Abstract
We report a rare case of a massive fatal embolism that occurred in the middle of endoscopic retrograde cholangiopancreatography (ERCP) and retrospectively examine the significant causes of the event. The patient was a 50-year old female with an uncertain history of previous abdominal surgery for multiple biliary stones 20 years prior. The patient presented with acute right upper quadrant pain. An abdominal computed tomographic (CT) scan revealed the presence of multiple stones in the common bile duct (CBD) and intra-hepatic duct (IHD) with biliary obstruction, multifocal liver abscesses, and air-biliarygram. Emergency ERCP showed a wide and straight opening of choledochoduodenostomy, which may have been created during a previous surgery, and multiple filling defects in the CBD. With the use of a forward endoscope, mud stones were extracted through the opening of the choledochoduodenostomy. Cardiac arrest suddenly developed during the procedure, and despite immediate resuscitation, the patient died due to a massive systemic air embolism. We reviewed previously reported fatal cases and accessed factors facilitating air embolisms in this case.
Currently, gastro-intestinal endoscopic procedures are routinely performed. Air embolisms that occur as an intra-operative complication from various endoscopic procedures has been reported in some cases.1 Most of the occurrences are portal venous air embolisms, which are absorbed spontaneously. However, serious complications have occurred, including cerebral air embolisms2-4 and fatal air embolisms that have resulted in cardiovascular collapse.1,5-8 Four fatal cases have been reported during the practice of endoscopic retrograde cholangiopancreatography (ERCP) since the procedure has became a major tool in manipulating the hepatobiliary pathology.1,5,7,8 Possible etiologies of developing portal venous gas in these cases are invasive procedures disrupting a gastro-intestinal or hepatobiliary structure such as a liver biopsy, sphincterotomy, percutaneous transhepatic biliary drainage (PTBD), and high intra-luminal pressure of insufflated air. We recently experienced a unique case where a fatal air embolism occurred during an ERCP in a patient that presented with multiple liver abscesses and a history of a choledochoduodenostomy.
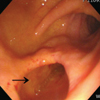
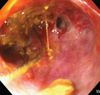
A 50 year-old female visited the emergency department with a 15-day history of epigastric pain, fever, chill, and nausea. The patient had a history of abdominal surgery for multiple biliary stones 20 years prior but was not able to recall detailed information. The patient complained of acute, continuous, dull-like pain, located in the epigastrium without any radiation, and, on a physical examination, the abdomen was soft but tender on the right upper quadrant area with no rebound tenderness. Initial laboratory test results were as follows: white blood cell count, 14,760/mm3; hemoglobin level, 10.0 g/dL; erythrocyte sedimentation ratio, 140 mm/hr (normal range, 1-20 mm/hr); c-reactive protein level, 23.89 mg/dL (normal range, 0-0.3 mg/dL); aspartate aminotransferase level (AST), 101 IU/L (normal range, 10-40 IU/L); alanine aminotransferase (ALT) level, 114 IU/L (normal range, 5-40 IU/L); total billirubin, 4.6 mg/dL (normal range, 0.2-1.2 mg/dL); amylase level, 48 U/L (normal range 20-125 U/L). An abdominal computed tomographic (CT) scan revealed the presence of multiple stones in the common bile duct (CBD) and intra-hepatic duct (IHD) with biliary obstruction, multifocal liver abscesses, and air-biliarygram (Fig. 1). Emergency ERCP was subsequently performed. On an initial examination, an opening of a choledochoduodenostomy, which may have been created at the previous surgery (Fig. 2, arrow), was observed. Cholangiogram confirmed multiple filling defects in the CBD. Due to the presence of a wide and straight ostomy orifice and the marked dilatation of the CBD, with the use of a forward endoscope (GIF-XQ260, Olympus, Tokyo, Japan) we were able to commence the extraction of brown-pigmented mud stones without difficulty (Fig. 3). In the middle of the procedure, the patient suddenly became hypoxic and bradycardic. The patient was soon comatose, and cardiac arrest developed. The procedure was immediately terminated and cardio-pulmonary resuscitation commenced followed by prompt intubation. The patient was transferred to the intensive care unit while resuscitation was continued. However, the patient died without restoration despite of all efforts. A chest X-ray taken at the scene suggested a massive systemic air embolism (Fig. 4). The cause of death was thought to be a massive cardiac and pulmonary air embolism originated from the biliary-venous fistula.
Portal venous gas results from pathologic state of the intestinal wall that permits intraluminal gas to enter the mesenteric veins via the damaged intestinal walls. The presence of portal venous gas is considered as not only a transient finding but an ominous prognostic sign in severely ill cases, such as ischemic bowel disease or intra-abdominal sepsis.9 Since endoscopic procedures have become standard methods for exploring the gastrointestinal and hepatobiliary systems, few cases of portal venous air embolisms have also been reported.1 Venous air embolisms have been observed in association with ERCP during sphincterotomy,10-12 gastro-duodenoscopy manipulating bleeding vessels in a peptic ulcer and duodenocaval fistula,2,13 and a colonoscopy investigating active Crohn's disease.14 Most of the cases had usually been resolved without significant incidents.
However, fatal cases of systemic air embolisms including cardiac and cerebral embolisms have occurred,2-4,6 and four events that originated from ERCP following a liver biopsy,7 sphincterotomy,1,5 and percutaneous transhepatic biliary drainage (PTBD)8 have been described. In a retrospective review of these cases, several contributing factors for promoting air embolism during ERCP have been suggested. Iatrogenic fistulas between the biliary and venous system within the liver, which were made during a liver biopsy or PTBD, provided direct communication for the passing air embolism. Sphincterotomy during ERCP also disrupts the gastrointestinal mucosal integrity and creates shunts between the veins in the duodenal walls and the intestinal cavity filled with insufflated air. A significant amount of air may travel to the heart via the fistulas or shunts, and it ends up filling the pulmonary vessels to cause a cardiovascular collapse. High intraluminal air pressure to keep the intestines distended may facilitate the progression of an embolism and may be considered as a common etiologic factor in catastrophic cases.
The present case demonstrates particular features that may have caused an air embolism to develop during the endoscopic procedure. Multiple liver abscesses and already existing air in the biliary trees seen on an abdominal CT scan predicate a distorted structure of the liver parenchyme. These abnormally weakened structures could have been easily broken by pressure generated from instilled air. Biliary-hepatic venous fistulas probably opened in the interrupted tissues, and air inside bile ducts could have spread into the systemic circulation. Another important factor is the wide opening of a choledochoduodenostomy. This broad and straight structure directly communicated with the intra-hepatic biliary ducts. It not only enabled us to remove the stones with a forward endoscope, but also allowed a push of a substantial amount of air and pressure into the hepatic venous circulation. We could formulate that these specific factors caused the air embolism to disseminate into a cardio-pulmonary system rapidly and induce a sudden arrest of the patient. We should have noticed the possibility of a fatal air embolism as soon as we discovered the abnormal structure of the hepatobiliary system that was seen on the CT scan and the presence of the unusual choledochoduodenostomy on the primary survey during the ERCP.
We reported a rare case of a fatal air embolism that occurred during ERCP in a patient with multiple liver abscesses and a history of a choledochoduodenostomy. Sphincterotomy, procedures interrupting the liver architecture including a percutaneous liver biopsy and PTBD, the pathological state of the hepato-biliary tissues vulnerable to barotraumas such as multiple liver abscesses, and high pressure generated by insufflated air may be the underlying causes of the fatal air embolism during ERCP. Furthermore, endoscopists should always be aware of the possible development of massive air embolisms when the basic vital and neurologic signs deteriorate abruptly in the course of the procedure.
Figures and Tables
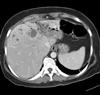 | Fig. 1Abdominal CT scan showing multiple stones in the CBD and IHD with biliary obstruction, multifocal liver abscesses, and air-biliarygram. CBD, common bile duct; IHD, intra-hepatic duct. |
References
1. Nayagam J, Ho KM, Liang J. Fatal systemic air embolism during endoscopic retrograde cholangio-pancreatography. Anaesth Intensive Care. 2004. 32:260–264.

2. Christi SU, Scheppach W, Peters U, Kirchner T. Cerebral air embolism after gastroduodenoscopy: complication of a duodenocaval fistula. Gastrointest Endosc. 1994. 40:376–378.
3. Raju GS, Bcndixen BH, Khan J, Summers RW. Cerebrovascular accident during endoscopy: consider cerebral air embolism, a rapidly reversible event with hyperbaric oxygen therapy. Gastrointest Endosc. 1998. 47:70–73.

4. Akhtar N, Jafri W, Mozaffar T. Cerebral artery air embolism following an esophagogastroscopy: a case report. Neurology. 2001. 56:136–137.

5. Kennedy C, Larvin M, Linsell J. Fatal hepatic air embolism following ERCR. Gastrointest Endosc. 1997. 45:187–188.
6. Mohammedi I, Ber C, Peguet O, Ould-Aoudia T, Duperret S, Petit P. Cardiac air embolism after endoscopic retrograde cholangiopancreatography in a patient with blunt hepatic trauma. J Trauma. 2002. 53:1170–1172.

7. Siddiqui J, Jaffe PE, Aziz K, Forouhar F, Sheppared R, Covault J, et al. Fatal air and bile embolism after percutaneous liver biopsy and ERCP. Gastrointest Endosc. 2005. 61:153–157.

8. Stabile L, Cigada M, Stillittano D, Morandi E, Zaffaroni M, Rossi G, et al. Fatal cerebral air embolism after endoscopic retrograde cholangiopancreatography. Acta Anaesthesiol Scand. 2006. 50:648–649.

9. Liebman PR, Patten MT, Manny J, Benfield JR, Hechtman HB. Hepatic--portal venous gas in adults: etiology, pathophysiology and clinical significance. Ann Surg. 1978. 187:281–287.
10. Simmons TC. Hepatic portal venous gas due to endoscopic sphincterotomy. Am J Gastroenterol. 1988. 83:326–328.
11. Barthet M, Membrini P, Bernard JP, Sahel J. Hepatic portal venous gas after endoscopic biliary sphincterotomy. Gastrointest Endosc. 1994. 40:261–263.

12. Herman JB, Levine MS, Long WB. Portal venous gas as a complication of ERCP and endoscopic sphincterotomy. Am J Gastroenterol. 1995. 90:828–829.
13. Katzgraber F, Glenewinkel F, Rittner C, Beule J. Fatal air embolism resulting from gastroscopy. Lancet. 1995. 346:1714–1715.
14. Huycke A, Moeller DD. Hepatic portal venous gas after colonoscopy in granulomatous colitis. Am J Gastroenterol. 1985. 80:637–638.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download