Abstract
Purpose
Methylenetetrahydrofolate reductase (MTHFR) is the main regulatory enzyme for homocysteine metabolism. In the present study, we evaluated whether the MTHFR 677C>T and 1298A>C gene polymorphisms are associated with SBI and plasma homocysteine concentration in a Korean population.
Materials and Methods
We enrolled 264 patients with SBI and 234 healthy controls in South Korea. Fasting plasma total homocysteine (tHcy) concentrations were measured, and genotype analysis of the MTHFR gene was carried out.
Results
The plasma tHcy levels were significantly higher in patients with SBI than in healthy controls. Despite a significant association between the MTHFR 677TT genotype and hyperhomocysteinemia, the MTHFR 677C>T genotypes did not appear to influence susceptibility to SBI. However, odds ratios of the 1298AC and 1298AC + CC genotypes for the 1298AA genotype were significantly different between SBI patients and normal controls. The frequencies of 677C-1298A and 677C-1298C haplotypes were significantly higher in the SBI group than in the control group.
Silent brain infarction (SBI) is defined as an asymptomatic infarction, and is often incidentally detected on computed tomography (CT) or magnetic resonance imaging (MRI) in subjects with no history of stroke. It is relatively common in the elderly, and the incidence of SBI significantly increases with older age.1,2 The presence of SBI has been identified as an independent risk factor for the development of symptomatic infarction.3-7 Therefore, population-based studies have been performed to identify risk factors for SBI, as well as factors that promote the progression of SBI to other symptomatic cerebrovascular disorders.8
It has been suggested that hyperhomocysteinemia is a risk factor for a number of occlusive vascular diseases, including SBI.2,9-12 The methylenetetrahydrofolate reductase (MTHFR) gene has genetic variants (677C>T and 1298A>C) that reduce the enzyme activity, thereby elevating plasma total homocysteine (tHcy) levels.13-17 Most previous studies have concentrated on the MTHFR 677C>T polymorphisms associated with stroke, cancer, birth defects, recurrent abortion, and cardiovascular disorders.15,18-24 However, only a few studies have been conducted to assess the association of a second common polymorphism, 1298A>C, with ischemic stroke, cancer, and heart disease.25-31 No association studies of the MTHFR 1298A>C polymorphism with SBI were conducted.
Therefore, we conducted this study to investigate the association between the MTHFR 677C>T and 1298A>C polymorphisms and the risk of SBI in a Korean population.
The study population was composed of 264 patients (121 males, 143 females; mean age ± SD, 62.26 ± 11.95 years) with SBI and 227 control subjects (109 males, 118 females; mean age ± SD, 59.62 ± 11.67 years). Patients with SBI were enrolled and recruited between July 2000 and February 2005 in the Bundang CHA Hospital.
Patients with known history of stroke or cardiovascular diseases were excluded. MRI was performed on a 1.5-T superconducting magnet (Siemens Magnetom Symphony, Erlangen, Germany). Transverse T1-weighted, T2-weighted, and FLAIR images were obtained with a slice thickness of 7 mm. The diagnosis of SBI was made as follows: 1) spotty areas ≥ 3 mm in diameter in the area supplied by deep perforating arteries, showing high intensity in the T2 and FLAIR images and low intensity in the T1 image; 2) absence of neurological signs and symptoms corresponding to the MRI lesions; 3) no history of clinical stroke, including transient ischemic attack. Small punctate hyperintensity lesions (1 to 2 mm in diameter) were more likely to represent a dilated perivascular space, and were not considered in the present study. The diagnosis of SBI was made when two independent researchers agreed on the diagnosis.
Controls (n = 227), which showed no evidence of SBI on MRI, were recruited from subjects who visited the hospital for a health examination. They had no past history of stroke or cardiovascular disease. Our subjects were classified into two age groups: subjects aged < 65 years and subjects aged ≥ 65 years. Baseline demographic data and a history of conventional vascular risk factors were obtained from each control subject. Detailed information on medical history was obtained from all study subjects. The institutional review committee of Bundang CHA Hospital approved this study in June 2000. Informed consent was obtained from all participants.
Overnight fasting (12 hours) blood samples were collected in EDTA-containing tubes and immediately placed on ice. After centrifugation at 2000 rpm for 15 minutes, plasma samples were kept at -20℃ until analysis. Plasma total homocysteine (tHcy) levels were determined by fluorescence polarization immunoassay (IMx, Abbott Laboratories, North Chicago, IL, USA).
Genomic DNA was extracted from leukocytes by using a DNA extraction kit (QIAmp blood kit, Qiagen) according to the protocol of the manufacturer. MTHFR 677C>T and 1,298A>C genotypes were identified as described previously.15,17 Regions containing the two polymorphisms were amplified separately. For the nucleotide 677 polymorphism, the primers 5'-GCA CTT GAA GAG AAG GTG TC-3' (forward) and 5'-AGG ACG GTG CGG TGA GAG TG-3' (reverse) were used, and for the nucleotide 1298 polymorphism, 5'-CTT TGG GGA GCT GAA GGA CTACTA C-3' (forward) and 5'-CAC TTT GTG ACC ATT CCG GTT TG-3' (reverse) were used. Human genomic DNA (200 ng) was amplified with 100 pmol of each forward and reverse primer, 1.5 mM MgCl2, 0.2 M each deoxynucleotide triphosphate, and 1 unit Taq polymerase (Takara, Madison, Wisconsin, USA) in a total volume of 100 uL. PCR conditions were as follows: denaturation at 94℃ for 5 min, followed by 35 cycles at 94℃ for 30s, 51℃ for 30s, and 72℃ for 30s, and a final terminal elongation at 72℃ for 5 min. PCR products were digested with HinfI (for nucleotide 677) or Fnu4HI (for nucleotide 1,298) for 2 hours at 37℃.
Amplification success was monitored by 3.0% agarose electrophoresis. For the nucleotide 677, an undigested PCR product (203 bp) indicated a homozygous wild-type, three bands of 203, 173, and 30 bp indicated the heterozygous genotype, and two bands of 170 and 30 bp indicated the homozygous genotype. For nucleotide 1,298, a single band of 138 bp indicated a wild-type, and two fragments of 119 and 19 bp indicated the homozygous genotype.
To estimate the relative risk for SBI for the various genotypes, an odds ratio (OR) and 95% confidence interval (CI) were calculated. Differences between the patient and control groups were assessed by the χ2 test for categorical variables (sex, hypertension, and diabetes mellitus) and the two-sample t-test for continuous variables (age and tHcy level). For the multivariate analysis, logistic regression analysis was used to adjust for possible confounders, including age, sex, hypertension, and diabetes mellitus. The plasma tHcy levels differences between patients and controls were examined by analysis of covariance (ANCOVA), adjusted for age and sex. Haplotypes analysis was performed using case-control haplotype analysis-permutation test.
The analysis was performed using GraphPad Prism 4.0 (GraphPad Software Inc., San Diego, CA, USA), Stats-Direct Statistical Software Version 2.4.4 (StatsDirect Ltd., Altrincham, UK), Medcalc (version 7.4 for Windows; Frank. Schoonjans, Belgium) and SAS 9.1 for Windows (SAS Institute Inc., Cary, NC, USA).
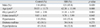
Table 1 shows the distributions of clinical characteristics of patients with SBI and control subjects. Patients had a significantly higher prevalence of hyperlipidemia, but not of diabetes mellitus or hypertension, compared to the controls. To evaluate the pure effects of the MTHFR genotypes on SBI, we adjusted the OR for age, sex, hypertension, and diabetes mellitus. Significant elevation of pHcy concentrations was found in patients compared to controls (11.34 ± 6.385 µmol/L vs. 9.676 ± 3.959 µmol/L, p = 0.0007).
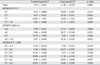
In this study, all of the study populations were in Hardy-Weinberg equilibrium. The 1298AC genotype was found to show a significant 1.734-fold increased risk of developing SBI (AOR = 1.734, 95% CI = 1.13-2.66), and 1298AC + CC genotypes were significantly associated with a 1.825-fold increased risk for SBI (AOR = 1.825, 95% CI = 1.20-2.78), whereas for the MTHFR 677C>T polymorphisms in SBI patients there were no statistically significant differences in the effects of the MTHFR genotypes on SBI between the patients and the controls (Table 2).
For the MTHFR 1298A>C polymorphisms, significant difference was found in terms of the risk for SBI in females (AC, AOR = 2.205, 95% CI = 1.11-3.70; AC + CC, AOR = 2.106, 95% CI = 1.16-3.83). When this population was separated into two age groups, 1298AC + CC genotypes showed a 1.789-fold increased risk for SBI in patients aged < 65 years, and this relationship showed statistical significance (AOR = 1.789; 95% CI = 1.05-3.05) (Table 3). In addition, when stratified by age of 55 years, genotype frequencies were significantly different for SBI in females and older than 55 years (in females, AC, AOR = 2.025, 95% CI = 1.11-3.70, AC + CC, AOR = 2.106, 95% CI = 1.16-3.83; in ≥ 55 years, AC, AOR = 1.987, 95% CI = 1.18-3.34, AC + CC, AOR = 2.088, 95% CI = 1.25-3.50). MTHFR 677C>T polymorphism in subgroup analysis of the SBI patients was not statistically significant such as genders or age groups (p > 0.05; data not shown).
As seen in Table 2, nine combinations are possible. However, no individual with 677CT/1298CC, 677TT/1298AC, and 677TT/1298CC was detected.32-34 The compound genotype of 677CC/1298AC showed a 2.689-fold increased risk for SBI (AOR=2.689, 95% CI = 1.26-5.76), and the compound genotype of 677CT/1298AC revealed a 2.604-fold increased risk for SBI (AOR = 2.604, 95% CI = 1.29-5.25). The 677TT/1298AA compound genotype was approximately 2.3 times more prone to developing SBI than the controls (AOR = 2.289; 95% CI = 1.19-4.42) (Table 2).
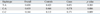
Four haplotypes are possible, but the 677T-1298C haplotype was not present in our patient population. When the cases of SBI were compared with the controls, there were significant differences in the distribution frequency between cases and controls for the 677C-1298A (p = 0.006) and 677C-1298C (p = 0.009) haplotypes (Table 4). The 677C-1298A haplotype showed a lower frequency in patients with SBI than in the controls. However, the 677C-1298C haplotype was more frequently observed in patients than in controls.
The tHcy levels were higher in patients with heterozygous 677CT and 677CT + TT genotypes compared to the corresponding control population. A statistically significant elevation of tHcy levels was observed for genotypes 1298AA, 1298AC, and 1298AC + CC. The tHcy levels were higher in patients with 1298CC than in the controls, but did not reach statistical significance due to the limited number of cases with this genotype. In combined genotypes, the tHcy levels were significantly higher in patients with 677CT/1298AC than in the controls, and 677TT/1298AA genotypes showed an increase in tHcy levels compared to controls, with marginal significance (Table 5).
Hyperhomocysteinemia is a well-known risk factor for vascular diseases, including stroke, and it has been suggested that this condition may be a risk factor for the development of SBI.8,9,12 The tHcy levels can potentially be elevated by either environmental (including diet) and/or genetic factors.
The common polymorphism in the MTHFR 677C>T can reduce enzyme activity, resulting in hyperhomocysteinemia, and can also increase the risks of cardiovascular diseases, certain types of cancer, and birth defects.31 The MTHFR 1298A>C polymorphism has also been found to reduce MTHFR enzyme activity, to a lesser extent than those with the 677C>T mutation, but conflicting results have been reported with respect to the association between 1298A>C polymorphism and tHcy levels. It has been reported that the MTHFR 1298A>C polymorphism may be associated with ischemic stroke, and may also play a protective role against colorectal cancer and acute lymphocytic leukemia.35
In this study, the tHcy levels were significantly higher in patients with MTHFR 677TT than in patients with other MTHFR 677C>T genotypes, while no correlation between tHcy and MTHFR 1298A>C genotypes was found. Recent studies have demonstrated that 1298A>C, in combination with 677C>T, may be associated with decreased MTHFR activity resulting in hyperhomocysteinemia, which is consistent with our results (Table 5).14,36-38 MTHFR 1298AC and MTHFR 1298AC + CC individuals were more prone to an increased risk for SBI than the corresponding controls, while the polymorphism of 677C>T at the MTHFR gene did not significantly influence the risk of SBI. When combined with the 1298A>C genotypes, however, we found that MTHFR 677C>T could have an additive effect on the variation at the MTHFR 1298A>C gene, because individuals carrying the predisposing variants (677CC/1298AC, 677CT/1298AC, 677TT/1298AA) at the two loci showed a higher risk of the development of SBI than any AOR individuals registered for MTHFR 1298A>C genotypes (Table 2).
Furthermore, we investigated the associations between SBI and allele haplotypes. The C-C haplotype increased the risk of SBI, whereas the C-A haplotype, a normal allele-combined haplotype, decreased the risk of the development of SBI. These results suggested that 1298A>C may be a more important genetic risk factor for SBI than 677C>T, and the MTHFR 1298C allele-containing haplotype may have the potential to be a predictive marker of the development of SBI in the Korean population.
However, the relationships between MTHFR polymorphisms and multifactorial diseases, especially cardiovascular disease and stroke, remain highly controversial, and genetic influences of MTHFR polymorphisms have not been observed in a number of populations. There was a racial difference in the frequency of the 1298C allele: Canadian, 0.36, French, 0.33, English, 0.32, German, 0.30, American, 0.29, South African, 0.21, Japanese, 0.19, Chinese, 0.17, Korean, 0.125, Korean, 0.178, and Korean, 0.163.25,28,32,36,37,39-42 From the literature, the MTHFR 1298C allele frequency was 0.125 to 0.178 in the Korean populations. The 1298CC genotype is present at a much lower frequency, at 1.4-3.7%, in Asian populations, compared to 7.2-12.6% in the Caucasian population; this information is consistent with our results.25,27-29,32,36,39 In the current study, the frequencies of the 1298AA, AC, and CC genotypes in the control group were 77.8%, 21.8%, and 0.4%, respectively. The corresponding frequencies in the patient group were 67.8%, 30.3%, and 1.9%, respectively. The frequency of the MTHFR 1298C allele was significantly higher in the SBI patients than in the controls. These findings indicate that there are ethnic variations in terms of the 1298A>C polymorphism, as well as a difference in the occurrence of SBI between the Asian population and the Caucasian population. It is conceivable that the contributions of MTHFR polymorphisms to SBI may vary in different ethnic groups.
In addition, no statistically significant difference in the risk for SBI was found between MTHFR genotypes in subjects over 65 years of age. We found that the 1298AC and 1298AC + CC genotypes showed an increased risk for SBI in patients under 65 years of age. SBI, a cerebrovascular disease, has an age-dependent nature. The causes of SBI are multifactorial, and additional environmental risk factors of SBI may develop with age. In this study, logistic regression, adjusting for possible confounders such as age, hypertension, and diabetes mellitus, showed a significant relationship between the 1298A>C polymorphism and early-onset SBI under 65 years of age. Prior to this study, Kohara, et al.2 reported that the MTHFR 677TT genotype is an independent risk factor for SBI and white matter lesions in the general Japanese population, especially in elderly subjects over 60 years of age. Since genetic polymorphisms often vary among ethnic groups or geographical areas, further studies are needed to clarify the association between MTHFR polymorphisms and SBI in diverse ethnic populations.
This study has limitations because it was conducted in a hospital-based population. The other possible limitations are related to exposure to different environmental factors, such as daily folate intake, additional genetic effects such as methionine synthase (MTR) and methionine synthase reductase (MTRR), and ethnic differences. Large, community-based random sampling is needed in order to resolve these limitations.
Despite these limitations, this study is unique in that it focused on the relationship between the MTHFR 1298A>C polymorphism and SBI in a Korean population. This study presents evidence that the 1298A>C polymorphism, but not the 677C>T polymorphism, acts as an independent risk factor for SBI, especially in patients under 65 years of age. In addition, it indicates that the polymorphisms of MTHFR 677C>T and 1298A>C interact additively, resulting in an increased risk of SBI in a Korean population.
Figures and Tables
Table 2
Comparison of Genotype Frequencies in the MTHFR 677C>T and 1298A>C Polymorphisms between Patients with Silent Brain Infarction (SBI) and Control Subjects
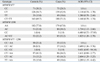
Table 3
Comparison of Genotype Frequencies in the MTHFR 1298A>C Polymorphism between Patients with Silent Brain Infarction (SBI) and Control Subjects, Stratified by Sex and Age
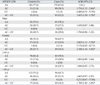
Table 4
Comparison of Haplotype Frequencies in the MTHFR 677C>T and 1298A>C Polymorphisms between Patients with Silent Brain Infarction (SBI) and Control Subjects
ACKNOWLEDGEMENTS
This work was partly supported by the Korea Research Foundation Grant, funded by the Korean Government (MOEHRD) (KRF-2008-521-E00121) and partly supported by a grant of the Healthcare Technology R & D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A084923).
References
1. Kobayashi S, Okada K, Yamashita K. Incidence of silent lacunar lesion in normal adults and its relation to cerebral blood flow and risk factors. Stroke. 1991. 22:1379–1383.

2. Kohara K, Fujisawa M, Ando F, Tabara Y, Niino N, Shimokata H. NILS-LSA Study. MTHFR gene polymorphism as a risk factor for silent brain infarcts and white matter lesions in the Japanese general population: The NILS-LSA Study. Stroke. 2003. 34:1130–1135.

3. Bernick C, Kuller L, Dulberg C, Longstreth WT Jr, Manolio T, Beauchamp N, et al. Silent MRI infarcts and the risk of future stroke: the cardiovascualr health study. Neurology. 2001. 57:1222–1229.
4. Kobayashi S, Okada K, Koide H, Bokura H, Yamaguchi S. Subcortical silent brain infarction as a risk factor for clinical stroke. Stroke. 1997. 28:1932–1939.

5. Uehara T, Tabuchi M, Mori E. Risk factors for silent cerebral infarcts in subcortical white matter and basal ganglia. Stroke. 1999. 30:378–382.

6. Szolnoki Z. Chemical events behind leukoaraiosis: medicinal chemistry offers new insight into a specific microcirculation disturbance in the brain (a chemical approach to a frequent cerebral phenotype). Curr Med Chem. 2007. 14:1027–1036.

7. Szolnoki Z. Pathomechanism of leukoaraiosis: a molecular bridge between the genetic, biochemical, and clinical processes (a mitochondrial hypothesis). Neuromolecular Med. 2007. 9:21–33.

8. Notsu Y, Nabika T, Park HY, Masuda J, Kobayashi S. Evaluation of genetic risk factors for silent brain infarction. Stroke. 1999. 30:1881–1886.

9. Boushey CJ, Beresford SA, Omenn GS, Motulsky AG. A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. Probable benefits of increasing folic acid intakes. JAMA. 1995. 274:1049–1057.
10. Kim NK, Choi BO, Jung WS, Choi YJ, Choi KG. Hyperhomocysteinemia as an independent risk factor for silent brain infarction. Neurology. 2003. 61:1595–1599.
11. Matsui T, Arai H, Yuzuriha T, Yao H, Miura M, Hashimoto S, et al. Elevated plasma homocysteine levels and risk of silent brain infarction in elderly people. Stroke. 2001. 32:1116–1119.

12. Vermeer SE, van Dijk EJ, Koudstaal PJ, Oudkerk M, Hofman A, Clarke R, et al. Homocysteine, silent brain infarcts, and white matter lesions: The Rotterdam Scan Study. Ann Neurol. 2002. 51:285–289.

13. Clarke R, Daly L, Robinson K, Naughten E, Cahalane S, Fowler B, et al. Hyperhomocysteinemia: an independent risk factor for vascular disease. N Engl J Med. 1991. 324:1149–1155.
14. Friedman G, Goldschmidt N, Friedlander Y, Ben-Yehuda A, Selhub J, Babaey S, et al. A common mutation A1298C in human methylenetetrahydrofolate reductase gene: association with plasma total homocysteine and folate concentrations. J Nutr. 1999. 129:1656–1661.

15. Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, et al. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet. 1995. 10:111–113.

16. Lievers KJ, Boers GH, Verhoef P, den Heijer M, Kluijtmans LA, van der Put NM, et al. A second common variant in the methylenetetrahydrofolate reductase (MTHFR) gene and its relationship to MTHFR enzyme activity, homocysteine, and cardiovascular disease risk. J Mol Med. 2001. 79:522–528.

17. van der Put NM, Gabreëls F, Stevens EM, Smeitink JA, Trijbels FJ, Eskes TK, et al. A second common mutation in the methylenetetrahydrofolate reductase gene: an additional risk factor for neural-tube defects? Am J Hum Genet. 1998. 62:1044–1051.
18. Choi BO, Kim NK, Kim SH, Kang MS, Lee S, Ahn JY, et al. Homozygous C677T mutation in the MTHFR gene as an independent risk factor for multiple small-artery occlusions. Thromb Res. 2003. 111:39–44.

19. Girelli D, Martinelli N, Pizzolo F, Friso S, Olivieri O, Stranieri C, et al. The interaction between MTHFR 677C-->T genotype and folate status is a determinant of coronary atherosclerosis risk. J Nutr. 2003. 133:1281–1285.

20. Heijmans BT, Boer JM, Suchiman HE, Cornelisse CJ, Westendorp RG, Kromhout D, et al. A common variant of the methylenetetrahydrofolate reductase gene (1p36) is associated with an increased risk of cancer. Cancer Res. 2003. 63:1249–1253.
21. Kim NK, Choi YK, Kang MS, Choi DH, Cha SH, An MO, et al. Influence of combined methylenetetrahydrofolate reductase (MTHFR) and thymidylate synthase enhancer region (TSER) polymorphisms to plasma homocysteine levels in Korean patients with recurrent spontaneous abortion. Thromb Res. 2006. 117:653–658.

22. Ko KH, Kim NK, Yim DJ, Hong SP, Park PW, Rim KS, et al. Polymorphisms of 5,10-methylenetetrahydrofolate reductase (MTHFR C677T) and thymidylate synthase enhancer region (TSER) as a risk factor of cholangiocarcinoma in a Korean population. Anticancer Res. 2006. 26:4229–4233.
23. Nelen WL, Blom HJ, Steegers EA, den Heijer M, Eskes TK. Hyperhomocysteinemia and recurrent early pregnancy loss: a meta-analysis. Fertil Steril. 2000. 74:1196–1199.

24. Ou CY, Stevenson RE, Brown VK, Schwartz CE, Allen WP, Khoury MJ, et al. 5,10 Methylenetetrahydrofolate reductase genetic polymorphism as a risk factor for neural tube defects. Am J Med Genet. 1996. 63:610–614.

25. Matsuo K, Suzuki R, Hamajima N, Ogura M, Kagami Y, Taji H, et al. Association between polymorphisms of folate-and methionine-metabolizing enzymes-and susceptibility to malignant lymphoma. Blood. 2001. 97:3205–3209.
26. Sazci A, Ergul E, Tuncer N, Akpinar G, Kara I. Methylenetetrahydrofolate reductase gene polymorphisms are associated with ischemic and hemorrhagic stroke: Dual effect of MTHFR polymorphisms C677T and A1298C. Brain Res Bull. 2006. 71:45–50.

27. Shen H, Xu Y, Zheng Y, Qian Y, Yu R, Qin Y, et al. Polymorphisms of 5,10-methylenetetrahydrofolate reductase and risk of gastric cancer in a Chinese population: a case-control study. Int J Cancer. 2001. 95:332–336.

28. Song C, Xing D, Tan W, Wei Q, Lin D. Methylenetetrahydrofolate reductase polymorphisms increase risk of esophageal squamous cell carcinoma in a Chinese population. Cancer Res. 2001. 61:3272–3275.
29. Stegmann K, Ziegler A, Ngo ET, Kohlschmidt N, Schröter B, Ermert A, et al. Linkage disequilibrium of MTHFR genotypes 677C/T-1298A/C in the German population and association studies in probands with neural tube defects (NTD). Am J Med Genet. 1999. 87:23–29.

30. van der Put NM, Gabreëls F, Stevens EM, Smeitink JA, Trijbels FJ, Eskeës TK, et al. A second common mutation in the methylenetetrahydrofolate reductase gene: an additional risk factor for neural-tube defects? Am J Hum Genet. 1998. 62:1044–1051.

31. Weisberg I, Tran P, Christensen B, Sibani S, Rozen R. A second genetic polymorphism in methylenetetrahydrofolate reductase (MTHFR) associated with decreased enzyme activity. Mol Genet Metab. 1998. 64:169–172.

32. Isotalo PA, Wells GA, Donnelly JG. Neonatal and fetal methyle-netetrahydrofolate reductase genetic polymorphisms: an examination of C677T and A1298C mutations. Am J Hum Genet. 2000. 67:986–990.

33. Zetterberg H, Regland B, Palmér M, Ricksten A, Palmqvist L, Rymo L, et al. Increased frequency of combined methylenetetrahydrofolate reductase C677T and A1298C mutated alleles in spontaneously aborted embryos. Eur J Hum Genet. 2002. 10:113–118.

34. Bae J, Shin SJ, Cha SH, Choi DH, Lee S, Kim NK. Prevalent genotypes of methylenetetrahydrofolate reductase (MTHFR C677T and A1298C) in spontaneously aborted embryos. Fertil Steril. 2007. 87:351–355.

35. Krajinovic M, Lamothe S, Labuda D, Lemieux-Blanchard E, Theoret Y, Moghrabi A, et al. Role of MTHFR genetic polymorphisms in the susceptibility to childhood acute lymphoblastic leukemia. Blood. 2004. 103:252–257.

36. Chango A, Potier De Courcy G, Boisson F, Guilland JC, Barbé F, Perrin MO, et al. 5,10-methylenetetrahydrofolate reductase common mutations, folate status and plasma homocysteine in healthy French adults of the Supplementation en Vitamines et Mineraux Antioxydants (SU.VI.MAX) cohort. Br J Nutr. 2000. 84:891–896.

37. Kim NK, Kang GD, Kim HJ, Kim SH, Nam YS, Lee S, et al. Genetic polymorphisms of 5,10-methylenetetrahydrofolate reductase (MTHFR C677T and A1298C) in healthy Korean. Korean J Genet. 2002. 24:227–234.
38. Kluijtmans LA, Young IS, Boreham CA, Murray L, McMaster D, McNulty H, et al. Genetic and nutritional factors contributing to hyperhomocysteinemia in young adults. Blood. 2003. 101:2483–2488.

39. Kim HN, Lee IK, Kim YK, Tran HT, Yang DH, Lee JJ, et al. Association between folate-metabolizing pathway polymorphism and non-Hodgkin lymphoma. Br J Haematol. 2008. 140:287–294.

40. Wiemels JL, Smith RN, Tayler GM, Eden OB, Alexander FE, Greaves MF. United Kingdom Childhood Cancer Study investigators. Methylenetetrahydrofolate reductase (MTHFR) polymorphisms and risk of molecularly defined subtypes of childhood acute leukemia. Proc Natl Acad Sci U S A. 2001. 98:4004–4009.

41. Gebhardt GS, Scholtz CL, Hillermann R, Odendaal HJ. Combined heterozygosity for methylenetetrahydrofolate reductase (MTHFR) mutations C677T and A1298C is associated with abruptio placentae but not with intrauterine growth restriction. Eur J Obstet Gynecol Reprod Biol. 2001. 97:174–177.

42. Kim JK, Kim S, Han JH, Kim HJ, Chong SY, Hong SP, et al. Polymorphisms of 5,10-methylenetetrahydrofolate reductase and risk of stomach cancer in a Korean population. Anticancer Res. 2005. 25:2249–2252.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download