Abstract
Purpose
The purpose of this study is to investigate the frequency and characteristics of migraine and seizure-related headache (SRH) according to the criteria of the International Headache Society.
Materials and Methods
A questionnaire was undertaken at the initial evaluation of newly referred patients from 32 epilepsy clinics.
Results
Of a total of 597 patients, 74 (12.4%) patients had migraine. Age at the onset of epilepsy was lower in patients with migraine than in those without. Twenty-six (4.4%), nine (1.5%), and 146 (24.5%) patients experienced prodromal, ictal, and postictal SRH, respectively (n = 169, 28.3%). A pain intensity of prodromal and postictal SRH was 6.1 ± 1.5 (SD) and 6.3 ± 1.9 (SD) on the visual analogue scale, and their duration was 12.6 ± 26.7 (SD) hours and 9.0 ± 17.4 (SD) hours, respectively. Age at the onset of epilepsy was lower in patients with SRH than in those without, and the risk of occurrence of SRH was significantly greater in patients with longer epilepsy duration. SRH could be classified as a type of migraine in 46.2% of patients with prodromal SRH and in 36.3% of patients with postictal SRH. Prodromal SRH occurred more frequently and was more likely to be a migraine-type in patients with migraine compared with those without. Postictal SRH occurred more frequently and was more likely to be a migraine-type in patients with migraine.
Migraine and epilepsy are both chronic neurological disorders characterized by recurrent attacks, which are often found as comorbid conditions. The comorbidity of migraine and epilepsy has been reported with the frequency of migraine in the epileptic population ranging from 8% to 15%.1 Headaches are often recognized as a part of symptoms of epileptic seizures. The characteristics of seizure-related headache (SRH) have been reported in many studies.2-12 However, only a few studies have been conducted on large patient populations (n > 300),3,8,11 and the influence of migraine on SRH has not been thoroughly investigated.2,5,8,11 We prospectively conducted a nationwide survey of migraine and SRH by using a questionnaire.
Five hundred and ninety-seven epileptic patients from 32 outpatient clinics (36 epileptologists) were investigated at their initial visit by using a questionnaire. Patients were ≥ 13 years of age and had experienced ≥ 2 seizures during the year prior to their first visit. Patients with seizures only during sleep, overt mental retardation, or impaired communication skills were excluded because these patients were unlikely to give reliable information regarding their headaches. A diagnosis of migraine was made in patients having interictal headaches that satisfy the criteria of the International Headache Society (IHS).13
The patients were given a questionnaire on SRH which addressed frequency, quality, lateralization, duration, severity, and accompanying symptoms. According to the timing of the headaches in relation to the seizure, SRH was classified as prodromal, ictal, and postictal headaches; prodromal SRH was regarded as a headache that had lasted for more than 10 minutes before the onset of overt seizure, ictal SRH was a headache that had occurred alone just before the onset of overt seizure or simultaneously with the other seizure manifestations, and postictal SRH was a headache that had begun immediately after cessation of the seizure. Prodromal SRH and postictal SRH were further classified into migraine-type by the IHS criteria, regardless of the number or duration of attacks, and non-migraine headaches were classified as other-type.
The pain intensity of SRH was determined by the patients on a visual analogue scale (VAS: 0, no pain; 10, strongest pain). The frequency of SRH associated with seizures was classified as: always (≥ 90% of seizures); frequent (50% to 89% of seizures); occasional (10% to 49% of seizures); and rare (< 10% of seizures). The classification of seizure and epilepsy, and the lobar classification of epileptogenic foci were based on ictal semiology, EEG, and neuroimaging findings.14,15
We used the Student's t-test to analyze continuous variables and the χ2 test or Fisher's exact test to examine categorical variables. The significance level was set at p < 0.05. The study was approved by the Institutional Review Board of Severance Hospital.
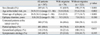
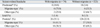
A total of 597 patients were enrolled (Table 1). Of these, 348 (58.3%) were men and 249 (41.7%) were women. Patients' ages ranged from 13 to 86 years, with a mean age (± SD) of 34.9 (± 15.1) years. The mean age (± SD) at the onset of epilepsy was 26.9 (± 16.1) years and the mean duration (± SD) of epilepsy was 8.0 (± 10.2) years. Symptomatic etiology was found in 243 (40.7%) patients. Three hundred and forty (57.0%) patients had not taken antiepileptic drugs (AEDs) at the time of their initial visit to the clinic. One hundred and sixteen (19.4%) patients had generalized epilepsy; 69.0% (n = 80), 25.0% (n = 29), and 6.0% (n = 7) of the patients were classified as having generalized tonic-clonic seizure (GTCS) only, juvenile myoclonic epilepsy, and absence epilepsy, respectively. Of those with partial epilepsy (n = 481, 80.6%), 3.1% (n = 15) had simple partial seizure (SPS) only, 17.5% (n = 84) had complex partial seizure (CPS) only, or SPS and CPS, and 79.4% (n = 382) had seizure types including secondarily GTCS. The percentage of patients diagnosed as frontal (FLE), temporal (TLE), parietal (PLE), and occipital (OLE) lobe epilepsies were 26.0% (n = 125), 32.6% (n = 157), 5.4% (n = 26), and 2.1% (n = 10), respectively, according to lobar classification. Lobar localization of the epileptogenic focus could not be determined in 33.9% (n = 163) of the patients (unspecified partial epilepsy: UPE). The distribution of secondarily GTCS differed significantly among lobar epilepsies (88.0% of FLE, 64.3% of TLE, 73.1% of PLE, 90.0% of OLE, and 87.7% of UPE; p < 0.001).
Seventy-four (12.4%) patients had migraine (without aura, 60; with aura, 14). Most of these patients (n = 73) had experienced at least one attack of migraine within 1 year before their initial visit. The mean age (± SD) at the onset of migraine was 21.4 (± 8.8) years, and the mean duration (± SD) of migraine was 9.4 (± 8.8) years. Migraine was more frequent in women, younger patients, and patients with younger age at the onset of epilepsy. The prevalence was similar between those with generalized and partial epilepsy (13.8% vs. 12.1%). The prevalence of migraine was similar between the patients with and without symptomatic etiology (10.3% vs. 13.8%) (Table 1). Migraine was found in 16.0% of FLE, 11.5% of TLE, 19.2% of PLE, 30.0% of OLE, and 7.4% of patients with UPE, which was statistically significant (p = 0.033).
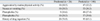
A total of 169 (28.3%) patients experienced SRH; 26 (4.4%), 9 (1.5%), and 146 (24.4%) patients had prodromal, ictal, and postictal SRH, respectively. Ten patients had both prodromal and postictal SRH and two patients had both ictal and postictal SRH. The description of the headache was consistent with migraine-type in 46.2% (n = 12) of patients with prodromal SRH and in 36.3% (n = 53) of patients with postictal SRH. Accompanying symptoms of SRH, such as aggravation by routine physical activity, nausea, vomiting, photophobia, and phonophobia, and a history of drug ingestion for relief of SRH were found in a significant number of patients and equally distributed among those with prodromal and postictal SRH (Table 2).
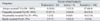
The pain intensity of prodromal, ictal, and postictal SRH was 6.1 (SD, 1.5; range, 4-10), 5.4 (SD, 2.5; range, 2.5-9.5), and 6.3 (SD, 1.9; range, 2-10) on the VAS, and their duration was 12.6 hours (SD, 26.7; range, 0.2-96), 157.2 seconds (SD, 152.2; range, 5-480), and 9.0 hours (SD, 17.4; range, 0.03-96), respectively. Postictal SRH always occurred in 66.4% of the patients, which was a significantly higher rate compared with 30.8% of patients with prodromal SRH and 33.3% of patients with ictal SRH (Table 3).
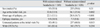
Age at the onset of epilepsy and age at the initial visit were lower in patients with SRH than in those without, and the risk of occurrence of SRH was significantly greater in patients with longer epilepsy duration. Patients without SRH had not been treated with AEDs more frequently compared to those with SRH at their initial visit. According to the seizure type, there was no significant difference in the frequency of overall SRH or postictal SRH between patients with GTCS (GTCS in generalized epilepsy, or seizure types including secondarily GTCS in partial epilepsy) and patients without GTCS (29.3% vs. 24.3%, p = 0.294; 25.9% vs. 18.3%, p = 0.085) (Table 4). In partial epilepsy, SRH was found in 13.3% of patients with SPS only, 26.2% of patients with CPS only or with SPS and CPS, and 28.3% of patients with seizure types including secondarily GTCS, which was not statistically significant (p = 0.488). Also, there was no significant difference in the frequency of postictal SRH (6.7%, 19.0%, and 24.9%; p = 0.172). According to the lobar classification, SRH occurred in 37.6% of FLE, 23.6% of TLE, 30.8% of PLE, 50.0% of OLE, and 21.5% of patients with UPE, which was statistically significant (p = 0.010). There was no significant difference in the frequency of postictal SRH among lobar epilepsies (31.2% of FLE, 20.4% of TLE, 19.2% of PLE, 40.0% of OLE, and 20.9% of UPE; p = 0.085). A significant relationship was not found between seizure type and the intensity or frequency (in association with seizure) of the SRH (data not shown).
Postictal SRH occurred more frequently (35.1% vs. 22.9%, p = 0.022) and was more likely to be a migraine-type (61.5% vs. 30.8%, p = 0.003) in patients with migraine compared to those without. Also, prodromal SRH occurred more frequently (10.8% vs. 3.4%; p = 0.009) and was more likely to be a migraine-type (75.0% vs. 33.3%, p = 0.090) in patients with migraine (Table 5).
Abundant clinical and epidemiologic data demonstrates that migraine and epilepsy are highly comorbid. Andermann and Andermann1 summarized a number of studies that investigated the association between migraine and epilepsy. The prevalence of epilepsy in persons with migraine ranged from 1% to 17% with a median of 5.9%, substantially higher than the population prevalence of epilepsy of 0.5%. Migraine prevalence in patients with epilepsy ranged from 8% to 15%. In an epidemiological study, the cumulative incidence of migraine by age 40 was 24% in probands with epilepsy, 23% in relatives with epilepsy, and 12% in relatives without epilepsy, which indicate that migraine and epilepsy are strongly associated.16 Several studies that were performed on a small number of epilepsy patients (n = 100 to 412) reported various results in the prevalence of migraine ranging from 8% to 20%.2,4,8,9,11,17-19 In this study, migraine was found in 12.4% of 597 patients, which is higher than the prevalence of 6.5% in the general Korean population (n = 1,523).20 The frequency of migraine with aura in the patients with migraine in this study was similar to that of the general Korean population with migraine (18.9% vs. 20.2%),20 which is in contrast with the study by Leniger, et al.19 showing that migraine with aura was significantly more frequent in patients with epilepsy and migraine compared with those with migraine alone. Ottman and Lipton16 reported that age at the onset of epilepsy was not a significant predictor of migraine, and Velioğlu, et al.21 reported that patients with epilepsy and migraine had a longer duration of epilepsy compared to those with epilepsy alone. In this study, the presence of migraine was associated with a younger age at the onset of epilepsy and at the initial visit, but not with a longer duration of epilepsy. Although our results suggest that epilepsy of earlier onset could increase the risk of migraine, further studies are required.
In this study, overall SRH occurred in 28% of all patients, which is lower than the frequency of 34% to 59% reported in previous studies.8,9,12 Also, the frequency of postictal SRH (24%) seems to be lower than the 23% to 52% reported in previous studies.2-12 This finding might be due to the inclusion of more patients with milder disease activity compared with other studies. In this study, 57% of all patients were untreated, and presumed to have drug-naive epilepsy. These patients were less likely to have SRH compared with those being treated for their epilepsy.
SRH, as well as seizures, significantly disturbs daily life. The pain intensity of SRH was 5.4 to 6.3 on average on the VAS, indicating a moderate to severe intensity. Moreover, prodromal and postictal SRH lasted 12.6 and 9.0 hours on average, respectively, and were accompanied by several annoying symptoms. The majority of patients with SRH had taken drugs for headache control. Among the patients with postictal SRH, 66% always experienced headaches in combination with their seizures, which was much more frequent compared to prodromal or ictal SRH. This agrees with the results reported by Leniger, et al.8 who observed a consistent appearance of SRH in 60% of the epilepsy patients with SRH.
The classification of SRH has been performed in previous studies. Fördereuther, et al.7 classified 34% of the patients with postictal SRH as having migraine headaches, and Ito, et al.11 observed migraine-like headaches in 26% of the patients with postictal SRH. Leniger, et al.8 reported that 56% of the patients with SRH experienced migraine-like headaches. Yankovsky, et al.12 reported that 36% of the patients with preictal headaches (prodromal and ictal SRH) and 48% of those with postictal headaches had migraine-like headaches. In this study, migraine-type (migraine-like) headaches were found in 46% and 36% of the patients with prodromal and postictal SRH, respectively. Also, it is interesting that the prevalence of migraine was significantly higher in patients with SRH and migraine-type SRH, which was in agreement with previous studies. Ito and Schachter5 found that postictal SRH occurred more frequently in patients with interictal headaches (presumed to be migraine in many cases), and Leniger, et al.8 and Ito, et al.11 reported a significant association between migraine-like SRH and migraine. Therefore, it is likely that there is a link between migraine, SRH, and migraine-like SRH. Although the mechanism of SRH is uncertain, the trigeminovascular system, which has been theorized to play a role in the pathogenesis of a migraine, may be activated by seizures.22
The presence of migraine and SRH seems to be related to the region of epileptogenic focus. In this study, determination of lobar epilepsy was often difficult to make on the outpatient basis, and might be affected by each investigator's bias. Also, the small number of patients with OLE (n = 10) may prohibit drawing any meaningful conclusion about the relationship between migraine or SRH, and OLE. However, the frequency of migraine and SRH seems to be higher in patients with OLE; 30% and 50% of patients with OLE had migraine and SRH, respectively, and four of the five patients with SRH had migraine-type headaches (data not shown in Results). A higher frequency of postictal headache and migraine-like postictal headache in OLE has been reported already.4,6,11 Cortical spreading depression is considered to be the mechanism of migraine aura, and characterized by transient increases in metabolic and electrical activity, and cerebral blood flow, followed by sustained decreases, spreading from the posterior to anterior cerebral area.23 Therefore, the occipital lobe could be the brain structure most responsible for the development of migraine. Migraine, SRH, and migraine-like SRH might be more likely to occur in association with OLE.
In conclusion, this study suggests that migraine is a frequent comorbidity in epilepsy patients and an important factor affecting the occurrence and character of SRH. This study also demonstrates that SRH is a frequent accompanying symptom of epileptic seizure, causing major impairment in daily life. The links between epilepsy, migraine, and SRH are an important subject for future investigation.
Figures and Tables
Appendix
APPENDIX
The HELP Study Group comprised the following members: Kyoung Heo, Byung In Lee, Severance Hospital, Seoul; Kyoon Huh, Ajou University Medical Centre, Suwon; Hyunwoo Nam, Boramae Medical Center, Seoul; Ok Joon Kim, Bundang CHA Hospital, Seongnam; Young-Min Shon, The Catholic University of Korea St. Mary's Hospital, Seoul; Hayoung Choi, Chonbuk National University Hospital, Chonju; Myeong-Kyu Kim, Chonnam National University Hospital, Gwangju; Hoo Won Kim, Chosun University Hospital, Gwangju; Sung-Hyun Lee, Chungbuk National University Hospital, Cheongju; Jae Moon Kim, Chungnam National University Hospital, Daejeon; Ji Eun Kim, Daegu Catholic University Medical Center, Daegu; Taewan Kim, Jangjoon Lee, Daegu Fatima Hospital, Daegu; Sang-Bong Lee, Daejeon St. Mary's Hospital, Daejeon; Sang Ho Kim, Dong-A University Hospital, Busan; Byung Kun Kim, Eulji General Hospital, Seoul; Gun-Sei Oh, Eulji University Hospital, Daejeon; Hyang Woon Lee, Ewha Womans University Mokdong Hospital, Seoul; Dong Jin Shin, Hyeonmi Park, Gachon Medical School Gil Medical Centre, Incheon; Juhan Kim, Hanyang University Hospital, Seoul; Sung Eun Kim, Inje University Busan Paik Hospital, Busan; Jeong Yeon Kim, Inje University Sanggye Paik Hospital, Seoul; Pil-Wook Chung, Kangbuk Samsung Hospital, Seoul; Hong-Ki Song, Kangdong Sacred Heart Hospital, Seoul; Sang Do Yi, Yong Won Cho, Keimyung University Dongsan Medical Centre, Daegu; Jin Yong Choi, Konkuk University Chungju Hospital, Chungju; Hyun Jeong Han, Kwandong University College of Medicine Myongji Hospital, Goyang; Jun Hong Lee, National Health Insurance Corporation Ilsan Hospital, Goyang; Sang Kun Lee, Seoul National University Hospital, Seoul; Kwang-Ik Yang, Soonchunhyang University Cheonan Hospital, Cheonan; Hyun-Young Park, Wonkwang University Hospital, Iksan; Se-Jin Lee, Yeungnam University Medical Center, Daegu; Won-Joo Kim, Gangnam Severance Hospital, Seoul.
References
1. Andermann E, Andermann FA. Andermann FA, Lugaresi E, editors. Migraine-epilepsy relationships: epidemiological and genetic aspects. Migraine and Epilepsy. 1987. Boston: Butterworths;281–291.
2. Schon F, Blau JN. Post-epileptic headache and migraine. J Neurol Neurosurg Psychiatry. 1987. 50:1148–1152.

3. Schachter SC, Richman K, Loder E, Beluk S. Self-reported characteristics of postictal headaches. J Epilepsy. 1995. 8:41–43.

4. Ito M, Nakamura F, Honma H, Takeda Y, Kobayashi R, Miyamoto T, et al. A comparison of post-ictal headache between patients with occipital lobe epilepsy and temporal lobe epilepsy. Seizure. 1999. 8:343–346.

5. Ito M, Schachter SC. Frequency and characteristics of interictal headaches in patients with epilepsy. J Epilepsy. 1996. 9:83–86.
6. Ito M, Nakamura F, Honma H, Takeda Y, Kobayashi R, Miyamoto T, et al. Clinical factors associated with post-ictal headache in patients with epilepsy. Acta Neurol Scand. 2000. 102:129–131.

7. Forderreuther S, Henkel A, Noachtar S, Straube A. Headache associated with epileptic seizures: epidemiology and clinical characteristics. Headache. 2002. 42:649–655.
8. Leniger T, Isbruch K, von den Driesch S, Diener HC, Hufnagel A. Seizure-associated headache in epilepsy. Epilepsia. 2001. 42:1176–1179.

9. Karaali-Savrun F, Goksan B, Yeni SN, Ertan S, Uzun N. Seizure-related headache in patients with epilepsy. Seizure. 2002. 11:67–69.
10. Ito M, Adachi N, Nakamura F, Koyama T, Okamura T, Kato M, et al. Multi-center study on post-ictal headache in patients with localization-related epilepsy. Psychiatry Clin Neurosci. 2003. 57:385–389.

11. Ito M, Adachi N, Nakamura F, Koyama T, Okamura T, Kato M, et al. Characteristics of postictal headache in patients with partial epilepsy. Cephalalgia. 2004. 24:23–28.
12. Yankovsky AE, Andermann F, Bernasconi A. Characteristics of headache associated with intractable partial epilepsy. Epilepsia. 2005. 46:1241–1245.
13. Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004. 24:Suppl 1. 9–160.
14. Proposal for revised clinical and electroencephalographic classification of epileptic seizures. From the Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia. 1981. 22:489–501.
15. Proposal for revised classification of epilepsies and epileptic syndromes. Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia. 1989. 30:389–399.
17. Marks DA, Ehrenberg BL. Migraine-related seizures in adults with epilepsy, with EEG correlation. Neurology. 1993. 43:2476–2483.

18. Velioğlu SK, Ozmenoğlu M. Migraine-related seizures in an epileptic population. Cephalalgia. 1999. 19:797–801.
19. Leniger T, von den Driesch S, Isbruch K, Diener HC, Hufnagel A. Clinical characteristics of patients with comorbidity of migraine and epilepsy. Headache. 2003. 43:672–677.
20. Lee TG, Chung KC, Choi JW. for the academic affairs committee of the Korean Headache Society. Prevalence of migraine in Korean adults: a nationwide survey. Korean J Headache. 2000. 1:57–66. [in Korean].
21. Velioğlu SK, Boz C, Ozmenoğlu M. The impact of migraine on epilepsy: a prospective prognosis study. Cephalalgia. 2005. 25:528–535.
22. Moskowitz MA, Buzzi MG, Sakas DE, Linnik MD. Pain mechanisms underlying vascular headaches. Progress Report 1989. Rev Neurol (Paris). 1989. 145:181–193.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download