Abstract
Eosinophilic gastroenteritis (EG) is characterized by eosinophilic infiltration of the bowel wall and variable gastrointestinal manifestations. Clinicians should have a high index of suspicion for EG when faced with gastrointestinal symptoms and peripheral eosinophilia to avoid incorrect diagnosis and inappropriate treatments. A 24-year-old woman was admitted to our hospital complaining of acute right lower quadrant abdominal pain and a laparoscopic appendectomy performed for a presumed diagnosis of an acute appendicitis. However, the procedure revealed bowel edema and a moderate amount of ascites without evidence of a suppurative appendicitis. Postoperatively, she showed persistent and progressive eosinophilia, exudative eosinophilic ascites, eosinophilic infiltration of the resected appendix wall, and eosinophilic infiltration of gastroduodenal mucosa. A punch biopsy of the abdominal skin also revealed inflammation with marked eosinophilic infiltration of the skin. She recovered after the treatment with a low dose of steroid for the EG with eosinophilic dermatitis. EG with eosinophilic dermatitis has not been reported yet and is considered fortuitous in this case.
Eosinophilic gastroenteritis (EG) is a rare disease of unknown etiology, which is characterized by eosinophilic inflammation of the bowel wall and various gastrointestinal manifestations.1 The diagnosis of EG is confirmed by a characteristic biopsy or eosinophilic ascitic fluid in the absence of other known causes of eosinophilia. Clinicians should have a high index of suspicion for EG when faced with gastrointestinal symptoms and peripheral eosinophilia because this medically treatable disease may mimic surgical conditions. We report a case of EG with eosinophilic dermatitis mimicking acute appendicitis who responded to a course of low-dose steroid.
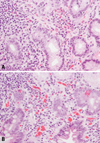
A 24-year-old woman arrived in the emergency department complaining of acute right lower quadrant abdominal pain and vomiting. She did not report any weight loss or diarrhea. She had no history of abdominal surgery or any other allergic disease. She denied taking any drugs or herbal medicines. A physical examination of the abdomen revealed tenderness with rebound tenderness in the right lower quadrant of her abdomen. Initial laboratory investigations showed a white cell count of 14,400/mm3 with 75% neutrophils, 16% lymphocytes, 3.3% monocytes, and 4.3% eosinophils (an absolute eosinophil count of 619/mm3). Other laboratory tests and stool examination for ova and parasites were within normal limits. Based on her physical examination, a laparoscopic appendectomy was performed for a presumed diagnosis of an acute appendicitis; however, it revealed bowel edema and a moderate amount of ascites in the abdominal cavity without gross evidence of appendicitis. The appendectomy specimen showed eosinophilics were infiltrating the muscular and subserosal layers of the appendix wall (Fig. 1). Ascitic fluid analysis showed exudative ascites with predominant eosinophils (a white cell count of 3,150 cells/µL with 75% eosinophils) and no evidence of malignant cells. Postoperatively, the degree of peripheral eosinophilia progressed to 1,729/mm3. Tests for antinuclear factor, rheumatoid factor, antineutrophilic cytoplasmic autoantibody, and skin prick test were all negative.
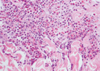
A gastroscopy showed marked edema of the gastric antrum and narrowing of the pyloric ring. The duodenum also showed mucosal edema with erythema. Biopsies of the gastric antrum and proximal duodenum revealed inflammation with eosinophilic infiltration (Fig. 2). A colonoscopy showed normal mucosa without eosinophilic infiltration. Although an abnormal skin lesion was not observed, a punch biopsy of the central abdominal skin revealed diffuse perivascular and interstitial inflammation with marked eosinophilic infiltration (Fig. 3). The diagnosis of EG with eosinophilic dermatitis was made based on these findings, and she was treated with oral prednisolone 40 mg/day. Her symptoms disappeared within 7 days and steroid treatment was tapered gradually and terminated after 28 days. Follow-up eosinophil count, endoscopic findings and abdominal ultrasonographic findings were normalized after 28 days of medication.
EG is classified into three major types according to the predominance of the eosinophilic infiltration in the different layers of the intestinal wall: mucosal, muscular, and subserosal types.2,3 Involvement of the different layers of the intestinal wall usually gives rise to different clinical manifestations. In this patient, eosinophils predominantly infiltrated the muscular and subserosal layers of the intestinal wall, which resulted in bowel wall edema, eosinophilic ascites, and abdominal pain mimicking appendicitis. Clinicians should be aware of diverse gastrointestinal manifestations of EG to avoid an unnecessary surgical approach,4 as in this patient. Some studies have speculated that allergies to certain foods or immunological abnormalities are causes;5,6 however, none of these findings were observed in this patient.
Tally, et al.7 proposed three main diagnostic criteria of EG: the presence of gastrointestinal symptoms, biopsies demonstrating eosinophilic infiltration of one or more areas of the gastrointestinal tract, and no evidence of parasitic or extra-intestinal diseases. Therefore, histological identification of an eosinophilic infiltration by an endoscopic biopsy is essential, but it is not always simple. Endoscopic biopsies may not demonstrate the eosinophilic infiltration due to its patchy mucosal involvement.8 In addition, it often fails to detect eosinophilic infiltration in the muscular or subserosal type of EG, and a laparotomy or laparoscopic full-thickness biopsy may be required in such cases.9 As the normal gastrointestinal tract may contain detectable eosinophils,1 the histological diagnosis of EG relies on a large amount of eosinophilic infiltration and, more impressively, the presence of extracellular eosinophilic staining constituents (often free granules) as in this patient.
In most cases, peripheral eosinophilia was the usual initial clue to detect EG;2,7,9 however, peripheral eosinophilia may be initially absent or mild in EG,7 as in our patient. As the EG rarely involves other organs, our case is most unusual in that eosinophilic dermatitis was present. EG with eosinophilic dermatitis may be confused as hypereosinophilic syndrome (HES). Yet, our patient did not meet the diagnostic criteria of HES because she lacked severe peripheral eosinophilia (> 1,500 cells/mm3) for more than 6 months and the presence of end-organ involvement such as heart, lungs, brain, and kidneys.10 To the best of our knowledge, no cases of EG associated with eosinophilic dermatitis have been reported. As such, an association has not been observed by earlier authors, though it may be simply a coincidence. However, the association may have been underestimated as the skin biopsy is not the usual practice in patients with EG. A punch biopsy of skin may provide additional information in the EG with eosinophilic dermatitis, when endoscopic biopsies fail to detect EG because of its muscular or subserosal type or patchy mucosal infiltration.
Clinical improvement is usually seen after a treatment with a low dose of steroid,1,9 such as prednisone with daily doses of 20 to 40 mg as in our patient. Surgical intervention may sometimes be required when a definite diagnosis cannot be made or when complications such as obstruction or perforation occur.11 Unnecessary surgery, though, should be avoided as occurred in our patient.
In conclusion, clinicians should have a high index of suspicion for EG when encountering gastrointestinal symptoms and peripheral eosinophilia because this medically treatable disease may mimic a surgical condition. In addition, EG may be associated with eosinophic dermatitis and further investigations for this association may be necessary.
Figures and Tables
 | Fig. 1Microscopic findings of the resected appendix showed a diffuse eosinophilic infiltration from the muscular layer to the subserosal layer of the appendix wall (H&E stain, A: ×40 and B: ×400). |
References
1. Rothenberg ME. Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol. 2004. 113:11–28.
2. Klein NC, Hargrove RL, Sleisenger MH, Jeffries GH. Eosinophlic gastroenteritis. Medicine (Baltimore). 1970. 49:299–319.
3. Kim JD, Im EH, Lee JH, Lee TH, Kim SM, Choi YW, et al. A case of eosinophilic esophagogastroenteritis with transmural involvement. Korean J Gastrointest Endosc. 2007. 35:404–409.
4. Tran D, Salloum L, Tshibaka C, Moser R. Eosinophilic gastroenteritis mimicking acute appendicitis. Am Surg. 2000. 66:990–992.
5. Liacouras CA. Eosinophilic esophagitis in children and adults. J Pediatr Gastroenterol Nutr. 2003. 37:Suppl 1. S23–S28.

6. Kweon MN, Kiyono H. Eosinophilic gastroenteritis: a problem of the mucosal immune systems? Curr Allergy Asthma Rep. 2003. 3:79–85.

7. Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR. Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissue. Gut. 1990. 31:54–58.

8. Katz AJ, Goldman H, Grand RJ. Gastric mucosal biopsy in eosinophilic (allergic) gastroenteritis. Gastroenterology. 1977. 73:705–709.

10. Rothenberg ME. Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol. 2004. 113:11–28.

11. Vara-Thorbeck C, Toscano-Mendez R, Osorio D. Eosinophilic gastroenteritis: diagnostic laparoscopy. Surg Laparosc Endosc. 1997. 7:66–69.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download