Abstract
A gastropericardial fistula, defined as penetration of a gastric lesion into the pericardium, is a rare occurrence. Such a fistula is usually associated with a huge ulcer in the gastric fundus, an ulcer within a hiatus hernia, a history of esophagogastric surgery, the concurrent use of non-steroidal anti-inflammatory drugs (NSAIDs), or Zollinger-Ellison syndrome. The patient in this case presented with shoulder pain and melena, caused by a gastropericardial fistula that had occurred as a late complication of postoperative esophagogastrostomy and a refractory gastric ulcer. Despite the severity of the condition, the patient showed great improvement after medical treatment and the fistula was cured at the end.
Clinically, a gastropericardial fistula is a very rare condition. It often presents with an acute onset of chest pain with radiating shoulder pain, as well as signs of pneumopericardium, pericarditis, subphrenic abscess, and catastrophic cardiac tamponade.1-5 Therefore, gastropericardial fistula results in a mortality rate greater than 50 percents.6
Pneumopericardium was first described by Britcheteau in 1844,7 who defined it as a collection of air or gas within the pericardial sac, usually caused by trauma. Non-traumatic pneumopericardium or gastropericardial fistula is usually associated with the perforation of a benign gastric ulcer or malignancy. The most common risk factor for gastropericardial fistula is a previous gastroesophageal surgery such as Nissen fundoplication for refractory reflux esophagitis.1,6
This case report deals with a gastropericardial fistula that had developed on an intrathoracic gastric ulcer after esophagectomy with esophagogastrostomy 7 years ago. The patient was successfully treated with conservative medical care for the gastric ulcer and fistula, and he was able to maintain a good general condition for 2 years with no additional operations.
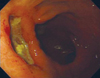
A 62 year-old man was admitted to Severance hospital, Seoul, Korea with a chief complaint of left shoulder pain for 2 months and melena for 1 week. He had been treated for diabetes mellitus for 3 years and had a smoking history of 30 pack-years. His medical history included esophagectomy with esophagogastrostomy due to an esophageal rupture caused by a lodged chicken bone 8 years prior. This gastric transposition was performed by the substernal route. The patient also underwent several esophageal dilations because he suffered an esophageal stricture due to lye ingestion more than 11 years ago. Upon admission, laboratory studies revealed that he had mild leukocytosis (13,800/uL) and severe anemia (Hb 5.5 g/dL). Chest radiographs showed mild pulmonary edema without evidence of pneumopericardium. On endoscopic examination, there was a huge, deeply penetrating gastric ulcer on the anterior wall of the upper body (Fig. 1). A gastrograffin chest CT scan was then performed, showing a focal lesion bulging out of the posterior gastric wall and protruding into the pericardial space with severe thickening of the adjacent pericardium. However, there were no signs of gastrograffin leakage. The fistula between the posterior wall of the transposed stomach and pericardium was probably sealed off, resulting in an adhesion (Fig. 2). Pathology revealed the presence of Helicobacter gastritis in the gastric ulcer. He was conservatively treated, including proton pump inhibitor and H. pylori eradication. A follow-up endoscopy was performed approximately 2 weeks later, showing great improvement (Fig. 3). However, 2 months later, the patient came to the emergency department with severe epigastric pain and left shoulder pain. The endoscopy showed a deep, active gastric ulcer at the same location as the previous ulcer. Therefore, it was decided to operate for the medically intractable ulcer. This operation required caution due to his previous surgical history. There was a possibility that a colonic interposition might be needed as a substitute for the esophagus and stomach. However, because the conservative care prior to the operation showed excellent results, the colonic interposition was not necessary. After 2 weeks, the ulcer had improved to the healing stage. He had no additional operations, and remained asymptomatic after 2 years, maintaining good condition.
Gastropericardial fistula is a highly fatal condition that is frequently found following intrathoracic stomach resection, laparoscopic Nissen fundoplication, refractory gastric ulcers, or esophagogastric malignancies.2,6 The common clinical presentation for this condition ranges from heartburn, epigastric pain, shoulder pain, dyspnea, and tachycardia to cardiac tamponade and even hypovolemic shock.
A refractory ulcer is defined as an ulcerative lesion that fails to heal after 8 to 12 weeks of conventional ulcer therapy, such as H2-antagonists and high doses of proton pump inhibitors.8,9 The pathogenesis of gastric ulcers is associated with abnormalities of motility and attenuation of mucosal blood flow rather than hyperacidity.10 Factors associated with poor healing of gastric ulcers include tolerance to H2-antagonists, long-term use of non-steroidal anti-inflammatory drugs (NSAIDs) or anticoagulants, persistence of H. pylori infection, malignancy, and poor compliance with therapy.9,11
According to some reports, the absence or reduction of TGF-β is associated with delayed healing in gastric mucosa of patients with refractory gastric ulcers, and gastric microcirculation plays an important role in gastric mucosal defense and healing.9 Therefore, an ulcer which develops in the intrathoracic stomach, especially the fundus, possesses a possibility of poor ulcer healing due to impaired gastric microcirculation and scar formation.11 However, insufficient studies concerning intrathoracic pull-up stomach pathology related to ulcer development currently exist. We believe that the gastropericardial fistula might develope from scar tissue formed at the site of the previous esophagogastric surgery. Gastropericardial fistula in this patient possibly resulted in adherence of the gastric fundus or lower esophagus to the pericardium, and produced a pathway for benign ulcers to erode into the pericardium. The ulcer healed very slowly because the patient had many gastric ulcer-inducing factors, including H. pylori infection, a smoking history of more than 30 pack-years, regular intake of NSAIDs, and impaired gastric microcirculation caused by the intrathoracic stomach. Thus, when diagnosed with an ulcer in the intrathoracic stomach, patients should be strongly warned against ulcer-inducing factors. We anticipate that this case will inform future management of gastropericardial fistula patients. Further studies are needed to examine the significance of gastric ulcer surveillance for intrathoracic stomach patients, and the pathological differences between intrathoracic and non-intrathoracic stomachs, in order to improve treatment results.
The case reported here concerns a gastropericardial fistula that occurred as a late complication of postoperative esophagogastrostomy and refractory gastric ulcer. Despite the severity of this condition, the patient showed great improvement through medical treatment, and the fistula was cured. We conclude that although the first treatment approach for most of gastropericardial fistulas is surgical, conservative management can also benefit the patient.
Figures and Tables
Fig. 1
Esophagogastroduodenoscopy revealing a huge, deeply penetrating gastric ulcer on the anterior wall of the upper body.

References
1. Sihvo EI, Räsänen JV, Hynninen M, Rantanen TK, Salo JA. Gastropericardial fistula, purulent pericarditis, and cardiac tamponade after laparoscopic Nissen fundoplication. Ann Thorac Surg. 2006. 81:356–358.

2. Chinnaiyan KM, Ali MI, Gunaratnam NT. Gastric cancer presenting as gastropericardial fistula in a patient with familial adenomatous polyposis syndrome. J Clin Gastroenterol. 2004. 38:298.

3. Kaur H, Singh D, Kirschner ES, Maxwell JS. True heartburn: a case of gastropericardial fistula. J Clin Gastroenterol. 2001. 32:458.
4. Ikard RW, Jacobs JK. Gastropericardial fistula and pericardial abscess: unusual complications of subphrenic abscess following Nissen fundoplication. South Med J. 1974. 67:17–19.
5. Farjah F, Komanapalli CB, Shen I, Sukumar MS. Gastropericardial fistula and Candida kruzei pericarditis following laparoscopic Nissen fundoplication (gastropericardial fistula). Thorac Cardiovasc Surg. 2005. 53:365–367.

6. Murthy S, Looney J, Jaklitsch MT. Gastropericardial fistula after laparoscopic surgery for reflux disease. N Engl J Med. 2002. 346:328–332.

7. Grandhi TM, Rawlings D, Morran CG. Gastropericardial fistula: a case report and review of literature. Emerg Med J. 2004. 21:644–645.

8. Raju GS, Bardhan KD, Royston C, Beresford J. Giant gastric ulcer: its natural history and outcome in the H2RA era. Am J Gastroenterol. 1999. 94:3478–3486.

9. Shih SC, Tseng KW, Lin SC, Kao CR, Chou SY, Wang HY, et al. Expression patterns of transforming growth factor-beta and its receptors in gastric mucosa of patients with refractory gastric ulcer. World J Gastroenterol. 2005. 11:136–141.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download