ratio was not correlated with the chest X-ray permeability findings just like case 7. |
References
1. Needleman P, Greenwald JE. Atriopeptin: a cardiac hormone intimately involved in fluid, electrolyte, and blood-pressure homeostasis. N Engl J Med. 1986. 314:828–834.

2. Tanabe M, Ueda M, Endo M, Kitajima M. Effect of acute lung injury and coexisting disorders on plasma concentrations of atrial natriuretic peptide. Crit Care Med. 1994. 22:1762–1768.

3. Langman CB, Engle WD, Baumgart S, Fox WW, Polin RA. The diuretic phase of respiratory distress syndrome and its relationship to oxygenation. J Pediatr. 1981. 98:462–466.

4. Heaf DP, Belik J, Spitzer AR, Gewitz MH, Fox WW. Changes in pulmonary function during the diuretic phase of respiratory distress syndrome. J Pediatr. 1982. 101:103–107.

5. Tanabe M, Ueda M, Endo M, Kitajima M. The effect of atrial natriuretic peptide on pulmonary acid injury in a pig model. Am J Respir Crit Care Med. 1996. 154:1351–1356.
6. Mitaka C, Hirata Y, Nagura T, Tsunoda Y, Amaha K. Beneficial effect of atrial natriuretic peptide on pulmonary gas exchange in patients with acute lung injury. Chest. 1998. 114:223–228.
7. Sumi K, Iida H, Yamaguchi S, Fukuoka N, Shimabukuro K, Dohi S. Human atrial natriuretic peptide prevents the increase in pulmonary artery pressure associated with aortic unclamping during abdominal aortic aneurysmectomy. J Cardiothorac Vasc Anesth. 2008. 22:204–209.

8. Berkowitz DM, Danai PA, Eaton S, Moss M, Martin GS. Accurate characterization of extravascular lung water in acute respiratory distress syndrome. Crit Care Med. 2008. 36:1803–1809.

9. Imamura T, Ohnuma N, Iwasa F, Furuya M, Hayashi Y, Inomata N, et al. Prorective effect of aipha-human atrial natriuretic polypeptide (alpha-hANP) on chemical induced pulmonary edema. Life Sci. 1988. 42:403–414.

10. Baron DA, Lofton CE, Newman WH, Currie MG. Atriopeptin inhibition of thrombin-mediated changes in the morphology and permeability of endothelial monolayers. Proc Natl Acad Sci U S A. 1989. 86:3394–3398.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download