Abstract
Natriuretic peptides (NPs) have been found to be useful markers in differentiating acute dyspneic patients presenting to the emergency department (ED) and emerged as potent prognostic markers for patients with congestive heart failure (CHF). The best-established and widely used clinical application of BNP and NT-proBNP testing is for the emergent diagnosis of CHF in patients presenting with acute dyspnea. Nevertheless, elevated NPs levels can be found in many circumstances involving left ventricular (LV) dysfunction or hypertrophy; right ventricular (RV) dysfunction secondary to pulmonary diseases; cardiac inflammatory or infectious diseases; endocrinology diseases and high output status without decreased LV ejection fraction. Even in the absence of significant clinical evidence of volume overload or LV dysfunction, markedly elevated NP levels can be found in patients with multiple comorbidities with a certain degree of prognostic value. Potential clinical applications of NPs are expanded accompanied by emerging reports regarding screening the presence of secondary cardiac dysfunction; monitoring the therapeutic responses, risk stratifications and providing prognostic values in many settings. Clinicians need to have expanded knowledge regarding the interpretation of elevated NPs levels and potential clinical applications of NPs. Clinicians should recognize that currently the only reasonable application for routine practice is limited to differentiation of acute dyspnea, rule-out-diagnostic-tests, monitoring of therapeutic responses and prognosis of acute or decompensated CHF. The rationales as well the potential applications of NPs in these settings are discussed in this review article.
Natriuretic peptides (NPs) have been found to be useful markers in differentiating acute dyspneic patients presenting to the emergency department (ED) and emerged as potent prognostic markers for patients with congestive heart failure (CHF). The best-established and widely used clinical application of BNP and NT-proBNP testing is for the emergent diagnosis of CHF in patients presenting with acute dyspnea. BNP and NT-proBNP, as the European Society of Cardiology recommended, are helpful in the diagnosis of HF and providing prognostic potential; as well at a low-normal concentration in untreated patients makes HF unlikely as the cause of symptoms.1 The Food and Drug Administration (FDA) approved a cutoff value of BNP for the diagnosis of CHF is 100 pg/mL. In NT-proBNP, the optimal cutoff values for confirmatory (rule in) decision limits for CHF are 450, 900 and 1,800 pg/mL for ages less than 50 years, between 50 to 75 years, and older than 75 years of age. The exclusionary (rule out) decision limit of NT-proBNP for cardiogenic acute dyspnea in all ages is less than 300 pg/mL.2 However, with the expanding clinical uses of NPs, many circumstances that directly or indirectly influence the heart functions have been found to associate with elevated NPs levels. Emerging reports have also suggested that the determination of NPs might be helpful in screening the presence of secondary cardiac dysfunction, monitoring the therapeutic responses, and providing prognostic values in many settings. Thus clinicians need to have expanded knowledge regarding the interpretation of elevated NPs levels and potential clinical applications of NPs.
In this review, we focus our discussion in current investigations on the interpretation and uses of elevated NPs levels in various non-CHF settings. The rationales as well the potential applications of NPs in these clinical settings are discussed.
Since 1956, Kisch found secretory granules in the guinea pig atrium; the heart is recognized not only as the pump of the circulatory system but also an endocrine organ.3,4 The secretory granule was determined to be atrial natriuretic peptide (ANP). Brain natriuretic peptide was identified from the porcine brain tissue initially and was found primarily synthesized from the ventricle. The name was subsequently changed to B-type natriuretic peptide (BNP). C-type natriuretic peptide (CNP) is produced by vascular endothelial cells and the kidney and is structurally similar to ANP and BNP.
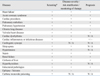
BNP can be produced in both atria and ventricles, and is upregulated in failing ventricular myocardium. In response to increased myocardial stretch and wall stress, ventricular myocytes secret the pro-hormone pre-proBNP, which is then cleaved into biologically active BNP and the inactive byproduct N-terminal-proBNP (NT-proBNP). The biological actions of NPs are mediated through membranebound natriuretic peptide receptors (NPR) that are linked to a cyclic guanosine monophosphate-dependent signaling cascade, including NPR-A, which preferentially binds ANP and BNP, and NPR-B, which preferentially binds CNP. Elevated BNP levels have been demonstrated to responsed to increased angiotensin II and sympathetic tones.5 Elevated NPs levels can be also found in many circumstances involving LV dysfunction or hypertrophy; right ventricular (RV) dysfunction secondary to pulmonary diseases; cardiac inflammatory or infectious diseases; and endocrinology diseases and high output status without decreased left ventricular ejection fraction (EF), e.g., sepsis, renal failure, cirrhosis of liver, or intracranial pathologies. Even in the absence of significant clinical evidence of volume overload or LV dysfunction, markedly elevated NP levels can be found in patients with multiple comorbidities with certain degree of prognostic value.6 The causes and mechanisms of elevated NPs levels are summarized in Fig. 1. The potential clinical applications in the non-HF settings are summarized in Table 1.
NPs induce vasodilatation, increase diuresis, and inhibit renin and aldosterone production. The function of CNP seems to be the regulation of regional blood flow. The net effects are decreasing cardiac preload and afterload. BNP is eliminated by binding to the NPR-C or degradation by neutral endopeptidase on endothelial cells, smooth muscle cells, cardiac myocytes, renal epithelium, and fibroblasts. NT-proBNP is cleared mainly by the kidney.7 BNP has a relatively shorter half-life of about 20 minutes; the half-life of NT-proBNP is about 60-90 minutes and would be expected to be longer in the setting of renal dysfunction. Obese patients (especially those who have body mass index greater than 30) tend to have lower BNP levels than others. Neural endopeptidases that can be secreted by adipose tissue may be related to increased BNP clearance in obese patients.8
During the past few years, several fully automated, rapid assays for the determinations of BNP and NT-proBNP have become commercially available, including both high-throughput automated plateforms and point-of care tests. Most immunoassays currently used in the clinical setting, however, do not determine precise molecular forms of these NPs, such as different cleavage points and post-translational modifications, which may vary depending on the pathophysiological state of CHF. In a recent study using quantitative mass spectral methodology, the authors reported the absence of circulating 32-amino acid BNP in advanced heart failure, suggesting the existence of altered forms of BNP that contribute to the high levels measured by conventional point-of-care tests.9 Plastic tubes containing ethylenedinitrolotetraacetic acid (EDTA) are desirable for BNP determination and refrigeration is required if the interval between blood collection and analysis is over 4 hours; whereas NT-proBNP can be measured in both serum or plasma, collected in glass or plastic tubes, and has no significant loss of immunoreactivity after 48 hours at room temperature. Although these existing BNP assays correlate closely, BNP assays are not currently analytical equivalent due to lack of assay standardization.10 A multicenter collaborative proficiency testing study conducted in 90 Italian laboratories had demonstrates that there are significant differences in analytical characteristics and measured values among the most popular commercial methods for BNP and NT-proBNP. Thus, clinicians should be very careful when comparing results obtained by laboratories that use different methods.11
Increased BNP levels correlate grossly with the severity of left ventricular (LV) dysfunction, both clinically and hemodynamically. It has been suggested that NT-proBNP levels also correlate and provide important prognostic information beyond echocardiographic parameters of cardiac structure and function.12 In 72 patients with various degrees of LV systolic dysfunction, a head-to-head comparison for performance of BNP and NT-proBNP to detect LV systolic dysfunction was performed. Similar to BNP, NT-proBNP is a promising marker in identifying LV systolic dysfunction. Although both assays are reliable and have good analytical performance, their diagnostic cut-off value is dynamic and population-dependent. The slightly wider detection range and the more stable structure of NT-proBNP compared to the BNP assay suggest that NT-proBNP could play an additional role in the evaluation of patients with LV systolic dysfunction.13
In a prospective observational study of 100 patients presenting with chest pain, Brown, et al. had reported that mean BNP levels in patients with cardiac chest pain was significantly greater than that for patients with non-cardiac chest pain. Comparing to cardiac troponin (cTn) T, BNP was less specific for myocardial injury, but more sensitive for the detection of acute cardiac chest pain. Combining BNP and cTn T significantly increased the sensitivity from 55.6% to 95.6% in detecting cardiac chest pain and was also a satisfactory rule out test (negative predictive value, NPV of 96%) for excluding chest pain that had a cardiac origin.14 Anemia (Hb < 12 g/dL for females; < 13 g/dL for males) was also associated with elevated NPs levels in patients with known or suspected coronary artery disease.15 NT-proBNP is also a sensitive marker of myocardial ischemia that rises much higher in the earlier phase compared with conventional markers of myocardial damage, especially in non-ST elevation -MI patients.16
In patients with ACS, BNP is a powerful indicator of acute HF.17 In a prospective study involving 74 patients with ST elevation MI, increased BNP levels are associated with progressive ventricular dilatation and development of clinical heart failure and powerful markers of LV systolic dysfunction as well poor prognosis after MI.18 In a study following 276 patients presented to the emergency department with chest pain for 90 days, baseline elevated BNP and NT-proBNP levels were predictive of adverse events, i.e., ED re-visiting for chest pain, cardiac readmission, and death at 30 and 90 days.19 Besides, BNP levels were significantly higher in patients with multivessels than those with only single-vessel diseases.20 Multivariate logistic regression analysis incorporating age, gender, history of hypertension, diabetes, LVEF, cTn I, and therapeutic regimens indicated that BNP was an independent predictor of cardiac death in ACS patients.21 In an outpatient follow-up study, ACS patients who had newly elevated BNP levels at 4 months were at increased risk of death or newly developed HF. Patients with elevated BNP levels at study entry and with BNP levels lower than 80 pg/mL at 4 months tended to have only modestly increased risk compared to patients with BNP levels lower than 80 pg/mL at both visits. Patients with BNP levels of more than 840 pg/mL and increased cTn levels are at a particularly high risk for mortality.22 In addition to Thrombolysis In Myocardial Infarction (TIMI) risk score, multi-marker risk approach based on cTnT, C-reactive protein (CRP), and NT-proBNP was associated with adverse events at 6 months.23 Changes in BNP levels over time were associated with long-term clinical outcomes.24
BNP levels obtained at post-PCI 24th hour were independent predictors of major adverse cardiac events (MACE), including cardiac death, MI, hospitalization with angina or repeat revascularization during 12 months of follow-up after elective successful PCI.25 In 26 patients that received the implantation of a paclitaxel-eluting stent, symptomatic re-stenosis after implantation of a paclitaxel-eluting stent could be predicted by the combination of a basal plasma BNP level of more than 50 pg/mL and a positive or inconclusive conventional exercise test. Thus, determining basal BNP levels could improve both the detection and exclusion of asymptomatic re-stenosis.26 In 135 patients undergoing various cardiac procedures, serum NT-proBNP is a good predictor for complications after cardiac surgery, is as good as the European system for cardiac operative risk evaluation, and better than EF alone.27 In 85 patients undergoing first-time elective CABG, preoperative BNP levels could be used to predict the development of postoperative new-onset atrial fibrillation (AFib), a need for inotropic support, and a requirement for intra-aortic balloon pump.28 In 149 that patients underwent cardiac surgery, BNP levels measured at the beginning of the rehabilitation program had been found to be independent predictors of late AFib after cardiac surgery.29
Despite the absence of a ventricular stretch or intracardiac pressure derangement, elevated BNP levels were found after cardiac transplantation; thus it had been implicated as a marker for allograft rejection, adverse prognosis, and coronary graft vasculopathy in these patients.30 BNP levels have high sensitivity and NPV for acute rejection in pediatric heart transplant patients. In 86 that patients underwent a total of 560 endomyocardial biopsies in patients > 1 year post-transplant, a BNP level of < 100 pg/mL correlated with a < 1% chance of aortic regurgitation (AR) and may obviate the need for biopsies in some cases.31 In an observational study that included 71 heart transplant patients, the increase between the two serial determinations of BNP levels at the end of the first year post-transplant indicated a subgroup of patients with a poorer outcome.32
In 19 children supported with a pulsatile ventricular assist device, extremely high levels of NPs reflect the severity of myocardial failure before extracorporeal membrane oxygenation implantation. During mechanical support, the decline of NPs appears to be an additional tool in the preselection of potential weaning candidates.33
NPs levels are elevated in most patients with acute PE complicated with RV overload or dysfunction.34 In 93 consecutive outpatients diagnosed with acute PE by means of helical computed tomography (CT), plasma levels of NT-proBNP greater than 500 ng/L were independently associated with central PE (in the main trunk or right or left main branches of the pulmonary artery) and perhaps as a predictor of death.35 The presence of RV dysfunction should be strongly considered in patients with plasma BNP levels of more than 90 pg/mL.36 BNP levels significantly associated with the severity of pulmonary hypertension and increased ventilation-perfusion mismatch on scintigraphy also corresponded to incremental increases in the levels of ANP and BNP. The combination of NT-proBNP or cTn tests to echocardiography could aid risk stratification in patients with acute PE.37
An aggressive therapy such as thrombolytic therapy may be beneficial in patients with acute massive or non-massive PE with RV dysfunction. Thrombolysis significantly reduced systolic pulmonary pressure, and declined BNP and cTn I levels were indicators of the efficacy of pharmacological treatment in patients with acute PE.38 After pulmonary thromboendarterectomy, plasma BNP levels markedly decreased in association with a reduction of total pulmonary resistance in survivors. The changes of plasma BNP levels were closely correlated with the total pulmonary resistance. Sustained elevated plasma BNP levels indicated the presence of residual pulmonary hypertension after operation. In hemodynamically stable PE, BNP/cTnI measurement could be helpful on admission, especially for ruling out circulatory failure and in-hospital death.39
In patients with RV pressure overload due to primary pulmonary hypertension (PPH) and thromboembolism, plasma BNP levels correlated with mean pulmonary artery pressure, right atrial pressure, RV end-diastolic pressure, and total pulmonary resistance.40 In 49 dyspneic patients (25 with chronic obstructive pulmonary disease (COPD), 8 with interstitial pneumonia, 16 with sequelae of tuberculosis), hypoxemia was more severe in patients with higher BNP levels than those with lower BNP levels.41 In a study involving 61 patients with various forms of chronic pulmonary hypertension, plasma NT-proBNP levels can be used to determine the clinical severity and are independently associated with long-term mortality.42
Elevated BNP levels have been found in hypoxemic patients with COPD, particularly in patients with cor pulmonale when compared with patients with COPD alone. BNP levels increased in proportion to the severity of RV dysfunction and could be a useful indicator of RV dysfunction.43 Adding mild diuretics to the standard treatment for an acute exacerbation (AE) of COPD may rapidly reduce plasma BNP levels in COPD patients with AE who have elevated BNP levels without any clinical evidence of cor pulmonale.44 In 208 patients presenting to the ED with an AE of COPD, BNP levels were significantly elevated during AE compared to recovery. In these patients, BNP levels independently predict the need for intensive care unit (ICU). However, BNP levels failed to predict short- and long-term mortality in these patients.45
Cardiovascular dysfunction is responsible for a majority of weaning failure. In 52 patients recovering from acute respiratory failure, the extubation failure group had significantly greater increases in BNP levels at the end of spontaneous breathing trial (SBT) than the extubation success groups. Thus, measuring the percentage change in the BNP levels during a SBT may help to improve the predictive value of SBT on weaning outcomes.46
Natriuretic peptides levels increase with increasing severity of mitral regurgitation (MR) and had been shown to be a marker of poor outcome in patients with organic MR.47
NT-proBNP levels were significantly greater in patients with severe mitral stenosis (MS) than in moderate MS. NT-proBNP levels were also significantly higher in patients with mitral valve replacement than in controls. There were positive correlations between BNP level with the degree of MS, pulmonary artery pressure, and a negative correlation with mitral valve area.48 Serum NT-proBNP levels correlated well with echocardiographic findings and functional class in patients with MS.49
In Patients < 70 years old with mild to moderate aortic stenosis (AS) with a peak transaortic gradient > 20 mm Hg, NT-proBNP levels increased even in asymptomatic patients with AS and correlated with echocardiographic parameters related to the severity of AS and degree of diastolic dysfunction.50 Preoperative NT-proBNP correlated significantly with diastolic and systolic LV wall stress assessed by echocardiography. Independent to preoperative LV mass index, higher pre-operative levels of NT-proBNP predicted a greater magnitude of total LV mass regression at follow-up.51
NPs could be used as an additional noninvasive method in monitoring disease progression and have potential prognostic usefulness in adjunct to echocardiography. In high-risk patients, BNP has been also considered to be useful for monitoring the progression of VHD.52 Detection of a cardiac murmur during routine medical examinations of hospitalized patients is associated with increased risk of death within a year. Determining NT-proBNP gives significant additional prognostic information of a murmur and could obviate the need for echocardiography in selected patients with a murmur and normal NT-proBNP for whom surgery is not feasible.53
In 60 patients with persistent AFib evaluated before cardioversion and 1, 30 and 180 days after cardioversion, a medium-low elevation of NT-proBNP indicated only an acute response to the distension of the atrial tissue induced by the arrhythmia; in contrast, markedly elevated values might be caused by ventricular dysfunction or hypertrophy. AFib may cause enduringly elevated ANP and BNP level. Changes in left atria (LA) volume correlated well with the changes in ANP and BNP levels following cardioversion; and atrial volume seems to be an important determinant of ANP and BNP in AFib.54 In 43 patients undergoing persistent/permanent AFib ablation, sinus rhythm (SR) following persistent/permanent AFib ablation is associated with a dramatic decrease in NPs with significantly improved cardiac functions, even after relatively extensive atrial ablation.55 Plasma NT-proBNP levels obtained before electrical cardioversion did neither predict cardioversion success nor relapse of AFib in patients without HF. However, maintained SR during follow-up was associated with a significant reduction in NT-proBNP levels.56 Significant reduction in BNP levels after pulmonary vein isolation was associated with therapeutic responses to antiarrhythmic drug therapy in patients with recurrent AFib after the procedure.57 In a study including 20 open-heart surgery patients with concomitant AFib, NPs levels tended to decrease in patients with stable SR at one year compared to patients in AFib.58 In 105 patients presented to the ED with a recent-onset AFib and supraventricular tachycardia, SR was restored in a low percentage of patients with NT-proBNP of greater than 4,500 pg/mL, while the vast majority of those with values < 1,500 pg/mL was normalized even by means of antiarrhythmic drugs alone. The evaluation of NT-proBNP could be used as an alternative to echocardiography to rapidly select patients in whom cardioversion should be attempted in the ED.59
High degree atrioventricular block can induce elevated plasma BNP levels and the atrioventricular dyssynchrony further induce elevated BNP levels. In 34 patients with preserved LV systolic function on permanent RV apical pacing, RV apical pacing is associated with LV dyssynchrony and subsequent accelerated BNP secretion.60 In a study involving 43 children and adolescents with high-grade second degree or complete atrioventricular conduction block, plasma BNP levels were significantly higher in patients without pacemaker than in those with permanent pacemaker. Additionally, patients with dual-chamber pacing had significantly lower BNP values compared to those with single chamber ventricular pacing.61
Increased release of BNP into the circulation may be a general feature of cardiac inflammation or injury. Inflammatory process can contribute specific cytokines leading to the disregulation of cardiac ANP and BNP production observed during myocardial inflammation and this process might be angiotensin receptor 1-dependent.62 In 14 patients with suspected acute perimyocarditis, BNP level are increased in some patients with acute perimyocarditis. BNP elevation is probably associated with hemodynamical stress caused by transient contractility abnormalities.63 In 45 patients with confirmed infective endocarditis, admission NT-proBNP levels of more than 1,500 pg/mL had significantly lower event-free survival than others. The combination of admission NT-proBNP and cTnI levels appeared to have even greater value for risk stratification in these patients.64 In a prospective study involving 45 patients with acute and convalescent rheumatic fever, BNP levels were higher compared to those of healthy subjects and could be used as a complementary tool in the treatment and prognosis of acute rheumatic fever.65 In 13 pediatric patients with Kawasaki disease, NT-proBNP levels increased in the acute phase and decreased significantly in the convalescent phase.66
Restrictive cardiomyopathy (RCM) and constrictive pericarditis (CP) are difficult to distinguish clinically and pose a diagnostic challenge. In 11 patients suspected of having either CP or RCM suffered New York Heart Association (NYHA) stage III-IV CHF with similar elevation in intracardiac pressures, BNP levels were markedly elevated in 5 patients with RCM than 6 patients with CP.67 In addition, patients with idiopathic CP had significantly lower levels of BNP than those with RCM and those with CP secondary to radiation and cardiac surgery.68
In 61 patients admitted to a university hospital due to syncope, NT-proBNP at a cut-off of 164 pg/mL identified patients with cardiac syncope and patients requiring interventional therapy with high sensitivity and NPV. Assessment of NT-proBNP might be helpful in differentiating cardiac from non-cardiac syncope and could effectively reduce the use of Holter echocardiography, telemetry monitoring, stress tests, echocardiography, coronary angiographies, and electrophysiological examinations in syncopal patients.69
Cardiac structural and functional abnormalities were observed with increased severity of sleep apnea. In 235 patients evaluated in a sleep clinic for obstructive sleep apnea, elevated BNP levels seemed to reflect an increased likelihood of LV hypertrophy in patients with severe sleep apnea.70 In a cross-sectional study involving 110 morbid obesity, healthy young female patients, NT-proBNP levels were independently predicted by sleep-disordered breathing and insulin resistance.71
In 154 untreated hypertensive patients without heart failure or AFib, logarithmic BNP was positively correlated with age, pulse pressure, cardiac hypertrophy, and diastolic dysfunction, and negatively correlated with hemoglobin, renin levels, and E/A ratio. Thus BNP might be useful in initial assessment of the severity of essential hypertension and may be also valuable for risk stratification.72
Both acute aortic dissection (AAD) and chronic aneurysms of the ascending aorta were associated with long-standing hypertension, which is often accompanied by LV diastolic dysfunction and AR. In 18 patients with AAD, both patients with AAD and chronic uncomplicated aneurysms had significant higher BNP levels than normal controls.73
Although clinical and echocardiographic signs define hemodynamic significance of patent ductus arteriosus (PDA), they are not predictive of the need for PDA intervention in the first days of life. In a prospective blinded study involving 67 preterm infants on the second day of life, plasma BNP levels positively correlated with ductal size and LA/Aortaratio significantly.74 Plasma NT-proBNP levels on day 3 are a good marker for hemodynamic significant PDA in preterm infants. Serial measurements of NT-proBNP may be useful in assessing the clinical course of PDA.75
In a study evaluating heart involvement in 152 patients with amyloidosis, NT-proBNP is a sensitive marker of cardiac dysfunction and a strong predictor of outcome in cardiac amyloidosis and had been shown to decline with treatment.76
Ventricular dysfunction with reduced EF and biventricular dilatation is present in most patients with severe sepsis and septic shock. Plasma ANP, NT-proBNP, and BNP were significantly elevated in septic shock patients than healthy control subjects. In a study involving 54 patients without heart diseases, BNP levels could be elevated in the acute phase of community-acquired microbial infections, particularly in patients with diabetes mellitus (DM) and lower respiratory tract infection, even in the absence of severe sepsis or septic shock.77 In a study involving 50 patients with septic shock, elevated BNP levels were significantly associated with myocardial dysfunction and severity of global tissue hypoxia. BNP levels were positively correlated with CRP levels in septic patients without clinical or echocardiographic evidence of volume overload or systolic dysfunction.78 In patients with community-acquired pneumonia (CAP), BNP level was an independent predictor of treatment failure and death. In a study evaluating 302 consecutive patients presenting to the ED with CAP, when used in conjunction with the pneumonia severity index (PSI), BNP levels significantly improved the risk prediction when compared with the PSI alone.79 Patients with septic shock had significantly higher BNP levels on admission compared to patients with early sepsis and healthy subjects. BNP levels for patients with septic shock were positively correlated with Sequential Organ Failure Assessment scores and prognosticated survival.80 NT-proBNP is an independent prognostic marker of mortality in severe sepsis and both NT-proBNP obtained on admission and 72-hours after admission are significantly higher in nonsurvivors than survivors.81
In a study involving 164 hemodialysis patients, elevated BNP levels were associated with volume overload, LV hypertrophy, cardiovascular disease and DM, and may be a useful parameter for assessing the risk of cardiac death in these patients.82 Renal function clearly influences the diagnostic performance of NT-proBNP; Goei, et al. had showed that NT-proBNP had more favorable discriminative value in patients with glomerular filtration rate (GFR) more than 90 mL/min/1.73 m2 and lost its prognostic value in patients with GFR less than 30 mL/min/1.73 m2.83 Unlike NT-proBNP, BNP levels are relatively independent of GFR. BNP may therefore be the more appropriate biomarker to screen for cardiac dysfunction in patients with renal failure.84 BNP levels could be a valuable tool for risk stratification of hemodialysis patients by confining echocardiographic studies to only patients with BNP levels above the established cutoff values.85
On the basis of the German Diabetes and Dialysis Study which evaluated atorvastatin in 1255 type 2 DM hemodialysis patients with a median follow-up of 4 years, patients with baseline NT-proBNP of more than 9,252 pg/mL exhibited a more than four-fold risk of stroke and a more than two-fold risk of sudden death, cardiovascular events, and mortality compared with patients with baseline NT-proBNP less than 1,433 pg/mL. Doubling of NT-proBNP increased the risk of death by 46%.86
In patients with cirrhosis of the liver, elevated proBNP and BNP levels reflect increased cardiac ventricular generation of NPs and thus indicates the presence of cardiac dysfunction. Hyperdynamic systemic circulation could also be contributed to elevated NPs levels in patients with cirrhosis of liver. In a study evaluating 52 non-alcoholic cirrhotic patients, BNP levels were significantly higher in cirrhotic patients complicated with ascites, spontaneous bacterial peritonitis and hepatic encephalopathy history, but no significant differences were observed for the presence of esophageal varices and bleeding history. BNP levels significantly correlated with Child score, interventricular septal thickness, and LV posterior wall thickness.87 In 51 cirrhotic patients during a hemodynamic investigation, circulating proBNP and BNP levels were related to the severity of liver decompensation (Child score, serum albumin, coagulation factors, and hepatic venous pressure gradient) and to markers of cardiac dysfunction (QT interval, heart rate, plasma volume).88
Assessing cardiac filling pressure and cardiac performance are important in patients with either noncardiogenic or cardiogenic shock. Low NT-proBNP values may be useful in excluding the need for pulmonary artery catheter placement in patients with ICU shock and identified those at lower risk for death.89 In a prospective, blinded cohort study that incorporated 54 patients admitted to the ICUs with respiratory distress, bilateral pulmonary edema and a central venous catheter suggesting either high-pressure (cardiogenic) or low-pressure, acute lung injury acute respiratory distress syndrome (ALI/ARDS) pulmonary edema, BNP at an accepted cutoff of 100 pg/mL had a high specificity for the diagnosis of ALI/ARDS (95.2%), but the sensitivity was poor (27.3%). BNP levels drawn within 48 hours of admission to the ICU did not correlate with invasive hemodynamic measurements and did not track predictably with changes in volume status on consecutive daily measurements.90 Patients with significant blood loss (decreased hemoglobin level more than 3 g/dL) had significant lower BNP levels than those without blood loss. Thus, BNP levels below normal are indicative of intravascular volume loss in traumatically injured patients.91 In a study evaluating 40 patients who had pre- and post transfusion NT-proBNP determinations, NT-proBNP could also be used to evaluate the development of transfusion associated circulatory overload with a sensitivity of 93.8% and specificity of 83.8%. Elevated post transfusion NT-proBNP is the only independent variable for this diagnosis.92 NT-proBNP on admission is an independent prognostic marker of outcome in an unselected cohort of critically ill patients. Measurement of NT-proBNP might facilitate triage of critical ED and ICU patients.93
Serum NT-proBNP levels are affected by thyroid functions and seem to be a direct stimulatory effect of thyroid hormones.94 A comparison between 67 patients with clinical hyperthyroidism and normal subjects, elevated BNP levels were mainly found in hyperthyroid patients who had clinical and echocardiographic evidence of LV dysfunction (increased LA diameter and decreased LVEF) but not in those with normal LV function and normal subjects.95 Multiple linear regression analysis demonstrated that free T4 and free T3 were independently associated with a high serum NT-proBNP, whereas cardiac output and resting pulse rate were not. In 21 patients with hyperthyroidism, both NT-proBNP and BNP levels were higher than hypothyroid patients and normal controls; and treatment of thyroid dysfunctions could result in normalization of NT-proBNP levels in both hypothyroid and hyperthyroid groups.96
A stress response consisting of elevated levels of cortisol and catecholamines is common after acute ischemic stroke (AIS). Activation of the hypothalamus-pituitary-adrenal axis in patients with AIS is associated with elevated levels of NPs.97 NT-proBNP levels were elevated in patients with AIS. In a study involving 30 patients with an AIS, the activated neurohumoral responses occurring in patients with AIS reflect either a counterbalancing vasodilating response to the cerebral ischemia or direct myocardial dysfunction.98 The log NT-proBNP correlated positively with cTnI and heart rate, and negatively with LVEF; and patients with signs of marked myocardial ischemia or insular cortex involvement had particularly higher NT-proBNP levels. BNP levels in AIS patients without AFib were correlated with MAP on admission or the degree of reduction in MAP at day 1. While in AIS patients with AFib, BNP levels showed a negative correlation with MAP on admission.99 Even in patients without AFib, the presence of at least one LA or appendage abnormality (atrial dilatation, low flow velocity, spontaneous echocontrast, or thrombus) had the strongest association with an elevated BNP, suggesting that BNP level could be a potential marker for the presence of LA sources of emboli.100 In a study involving 707 patients presenting to the ED with AIS, BNP of more than 76 pg/mL was an independent predictor of cardioembolic stroke. Even among patients with transient symptoms, a high BNP level identified cardioembolic etiology.101 Elevated NPs and cortisol levels predict long-term mortality after AIS, suggesting that this profound neurohumoral disturbance is prognostically unfavorable.102
Cardiovascular abnormalities are independent predictors of in-patient mortality after a subarachnoid hemorrhage (SAH). Patients with SAH showed an increased urine output and urinary excretion of sodium as well as higher BNP levels than the controls.103,104 In a study involving 50 patients with traumatic SAH, early after SAH, elevated BNP levels are associated with myocardial necrosis, pulmonary edema, and LV dysfunction. BNP levels may be elevated in patients with head injuries without echocardiographic evidence of HF.105 In the absence of evidence for activation of NPs within the brain, prompt and consistent increase in both ANP and BNP strongly supports the view that the heart is the source of increased NPs release after acute SAH.106 In a study involving 30 patients with severe isolated head injury, BNP levels are elevated shortly after head injury and progressively elevated through days 7-8 after the event in patients with diffused SAH as compared to patients with mild or no SAH; and in patients with elevated intracranial pressure (ICP) as compared to patients without elevated ICP as well as a poorer outcome.107 In a study involving 14 patients suffering from severe traumatic brain injury, NT-proBNP levels in cerebral spinal fluid and serum were significantly elevated in patients exhibiting an ICP of more than 15 mmHg.108 In a prospective cohort study incorporating 300 patients with aneurysmal SAH, an initial BNP level greater than 600 pg/mL was markedly associated with death.109
In a study incorporating 65 postictal children and 31 children with epilepsy after a seizure-free period for at least 2 months serving as controls, NT-proBNP levels were significantly higher 4 hours after a seizure attack compared to 24-48 hours after a seizure attack. Serum NT-proBNP levels were higher in children with tonic-clonic seizures and febrile convulsions than those with partial motor seizures, syncope, or normal subjects.110 Obi, et al. had reported a patient who had episodic elevation of ANP and BNP during epileptic activity caused by a left frontotemporal lesion. ANP and BNP were assumed to release from the heart by the epileptic stimulation on the anterior ventral region of the third ventricle.111
The level of NT-proBNP and carbon monoxide (CO) Hb were increased in patients with CO poisoning. In a study involving 15 patient with CO poisoning, there was a positive correlation between the levels of COHb and NT-proBNP. Thus, determining plasma NT-proBNP levels may contribute to the early diagnosis of cardiotoxicity in patients with CO poisoning.112
Elevated NPs levels have shown predictive value in various diseases that have direct or indirect influences on the heart functions in many non-HF circumstances, even in the absence of depressed cardiac function. It should be noted that NPs should never be interpreted without thorough clinical messages. NPs are very sensitive for primary or secondary cardiac dysfunction, but the specificity is low. Potential clinical applications of NPs are expanded, accompanied by emerging reports regarding to screening for the presence of secondary cardiac dysfunction, monitoring the therapeutic responses, risk stratifications, or providing prognostic values in many settings. Clinical decision on timely and costly cardiac examinations or more risky and invasive procedures rather than deferred, conservative strategies might be facilitated by appropriate use and interpretation of NPs. However, clinicians should recognize that currently the only reasonable application for routine practice is limited to differentiation of acute dyspnea, ruleout-diagnostic-tests (high NPV and low positive predictive values), monitoring of therapeutic responses, and prognosis of acute or decompensated CHF.
Figures and Tables
References
1. Swedberg K, Cleland J, Dargie H, Drexler H, Follath F, Komajda M, et al. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): The Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology. Eur Heart J. 2005. 26:1115–1140.

2. Januzzi JL, van Kimmenade R, Lainchbury J, Bayes-Genis A, Ordonez-Llanos J, Santalo-Bel M, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study. Eur Heart J. 2006. 27:330–337.

3. Kisch B. Electron microscopy of the atrium of the heart. I. Guinea pig. Exp Med Surg. 1956. 14:99–112.
4. De Bold AJ. Heart atria granularity effects of changes in water-electrolyte balance. Proc Soc Exp Biol Med. 1979. 161:508–511.
5. Iwanaga Y, Nishi I, Furuichi S, Noguchi T, Sase K, Kihara Y, et al. B-type natriuretic peptide strongly reflects diastolic wall stress in patients with chronic heart failure: comparison between systolic and diastolic heart failure. J Am Coll Cardiol. 2006. 47:742–748.
6. Burjonroppa SC, Tong AT, Xiao LC, Johnson MM, Yusuf SW, Lenihan DJ. Cancer patients with markedly elevated B-type natriuretic peptide may not have volume overload. Am J Clin Oncol. 2007. 30:287–293.

7. Schrier RW, Abraham WT. Hormones and hemodynamics in heart failure. N Engl J Med. 1999. 341:577–585.

8. Young JB, Correia NG, Francis GS, Maisel A, Michota F. Testing for B-type natriuretic peptide in the diagnosis and assessment of heart failure: what are the nuances? Cleve Clin J Med. 2004. 71:Suppl 5. S1–S17.
9. Hawkridge AM, Heublein DM, Bergen HR 3rd, Cataliotti A, Burnett JC Jr, Muddiman DC. Quantitative mass spectral evidence for the absence of circulating brain natriuretic peptide (BNP-32) in severe human heart failure. Proc Natl Acad Sci U S A. 2005. 102:17442–17447.
10. Omland T. Advances in congestive heart failure management in the intensive care unit: B-type natriuretic peptides in evaluation of acute heart failure. Crit Care Med. 2008. 36:S17–S27.

11. Prontera C, Zaninotto M, Giovannini S, Zucchelli GC, Pilo A, Sciacovelli L, et al. Proficiency testing project for brain natriuretic peptide (BNP) and the N-terminal part of the propeptide of BNP (NT-proBNP) immunoassays: the CardioOrmocheck study. Clin Chem Lab Med. 2009. In press.

12. Chen AA, Wood MJ, Krauser DG, Baggish AL, Tung R, Anwaruddin S, et al. NT-proBNP levels, echocardiographic findings, and outcomes in breathless patients: results from the ProBNP Investigation of Dyspnoea in the Emergency Department (PRIDE) echocardiographic substudy. Eur Heart J. 2006. 27:839–845.

13. Vanderheyden M, Bartunek , Claeys G, Manoharan G, Beckers JF, Ide L. Head to head comparison of N-terminal pro-B-type natriuretic peptide and B-type natriuretic peptide in patients with/without left ventricular systolic dysfunction. Clin Biochem. 2006. 39:640–645.
14. Brown A, George J, Murphy MJ, Struthers A. Could BNP screening of acute chest pain cases lead to safe earlier discharge of patients with non-cardiac causes? A pilot study. QJM. 2007. 100:755–761.

15. Fukuta H, Ohte N, Mukai S, Saeki T, Kobayashi K, Kimura G. Anemia is an independent predictor for elevated plasma levels of natriuretic peptides in patients undergoing cardiac catheterization for coronary artery disease. Circ J. 2008. 72:212–217.

16. Ogawa A, Seino Y, Yamashita T, Ogata K, Takano T. Difference in elevation of N-terminal pro-BNP and conventional cardiac markers between patients with ST elevation vs non-ST elevation acute coronary syndrome. Circ J. 2006. 70:1372–1378.
17. Sinclair H, Paterson M, Walker S, Beckett G, Fox KA. Predicting outcome in patients with acute coronary syndrome: evaluation of B-type natriuretic peptide and the global registry of acute coronary events (GRACE) risk score. Scott Med J. 2007. 52:8–13.
18. Günes Y, Okçün B, Kavlak E, Erbas C, Ķarcier S. Value of brain natriuretic peptide after acute myocardial infarction. Anadolu Kardiyol Derg. 2008. 8:182–187.
19. Kwan G, Isakson SR, Beede J, Clopton P, Maisel AS, Fitzgerald RL. Short-term serial sampling of natriuretic peptides in patients presenting with chest pain. J Am Coll Cardiol. 2007. 49:1186–1192.
20. Palazzuoli A, Rizzello V, Calabrò A, Gallotta M, Martini G, Quatrini I, et al. Osteoprotegerin and B-type natriuretic peptide in non-ST elevation acute coronary syndromes: relation to coronary artery narrowing and plaques number. Clin Chim Acta. 2008. 391:74–79.
21. Sun T, Wang L, Zhang Y. Prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. Arch Med Res. 2006. 37:502–505.

22. Fonarow GC, Peacock WF, Horwich TB, Phillips CO, Givertz MM, Lopatin M, et al. Usefulness of B-Type natriuretic peptide and cardiac troponin levels to predict in-hospital mortality from ADHERE. Am J Cardiol. 2008. 101:231–237.

23. Tello-Montoliu A, Marín F, Roldán V, Mainar L, López MT, Sogorb F, et al. A multimarker risk stratification approach to non-ST elevation acute coronary syndrome: implications of troponin T, CRP, NT pro-BNP and fibrin D-dimer levels. J Intern Med. 2007. 262:651–658.

24. Morrow DA, de Lemos JA, Blazing MA, Sabatine MS, Murphy SA, Jarolim P, et al. Prognostic value of serial B-type natriuretic peptide testing during follow-up of patients with unstable coronary artery disease. JAMA. 2005. 294:2866–2871.

25. Yildirir A, Acikel S, Ertan C, Aydinalp A, Ozin B, Muderrisoglu H. Value of peri-procedural B-type natriuretic peptide levels in predicting cardiac events after elective percutaneous coronary intervention. Acta Cardiol. 2008. 63:47–52.

26. Lo Mauro R, Arcoleo F, Lo Giudice A, Picone A, Schirosa M, Raspanti G, et al. B-type natriuretic peptide as a marker of asymptomatic re-stenosis after coronary implantation of a paclitaxeleluting stent. J Cardiovasc Med (Hagerstown). 2007. 8:1020–1023.

27. Elíasdóttir SB, Klemenzson G, Torfason B, Valsson F. Brain natriuretic peptide is a good predictor for outcome in cardiac surgery. Acta Anaesthesiol Scand. 2008. 52:182–187.

28. Turk T, Ata Y, Ay D, Ozkan H, Vural H, Yavuz S, et al. Plasma brain natriuretic peptide after isolated on-pump coronary artery bypass grafting: prediction of postoperative adverse outcomes. Heart Surg Forum. 2008. 11:E84–E89.

29. Sarzi Braga S, Vaninetti R, Pedretti RF. Plasma B-type natriuretic peptide predicts atrial fibrillation during rehabilitation after cardiac surgery. Eur J Cardiovasc Prev Rehabil. 2008. 15:460–466.

30. Shaw SM, Fildes J, Yonan N, Williams SG. Does brain natriuretic peptide interact with the immune system after cardiac transplantation? Transplantation. 2007. 84:1377–1381.

31. Rossano JW, Denfield SW, Kim JJ, Price JF, Jefferies JL, Decker JA, et al. B-type Natriuretic peptide is a sensitive screening test for acute rejection in pediatric heart transplant patients. J Heart Lung Transplant. 2008. 27:649–654.

32. Martínez-Dolz L, Almenar L, Hervás I, Moro J, Agüero J, Sánchez-Lázaro I, et al. Prognostic relationship between two serial determinations of B-type natriuretic peptide and medium-long-term events in heart transplantation. J Heart Lung Transplant. 2008. 27:735–740.

33. Heise G, Lemmer J, Weng Y, Hübler M, Alexi-Meskishvili V, Böttcher W, et al. Biomarker responses during mid-term mechanical cardiac support in children. J Heart Lung Transplant. 2008. 27:150–157.

34. Pruszczyk P. N-terminal pro-brain natriuretic peptide as an indicator of right ventricular dysfunction. J Card Fail. 2005. 11:S65–S69.

35. Alonso-Martínez JL, Urbieta-Echezarreta M, Anniccherico-Sánchez FJ, Abínzano-Guillén ML, Garcia-Sanchotena JL. N-terminal pro-B-type natriuretic peptide predicts the burden of pulmonary embolism. Am J Med Sci. 2009. 337:88–92.

36. Yardan T, Altintop L, Baydin A, Yilmaz O, Guven H. B-type natriuretic peptide as an indicator of right ventricular dysfunction in acute pulmonary embolism. Int J Clin Pract. 2008. 62:1177–1182.

37. Binder L, Pieske B, Olschewski M, Geibel A, Klostermann B, Reiner C, et al. N-terminal pro-brain natriuretic peptide or troponin testing followed by echocardiography for risk stratification of acute pulmonary embolism. Circulation. 2005. 112:1573–1579.

38. Enea I, Ceparano G, Mazzarella G, Di Sarno R, Cangiano G, Busino CA. [Biohumoral markers and right ventricular dysfunction in acute pulmonary embolism: the answer to thrombolytic therapy]. Ital Heart J Suppl. 2004. 5:29–35.
39. Logeart D, Lecuyer L, Thabut G, Tabet JY, Tartière JM, Chavelas C, et al. Biomarker-based strategy for screening right ventricular dysfunction in patients with non-massive pulmonary embolism. Intensive Care Med. 2007. 33:286–292.

40. Yap LB, Mukerjee D, Timms PM, Ashrafian H, Coghlan JG. Natriuretic peptides, respiratory disease, and the right heart. Chest. 2004. 126:1330–1336.

41. Yano S, Kobayashi K, Kato K, Ikeda T. [The study of pulmonary hypertension and plasma BNP values in respiratory diseases]. Nihon Kokyuki Gakkai Zasshi. 2006. 44:99–103.
42. Andreassen AK, Wergeland R, Simonsen S, Geiran O, Guevara C, Ueland T. N-terminal pro-B-type natriuretic peptide as an indicator of disease severity in a heterogeneous group of patients with chronic precapillary pulmonary hypertension. Am J Cardiol. 2006. 98:525–529.

43. Yap LB, Mukerjee D, Timms PM, Ashrafian H, Coghlan JG. Natriuretic peptides, respiratory disease, and the right heart. Chest. 2004. 126:1330–1336.

44. Kanat F, Vatansev H, Teke T. Diuretics, plasma brain natriuretic peptide and chronic obstructive pulmonary disease. Neth J Med. 2007. 65:296–300.
45. Stolz D, Breidthardt T, Christ-Crain M, Bingisser R, Miedinger D, Leuppi J, et al. Use of B-type natriuretic peptide in the risk stratification of acute exacerbations of COPD. Chest. 2008. 133:1088–1094.

46. Chien JY, Lin MS, Huang YC, Chien YF, Yu CJ, Yang PC. Changes in B-type natriuretic peptide improve weaning outcome predicted by spontaneous breathing trial. Crit Care Med. 2008. 36:1421–1426.

47. Moe GW, Howlett J, Januzzi JL, Zowall H. Canadian Multicenter Improved Management of Patients With Congestive Heart Failure (IMPROVE-CHF) Study Investigators. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation. 2007. 115:3103–3110.

48. Iltumur K, Karabulut A, Yokus B, Yavuzkir M, Taskesen T, Toprak N. N-terminal proBNP plasma levels correlate with severity of mitral stenosis. J Heart Valve Dis. 2005. 14:735–741.
49. Arat-Ozkan A, Kaya A, Yigit Z, Balci H, Okçün B, Yazicioglu N, et al. Serum N-terminal pro-BNP levels correlate with symptoms and echocardiographic findings in patients with mitral stenosis. Echocardiography. 2005. 22:473–478.

50. Cemri M, Arslan U, Kocaman SA, Cengel A. Relationship between N-terminal pro-B type natriuretic peptide and extensive echocardiographic parameters in mild to moderate aortic stenosis. J Postgrad Med. 2008. 54:12–16.

51. Della Corte A, Salerno G, Chiosi E, Iarussi D, Santarpino G, Miraglia M, et al. Preoperative, postoperative and 1-year follow-up N-terminal pro-B-type natriuretic peptide levels in severe chronic aortic regurgitation: correlations with echocardiographic findings. Interact Cardiovasc Thorac Surg. 2008. 7:419–424.

52. Moura LM, Rocha-Gonçalves F, Zamorano JL, Barros I, Bettencourt P, Rajamannan N. New cardiovascular biomarkers: clinical implications in patients with valvular heart disease. Expert Rev Cardiovasc Ther. 2008. 6:945–954.

53. Iversen K, Nielsen OW, Kirk V, Bay M, Hassager C, Boesgaard S, et al. Heart murmur and N-terminal pro-brain natriuretic peptide as predictors of death in 2977 consecutive hospitalized patients. Am J Med Sci. 2008. 335:444–450.

54. Therkelsen SK, Groenning BA, Kjaer A, Svendsen JH, Boje Jensen G. ANP and BNP in atrial fibrillation before and after cardioversion--and their relationship to cardiac volume and function. Int J Cardiol. 2008. 127:396–399.

55. Sacher F, Corcuff JB, Schraub P, Le Bouffos V, Georges A, Jones SO, et al. Chronic atrial fibrillation ablation impact on endocrine and mechanical cardiac functions. Eur Heart J. 2008. 29:1290–1295.

56. Tveit A, Seljeflot I, Grundvold I, Abdelnoor M, Arnesen H, Smith P. Candesartan, NT-proBNP and recurrence of atrial fibrillation after electrical cardioversion. Int J Cardiol. 2009. 131:234–239.

57. Yamada T, Murakami Y, Okada T, Yoshida N, Toyama J, Yoshida Y, et al. Plasma brain natriuretic peptide level after hybrid therapy with pulmonary vein isolation and antiarrhythmic drugs for atrial fibrillation. Int Heart J. 2008. 49:143–151.

58. Ahlsson A, Linde P, Rask P, Englund A. Atrial function after epicardial microwave ablation in patients with atrial fibrillation. Scand Cardiovasc J. 2008. 42:192–201.

59. Magioncalda A, Sartini M, Costaguta C, Castellaneta M, Schenone E, Tognoni E, et al. [The utility of assaying the N-terminal of brain natriuretic peptide precursor (NT pro-BNP) to predict the clinical outcome in patients with supraventricular tachyarrhythmias observed and treated in the emergency room]. Recenti Prog Med. 2008. 99:141–145.
60. Kawanishi Y, Ito T, Suwa M, Terasaki F, Futai R, Kitaura Y. Effect of left ventricular dyssynchrony on plasma B-type natriuretic peptide levels in patients with long-term right ventricular apical pacing. Int Heart J. 2008. 49:165–173.
61. Koch A, Zink S, Dittrich S. Plasma levels of B-type natriuretic peptide in children and adolescents with high degree atrioventricular block. Int J Cardiol. 2009. 134:429–430.
62. Ogawa T, Veinot JP, Kuroski de Bold ML, Georgalis T, de Bold AJ. Angiotensin II receptor antagonism reverts the selective cardiac BNP upregulation and secretion observed in myocarditis. Am J Physiol Heart Circ Physiol. 2008. 294:H2596–H2603.
63. Grabowski M, Karpiński G, J Filipiak K, Rdzanek A, Pietrasik A, Wretowski D, et al. Diagnostic value of BNP in suspected perimyocarditis--a preliminary report. Kardiol Pol. 2004. 61:451–458.
64. Kahveci G, Bayrak F, Mutlu B, Bitigen A, Karaahmet T, Sonmez K, et al. Prognostic value of N-terminal pro-B-type natriuretic peptide in patients with active infective endocarditis. Am J Cardiol. 2007. 99:1429–1433.
65. Bayram E, Kocatürk H, Yücel O, Atalay C, Colak MC, Atesal S. The role of adrenomedullin and brain natriuretic peptide levels in acute rheumatic fever in adults. Anadolu Kardiyol Derg. 2008. 8:188–191.
66. Zhang QY, Du JB, Chen YH, Li WZ. [Change in plasma N-terminal pro-brain natriuretic peptide in children with Kawasaki disease and its value in clinical practice]. Zhonghua Er Ke Za Zhi. 2006. 44:886–890.
67. Leya FS, Arab D, Joyal D, Shioura KM, Lewis BE, Steen LH, et al. The efficacy of brain natriuretic peptide levels in differentiating constrictive pericarditis from restrictive cardiomyopathy. J Am Coll Cardiol. 2005. 45:1900–1902.
68. Babuin L, Alegria JR, Oh JK, Nishimura RA, Jaffe AS. Brain natriuretic peptide levels in constrictive pericarditis and restrictive cardiomyopathy. J Am Coll Cardiol. 2006. 47:1489–1491.
69. Pfister R, Diedrichs H, Larbig R, Erdmann E, Schneider CA. NT-pro-BNP for differential diagnosis in patients with syncope. Int J Cardiol. 2009. 133:51–54.

70. Usui Y, Tomiyama H, Hashimoto H, Takata Y, Inoue Y, Asano K, et al. Plasma B-type natriuretic peptide level is associated with left ventricular hypertrophy among obstructive sleep apnoea patients. J Hypertens. 2008. 26:117–123.

71. Ybarra J, Planas F, Pou JM. Aminoterminal pro-brain natriuretic peptide (NT-proBNP) and sleep-disordered breathing in morbidly obese females: a cross-sectional study. Diab Vasc Dis Res. 2008. 5:19–24.
72. Seki S, Tsurusaki T, Kasai T, Taniguchi I, Mochizuki S, Yoshimura M. Clinical significance of B-type natriuretic Peptide in the assessment of untreated hypertension. Circ J. 2008. 72:770–777.
73. Sbarouni E, Georgiadou P, Marathias A, Geroulanos S, Kremastinos DT. D-dimer and BNP levels in acute aortic dissection. Int J Cardiol. 2007. 122:170–172.
74. Czernik C, Lemmer J, Metze B, Koehne PS, Mueller C, Obladen M. B-type natriuretic peptide to predict ductus intervention in infants <28 weeks. Pediatr Res. 2008. 64:286–290.

75. Farombi-Oghuvbu I, Matthews T, Mayne PD, Guerin H, Corcoran JD. N-terminal pro-B-type natriuretic peptide: a measure of significant patent ductus arteriosus. Arch Dis Child Fetal Neonatal Ed. 2008. 93:F257–F260.

76. Palladini G, Campana C, Klersy C, Balduini A, Vadacca G, Perfetti V, et al. Serum N-terminal pro-brain natriuretic peptide is a sensitive marker of myocardial dysfunction in AL amyloidosis. Circulation. 2003. 107:2440–2445.
77. Nikolaou NI, Goritsas C, Dede M, Paissios NP, Papavasileiou M, Rombola AT, et al. Brain natriuretic peptide increases in septic patients without severe sepsis or shock. Eur J Intern Med. 2007. 18:535–541.

78. Nakamura T, Suzuki T, Kawagoe Y, Koide H. Polymyxin B-immobilized fiber hemoperfusion attenuates increased plasma atrial natriuretic peptide and brain natriuretic Peptide levels in patients with septic shock. ASAIO J. 2008. 54:210–213.

79. Christ-Crain M, Breidthardt T, Stolz D, Zobrist K, Bingisser R, Miedinger D, et al. Use of B-type natriuretic peptide in the risk stratification of community-acquired pneumonia. J Intern Med. 2008. 264:166–176.

80. Kandil E, Burack J, Sawas A, Bibawy H, Schwartzman A, Zenilman ME, et al. B-type natriuretic peptide: a biomarker for the diagnosis and risk stratification of patients with septic shock. Arch Surg. 2008. 143:242–246.
81. Varpula M, Pulkki K, Karlsson S, Ruokonen E, Pettilä V. FINNSEPSIS Study Group. Predictive value of N-terminal probrain natriuretic peptide in severe sepsis and septic shock. Crit Care Med. 2007. 35:1277–1283.

82. Naganuma T, Sugimura K, Wada S, Yasumoto R, Sugimura T, Masuda C, et al. The prognostic role of brain natriuretic peptides in hemodialysis patients. Am J Nephrol. 2002. 22:437–444.

83. Goei D, Schouten O, Boersma E, Welten GM, Dunkelgrun M, Lindemans J, et al. Influence of renal function on the usefulness of N-terminal pro-B-type natriuretic peptide as a prognostic cardiac risk marker in patients undergoing noncardiac vascular surgery. Am J Cardiol. 2008. 101:122–126.
84. Tagore R, Ling LH, Yang H, Daw HY, Chan YH, Sethi SK. Natriuretic peptides in chronic kidney disease. Clin J Am Soc Nephrol. 2008. 3:1644–1651.

85. Biasioli S, Zamperetti M, Borin D, Guidi G, De Fanti E, Schiavon R. Significance of plasma B-type natriuretic peptide in hemodialysis patients: blood sample timing and comorbidity burden. ASAIO J. 2007. 53:587–591.

86. Winkler K, Wanner C, Drechsler C, Lilienthal J, März W, Krane V. for the German Diabetes and Dialysis Study Investigators. Change in N-terminal-pro-B-type-natriuretic-peptide and the risk of sudden death, stroke, myocardial infarction, and all-cause mortality in diabetic dialysis patients. Eur Heart J. 2008. 07. 09. [Epubahead of print].

87. Yildiz R, Yildirim B, Karincaoglu M, Harputluoglu M, Hilmioglu F. Brain natriuretic peptide and severity of disease in non-alcoholic cirrhotic patients. J Gastroenterol Hepatol. 2005. 20:1115–1120.

88. Henriksen JH, Gøtze JP, Fuglsang S, Christensen E, Bendtsen F, Møller S. Increased circulating pro-brain natriuretic peptide (proBNP) and brain natriuretic peptide (BNP) in patients with cirrhosis: relation to cardiovascular dysfunction and severity of disease. Gut. 2003. 52:1511–1517.
89. Januzzi JL, Morss A, Tung R, Pino R, Fifer MA, Thompson BT, et al. Natriuretic peptide testing for the evaluation of critically ill patients with shock in the intensive care unit: a prospective cohort study. Crit Care. 2006. 10:R37.
90. Levitt JE, Vinayak AG, Gehlbach BK, Pohlman A, Van Cleve W, Hall JB, et al. Diagnostic utility of B-type natriuretic peptide in critically ill patients with pulmonary edema: a prospective cohort study. Crit Care. 2008. 12:R3.

91. Kia M, Cooley A, Rimmer G, MacDonald T, Barber K, Manion P, et al. The efficacy of B-type natriuretic peptide for early identification of blood loss in traumatic injury. Am J Surg. 2006. 191:353–357.

92. Tobian AA, Sokoll LJ, Tisch DJ, Ness PM, Shan H. N-terminal pro-brain natriuretic peptide is a useful diagnostic marker for transfusion-associated circulatory overload. Transfusion. 2008. 48:1143–1150.
93. Meyer B, Huelsmann M, Wexberg P, Delle Karth G, Berger R, Moertl D, et al. N-terminal pro-B-type natriuretic peptide is an independent predictor of outcome in an unselected cohort of critically ill patients. Crit Care Med. 2007. 35:2268–2273.
94. Schultz M, Faber J, Kistorp C, Jarløv A, Pedersen F, Wiinberg N, et al. N-terminal-pro-B-type natriuretic peptide (NT-pro-BNP) in different thyroid function states. Clin Endocrinol (Oxf). 2004. 60:54–59.
95. Wei T, Zeng C, Tian Y, Chen Q, Wang L. B-type natriuretic peptide in patients with clinical hyperthyroidism. J Endocrinol Invest. 2005. 28:8–11.
96. Ozmen B, Ozmen D, Parildar Z, Mutaf I, Bayindir O. Serum N-terminal-pro-B-type natriuretic peptide (NT-pro-BNP) levels in hyperthyroidism and hypothyroidism. Endocr Res. 2007. 32:1–8.

97. Anne M, Juha K, Timo M, Mikko T, Olli V, Kyösti S, et al. Neurohormonal activation in ischemic stroke: effects of acute phase disturbances on long-term mortality. Curr Neurovasc Res. 2007. 4:170–175.

98. Giannakoulas G, Hatzitolios A, Karvounis H, Koliakos G, Charitandi A, Dimitroulas T, et al. N-terminal pro-brain natriuretic peptide levels are elevated in patients with acute ischemic stroke. Angiology. 2005. 56:723–730.

99. Nakagawa K, Yamaguchi T, Seida M, Yamada S, Imae S, Tanaka Y, et al. Plasma concentrations of brain natriuretic peptide in patients with acute ischemic stroke. Cerebrovasc Dis. 2005. 19:157–164.

100. Di Angelantonio E, De Castro S, Toni D, Sacchetti ML, Biraschi F, Prencipe M, et al. Determinants of plasma levels of brain natriuretic peptide after acute ischemic stroke or TIA. J Neurol Sci. 2007. 260:139–142.

101. Montaner J, Perea-Gainza M, Delgado P, Ribó M, Chacón P, Rosell A, et al. Etiologic diagnosis of ischemic stroke subtypes with plasma biomarkers. Stroke. 2008. 39:2280–2287.

102. Anne M, Juha K, Timo M, Mikko T, Olli V, Kyösti S, et al. Neurohormonal activation in ischemic stroke: effects of acute phase disturbances on long-term mortality. Curr Neurovasc Res. 2007. 4:170–175.

103. Berendes E, Walter M, Cullen P, Prien T, Van Aken H, Horsthemke J, et al. Secretion of brain natriuretic peptide in patients with aneurysmal subarachnoid haemorrhage. Lancet. 1997. 349:245–249.
104. Lu DC, Binder DK, Chien B, Maisel A, Manley GT. Cerebral salt wasting and elevated brain natriuretic peptide levels after traumatic brain injury: 2 case reports. Surg Neurol. 2008. 69:226–229.

105. Stewart D, Waxman K, Brown CA, Schuster R, Schuster L, Hvingelby EM, et al. B-type natriuretic peptide levels may be elevated in the critically injured trauma patient without congestive heart failure. J Trauma. 2007. 63:747–750.

106. Tung PP, Olmsted E, Kopelnik A, Banki NM, Drew BJ, Ko N, et al. Plasma B-type natriuretic peptide levels are associated with early cardiac dysfunction after subarachnoid hemorrhage. Stroke. 2005. 36:1567–1569.

107. Espiner EA, Leikis R, Ferch RD, MacFarlane MR, Bonkowski JA, Frampton CM, et al. The neuro-cardio-endocrine response to acute subarachnoid haemorrhage. Clin Endocrinol Oxf. 2002. 56:629–635.

108. Kirchhoff C, Stegmaier J, Bogner V, Buhmann S, Mussack T, Kreimeier U, et al. Intrathecal and systemic concentration of NT-proBNP in patients with severe traumatic brain injury. J Neurotrauma. 2006. 23:943–949.

109. Yarlagadda S, Rajendran P, Miss JC, Banki NM, Kopelnik A, Wu AH, et al. Cardiovascular predictors of in-patient mortality after subarachnoid hemorrhage. Neurocrit Care. 2006. 5:102–107.

110. Rauchenzauner M, Haberlandt E, Foerster S, Ulmer H, Laimer M, Ebenbichler CF, et al. Brain-type natriuretic peptide secretion following febrile and afebrile seizures - a new marker in childhood epilepsy? Epilepsia. 2007. 48:101–106.
111. Obi T, Takatsu M, Konishi T, Mizoguchi K, Nishimura Y. Secretion of natriuretic peptides caused by an epileptic attack. Acta Neurol Scand. 2002. 106:225–228.

112. Davutoglu V, Gunay N, Kocoglu H, Gunay NE, Yildirim C, Cavdar M, et al. Serum levels of NT-ProBNP as an early cardiac marker of carbon monoxide poisoning. Inhal Toxicol. 2006. 18:155–158.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download