Abstract
Purpose
After a century, cheiro-oral syndrome (COS) was harangued and emphasized for its localizing value and benign course in recent two decades. However, an expanding body of case series challenged when COS may arise from an involvement of ascending sensory pathways between cortex and pons and terminate into poor outcome occasionally.
Materials and Methods
To analyze the location, underlying etiologies and prognosis in 76 patients presented with COS collected between 1989 and 2007.
Results
Four types of COS were categorized, namely unilateral (71.1%), typically bilateral (14.5%), atypically bilateral (7.9%) and crossed COS (6.5%). The most common site of COS occurrence was at pons (27.6%), following by thalamus (21.1%) and cortex (15.8%). Stroke with small infarctions or hemorrhage was the leading cause. Paroxysmal paresthesia was predicted for cortical involvement and bilateral paresthesia for pontine involvement, whereas crossed paresthesia for medullary involvement. However, the majority of lesions cannot be localized by clinical symptoms alone, and were demonstrated only by neuroimaging. Deterioration was ensued in 12% of patients, whose lesions were large cortical infarction, medullary infarction, and bilateral subdural hemorrhage.
Conclusion
COS arises from varied sites between medulla and cortex, and is usually caused by small stroke lesion. Neurological deterioration occurs in 12% of patients and relates to large vessel occlusion, medullary involvement or cortical stroke. Since the location and deterioration of COS cannot be predicted by clinical symptoms alone, COS should be considered an emergent condition for aggressive investigation until fatal cause is substantially excluded.
In 1914, Sitting1 reported three patients presenting with unilateral sensory impairment which was restricted at their perioral area and homolateral distal finger(s)/hand. Their responsible lesions, namely encephalitis, gumma, and vascular malformation, were found at their contralateral postcentral gyrus on autopsy for a period of time after onset. Later, this peculiar sensory disorder was also found in thalamic stroke.2,3 This characteristic unilateral sensory disorder was soon coined as cheiro-oral syndrome (COS). At that moment, COS was considered to proffer two contributions in clinical medicine, including a neuroanatomic localization at cortex or thalamus and a benign neurological course.
Following the advert of COS in Europe, an accumulation of case series of COS has subsequently been reported in European countries other from German and France, North America, Japan, Korea4 and Taiwan.5 In contrast to previous suggestion that COS provides a localizing value,6 current knowledge has already realized that COS can arise from an involvement of the spinothalamocortical and trigeminothalamocortical tract between pons and sensory cortex. A few corresponding etiologies are also found. In recent publications, there are three main streams of thought concerning COS: an association with uncommon intracranial cause,7,8 concomitant uncommon neurological deficits,9,10 and an increasing number of variants.11-13 This trend adumbrates COS merely a clinical presentation without diagnostic or prognostic value. In this study, the neuroanatomy, underlying cause and clinical course were analyzed in 76 patients presenting with COS. In contrast to recent suggestion that COS displays a poverty of diagnostic and prognostic value, COS was actually found to be an early warning sign for neurological exacerbation obligatory for aggressive investigation herein.
A prospective study has been carried out to analyze the localization, pathogenesis and prognosis of COS since 1989 (from 1989 to 2000 at Kaohsiung Medical University Hospital, Kaohsiung, Taiwan, and from 2001 to 2007 at Chang Gung Memorial Hospital-Kaohsiung Medical Center, Kaohsiung, Taiwan). In this database, COS was strictly defined as a sensory impairment confined to the perioral area and the ipsilateral finger(s)/hand, without a detectable abnormality in mental, memory, motor or cerebellar function. COS patients were also excluded when COS was an ictus in migraine or due to intoxication from marine toxin or other cause. However, a mild change of tendon reflex or muscle tonicity without a decrease of muscle strength, an association with a focal seizure or movement disorder, or a neurological deficit probably due to previous event was not contraindicated. Each patient received detailed medical history evaluation, neurological examination, cranial computerized tomography or magnetic resonance image, and somatosensory evolved potential to localize their pathological location. If necessary, further appropriate tests would be performed and their procedures had been mentioned in previous reports.5,14-19
A corresponding lesion was defined as a lesion which was detected under neuroimaging study, and was time- and neuroanatomic-compatible with concomitant neurological manifestation. Accordingly, a T2-weighted or fluid attenuated inversion recovery (FLAIR)-weighted intensity situated within the ascending sensory pathway could not be considered a corresponding lesion if there was no parallel change in diffusion weighted image (DWI) or apparent diffusion coefficient (ADC)-weighted image, and in T1-weighted image if hemorrhage was considered. Patient was considered to have no corresponding lesion when there was no lesion found, lesion not compatible with concomitant neurological manifestation, or only T2-weighted or FLAIR-weighted hyperintense lesion without parallel change in DWI, ADC or T1-weighted image.
In case of brainstem hemorrhage which extended beyond one or more neuroanatomic landmarks (midbrain, pons, medulla oblongata), the location was selected for the site where the hematoma volume was the biggest. The hematoma or infarction at brainstem was considered large when the area of infarction or hematoma was over one-fourth area of brainstem at the same level. Otherwise, it was small.
Categorical variables were expressed as number and percentage. Chi-Square test and Fisher exact test were used for statistical analysis. A probability less than 0.05 was accepted as significance.
Between 1989 and 2007, there were 76 patients presented with COS enrolled. Some of them had been reported in previous publications.5,14-19 They were 49 men and 27 women. The age ranged from 41 to 74 years.
Basing on the distribution of sensory impairments, four types of COS were categorized. Type I COS was sensory impairment confined to perioral area and homolateral finger(s)/hand in unilaterality. Type II COS was sensory impairment confined to perioral area and finger(s)/hand in bilaterality. Type III COS was sensory impairment confined to perioral area and finger(s)/hand in that one was involved in bilaterality whereas another one in unilaterality. It was an incomplete and atypical form of type II COS. Type IV COS was sensory impairment confined to perioral area and opposite finger(s)/hand, or crossed COS. Finally, type I included 54 patients (71.1%), type II 11 patients (14.5%), type III 6 patients (7.9%), and type IV 5 patients (6.5%).
All patients presented an abrupt onset of paresthesia confined to perioral area and finger(s)/hand initially without conscious change. Their paresthesia was usually described as numb or tingling, and also piercing, thickening, thinning, burning, spicy, coldness, ice, or crawling. In three patients, subjective paresthesia occurred at fingers whereas hypesthesia to pinprick pain and cotton fine touch was only detected at perioral area on examination. Intermittent focal motor convulsion was present in 1 patient with cortical meningioma and another one with arteriovenous malformation after onset.
The paresthesia was constant in 70 patients whereas paroxysmal in another 6 patients; namely, 3 type I patients whose etiology was cortical arteriovenous malformation or meningioma, 1 type I patient with subdural hemorrhage, and 2 type 1 patients with pontine infarction in whom their sensorum exacerbated in parallel to an increase of blood pressure.17 Paroxysmal paresthesia was more frequent in patients with cortical involvement (4 out of 12; 33.4%) than subcortical involvement (2 out of 70; 2.9%) in this series. Accordingly, a paroxysmal COS would predict for cortical involvement (Fisher's exact test, p = 0.0038).
A variable magnitude of exterioceptive (pinprick pain or cotton fine touch) or proprioceptive (positional joint sensation or vibratory sense) hypesthesia, ranging from 20% to 70% subjectively, was detected at perioral area or finger(s)/hand in most patients. No patient showed anesthesia to sensory stimulation. In practice, the magnitude of proprioceptive hypesthesia was usually mild. Cortical type-sensory impairment (astereognosis, barognosis, or graphesthesia) was detected in 6 patients (50.0%) with cortical involvement whereas 3 patients (18.8%) with thalamic involvement. Objective hypesthesia to pinprick pain, cotton fine touch, positional joint sensation and vibratory was detected in 6 (50.0%), 6 (50.0%), 4 (33.4%), and 4 (33.4%) out of 12 patients with cortical involvement; 12 (75.0%), 14 (87.5%), 4 (25.0%), and 4 (25.0%) out of 16 patients with thalamic involvement; and 15 (71.4%), 16 (76.2%), 3 (14.3%), and 4 (19.1%) out of 21 patients with pontine involvement, respectively. Cotton fine touch was the most common sensation involved. There was no difference in the frequency of exterioceptive or proprioceptive hypesthesia among cortical, thalamic and pontine involvement. However, a presence of cortical type-sensory impairment predicted for cortical involvement and thalamic involvement less. In addition, a crossed sensory impairment exclusively indicated medullary involvement.
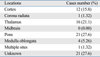
Associated symptoms were absent in 27 (35.5%), but present in 49 (64.5%) patients. The most frequent symptom was dizziness in 41 patients. Other dizziness-minus symptoms included facial flushing/hotness in 11, vertigo in 8, palpitation in 7, headache in 6, fatigue in 6, unsteadiness in 5, nausea in 3, blurred vision in 3, chest tightness in 3, tinnitus in 2, near-syncope feeling in 1, abdominal hyperactive feeling in 1, strange feeling to environment in 1, tooth-falling feeling in 1, and hiccough in 1 patient (Table 1). In these 49 patients, isolated dizziness was present in 17 patients, isolated dizziness-minus symptoms in 8 patients, and both dizziness and dizziness-minus symptoms in 24 patients. Dizziness and vertigo persisted for more than one day in some patients, however, all other associated symptoms subsided within 24 hours after onset.
Hypertension was present in 53 patients and was the most common associated medical comorbidity. Diabetes mellitus, Sjogren syndrome, and recent traumatic head injury were found in 9, 1 and 1 patient, respectively. In 18 patients, there was no associated medical comorbidity known before, but arteriovenous malformation, meningioma and acute myelogenous leukemia were found in 5 patients later after investigation.
Single lesion was found in 54 patients (71.1%), multiple lesions in 1 patient (1.32%) and no definite lesion in 21 patients (27.6%) (Table 2). The most common site of single lesion was pons (27.6%), followed by thalamus (21.1%), cortex (15.8%), and medullary oblongata (5.26%). No patient had midbrain involvement. In 11 of those 21 patients without definite intracranial lesions, previous multiple infarctions, hemorrhage or demyelination were disclosed. In another 6 patients, a variable range of cervical spondylosis was found. In another 4 patients, there was no structural abnormality disclosed.
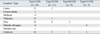
In the 54 patients in whom single lesion was identified, type II and III COS predicted for pontine involvement (Chi-Square test, F = 13.7, p < 0.001) whereas type IV COS for medullary involvement (Table 3).
Stroke was identified in 50 patients (65.8%) and small infarction was the leading cause in them (34 out of 50 patients; 68.0%). Small infarction and small hemorrhage were exclusively found at thalamus or pons, except one patient who had cortical infarction presenting with type I COS. Tumor and vascular malformation were found in 4 patients and they were exclusively located at cortex (Table 4).5,18 Multiple sites of infarction were found in 1 patient. In one Sjogren syndrome patient, her type II COS was ensued by painful polyneuropathy which was reversed by plasmapheresis. Her nerve conduction velocity study showed sensory axonopathy but magnetic resonance image did not reveal consistent abnormality. Acute myelogenous leukemia with subdural hemorrhage was found in an another type I patient after extensive investigation.18
In regard to stroke patients, detailed survey for stroke risk factor was performed. In the 3 patients with large cortical infarction, atherothrombosis was considered as remarkable atherosclerotic stenosis (≥ 50% stenosis of luminal area) of intracranial large artery was observed. In another one patient with small cortical infarction, atherosclerosis of middle cerebral artery branch was seen. Her cardiac function was normal. In those 24 patients with small infarctions at corona radiata, thalamus or pons, remarkable atherosclerosis of intracranial or extracranial arteries was disclosed in 6 of them, whereas minimal to mild atherosclerosis (≥ 50% stenosis of luminal area) was common. Old myocardial ischemia was found in 12 patients and atrial fibrillation in another 2 patients; they also had had hypertension or diabetes mellitus. There was no patient having dissecting disease or other nonatherosclerotic vasculopathy.
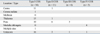
There were 9 patients who experienced a deterioration of neurological function ranging from 3 hours to 1 month after onset (Table 5).15,16,18,19 Three patients had medullary involvement with crossed COS,19 3 patients had subdural hemorrhage,15,18 2 patients had large cortical infarction,18 and one patient had large pontine hemorrhage.16 Surgical removal of hematoma was done in 2 subdural hemorrhage patients and decompressive craniotectomy in 1 large cortical infarction patient. Conservation treatment was performed in another 5 patients.
In another 67 patients who did not experience neurological deterioration, there was no specific measure other from cardiovascular risk factor control and stroke secondary prevention in patients with hemorrhage or infarction. In the Sjogren syndrome patient, plasmapheresis was done.
A favorable recovery of COS was ensued in 55 patients within 6 months after onset. Mild to moderate post-stroke central pain occurred in 12 patients and was abolished or attenuated by clonidine, amitriptyline or gabapentin. In those 9 patients with deterioration, mild ataxia was complicated in 2 of them, but moderate to severe functional disability was terminated in another 7 patients (Table 5).
Besides three clusters of neurological manifestations and localization, (paroxysmal paresthesia and cortical involvement, typically/atypically bilateral COS and pontine involvement, and crossed COS and medullary involvement), the predictive weight of neurological manifestation, associated symptoms, locations of lesions, and underlying etiologies for prognosis was analyzed.
Two positive predictors are finally identified, namely crossed COS and cortical involvement. First, there were 5 crossed or type IV COS patients and 3 of them (60%) deteriorated soon after onset. Crossed COS highly predicted for deterioration (Fisher exact test, p = 0.007). The odd ratio, sensitivity, and specificity were 16.25, 60.0%, and 90.1%, respectively. Second, deterioration occurred in 5 out of 12 patients (41.7%) with cortical involvement whereas 4 out of 64 patients (6.25%) with subcortical involvement. Obviously, cortical involvement also predicted for deterioration (Fisher exact test, p = 0.008). The odd ratio, sensitivity, and specificity were 10.7, 41.7%, and 93.8%, respectively.
Dizziness and dizziness-minus symptoms were experienced in 49 patients and 7 of them terminated into deterioration, whereas they were not experienced in another 27 patients in whom 2 of them suffered further deterioration. A presence of dizziness or dizziness-minus symptom did not predict for deterioration (Fisher exact test, p = 0.62). The odd ratio was 2.08.
Although cortical-type sensory impairment and paroxysm gave a high specificity for predicting cortical involvement, however, the sensitivity was low. In addition, crossed COS and cortical COS constituted only 5% and 16% of all cases of COS, respectively. Therefore, the majority of COS cannot be predicted, based simply on clinical history, neurological manifestation and associated symptom. Therefore, it is reasonable and urgent to schedule indispensable procedure, especially neuroimaging study, for COS patients.
In this series, traditional or type I COS, that is characterized by an involvement of perioral area and homolateral finger(s)/hand,1,20 does not have localizing value. Rather, the manner of paresthesia and atypical forms of COS show neuroanatomic correlation. Paroxysmal paresthesia predicted for cortical involvement. Simultaneously, type II /III COS predicts for pontine involvement whereas type IV COS for medullary involvement. COS also cannot predict for corresponding etiology. Therefore, except for crossed pattern19 or bilaterality of sensory deficits,21 COS is not an ideal localizing or etiological marker.
A deterioration of neurological condition was present in 12% of COS patients. Neurological deterioration has subsequently been mentioned in COS patients before.15,16,18,19,22,23 Therefore, COS can be a warning marker to alarm for a high possibility of grave deterioration when it presents in crossed pattern or arises from cortical involvement as found in this series. Crossed COS indicates an involvement of medulla oblongata and is an incomplete variant of Wallenberg's syndrome,19 in that infarction is due to an occlusion of vertebral artery and usually carries a high risk of deterioration and mortality.24-26 Cortical involvement usually results from a large lesion.18 These two positive predictors, therefore, are expected to increase the risk of deterioration in COS. However, the sensitivity of these predictors ranges from 41% to 60% only. Since deterioration can be prevented in some patients,18 COS should be considered an emergent condition obligatory for aggressive investigation until underlying cause is known.
In the present study, 3 patients should be emphasized because of a diagnostic trap and medicolegal risk in COS. Sjogren syndrome was in one patient. Her cheiro-oral paresthesia peaked rapidly and persisted for one week until pedal painful paresthesia developed simulating cheiro-oral-pedal syndrome. Since there was no consistent finding in head neuroimaging, a symmetric distribution of cheiro-oral-pedal paresthesia favored polyneuritis for her COS. Her paresthesia was markedly attenuated after plasmapheresis. In another two type I COS patients, one who had had subdural hemorrhage was finally found to have acute myelogenous leukemia.18 Another one who also had had subdural hemorrhage after traumatic minor head injury deteriorated one month later.15,18 These experiences indicate COS not as a simple benign neurological manifestation, therefore, should carefully be surveyed.
In conclusion, in contrast to previous concept and recent publications, COS is eventually a warning marker predicting for neurological deterioration. Clinically, a rapid neuroimaging study to exclude large infarction/hemorrhage or medullary involvement is necessary.
References
1. Sitting O. Klinische Beitrage zur Lehre von der Lokalisation der sensiblen Rindenzentren [Ger]. Prager Med Wochenschr. 1914. 45:548–550.
2. Strauss H. Über Sensibiliätsstörungen an Hand und Gesicht, Geschmacksstörungen und ihre lokalisatorische Bedeutung [Ger]. Monatsschr Psychiat Neurol. 1925. 58:265–276.

3. Garcin R, Lapresle J. [2d personal observation of a sensory syndrome of the thalamic type with cheiro-oral topography caused by localized lesion of the thalamus]. Rev Neurol (Paris). 1960. 103:474–481.
4. Kim JS. Restricted acral sensory syndrome following minor stroke. Further observation with special reference to differential severity of symptoms among individual digits. Stroke. 1994. 25:2497–2502.

5. Ngai WK, Chang YY, Liu JS, Chen SS. Cheiro-oral syndrome: identification of the lesion sites and a proposal for its clinical classification. Gaoxiong Yi Xue Ke Xue Za Zhi. 1991. 7:536–541.
6. Ten Holter J, Tijssen C. Cheiro-oral syndrome: does it have a specific localizing value? Eur Neurol. 1988. 28:326–330.

7. Nakamura M, Mizuguchi M, Momoi MY, Chou H, Masuzawa T. Transient cheiro-oral syndrome due to a ruptured intracranial dermoid cyst. Brain Dev. 2001. 23:261–263.

8. Hasegawa Y, Okada H, Okamoto S. [Neuro-Behçet disease with bilateral cheiro-oral syndrome following simultaneous multiple brain hemorrhage]. Rinsho Shinkeigaku. 1991. 31:754–759.
9. Kim JS. Cheiro-oral syndrome and vivid recollection of past in thalamic infarction. Eur Neurol. 1997. 37:253–254.

10. Mochizuki A, Eto H, Takasu M, Utsunomiya K, Schoji S. Cheiro-oral syndrome with internuclear ophthalmoplegia and cerebellar ataxia following midbrain infarction. Eur Neurol. 1994. 34:286–287.

11. Yasuda Y, Morita T, Okada T, Seko S, Akiguchi I, Kimura J. Cheiro-oral-pedal syndrome. Eur Neurol. 1992. 32:106–108.

12. Matsumoto S, Kaku S, Yamasaki M, Imai T, Nabatame H, Kameyama M. Cheiro-oral syndrome with bilateral oral involvement: a study of pontine lesions by high-resolution magnetic resonance imaging. J Neurol Neurosurg Psychiatry. 1989. 52:792–794.

13. Iwasaki Y, Kinoshita M, Ikeda K, Takamiya K, Shiojima T. Oral syndrome: an incomplete form of cheiro-oral syndrome? Int J Neurosci. 1991. 58:271–273.

14. Chang YY, Chen WH, Liu JS, Chen SS, Wu HS. Unilateral cheiro-oral syndrome in a patient with bilateral subdural hematomas. J Formos Med Assoc. 1994. 93:727–729.
15. Chen WH, Chang YY, Yin HL, Liu JS. Bilateral cheiro-oral syndrome and traumatic subdural hematoma. J Trauma. 1995. 38:826–827.

16. Chen WH, Lan MY, Chang YY, Liu JS, Chou MS, Chen SS. Bilateral cheiro-oral syndrome. Clin Neurol Neurosurg. 1997. 99:239–243.

17. Chen WH, Tseng YL, Lui CC, Liu JS. Episodic pain syndrome restricted cheiro-oral region associated with pontine lesion. Brain Inj. 2005. 19:949–953.

18. Chen WH, Lan MY, Chang YY, Lui CC, Chen SS, Liu JS. Cortical cheiro-oral syndrome: a revisit of clinical significance and pathogenesis. Clin Neurol Neurosurg. 2006. 108:446–450.

19. Chen WH, Li TH, Chen TH, Lin HS, Hsu MC, Chen SS, et al. Crossed cheiro-oral syndrome. Clin Neurol Neurosurg. 2008. 110:1008–1011.

20. Fujisawa A, Imaizumi M, Nukada T. [Clinical study of cheiro-oral syndrome (author's transl)]. Rinsho Shinkeigaku. 1979. 19:17–21.
21. Yasuda Y, Watanabe T, Tanaka H, Ogura A. Localizing value of bilateral cheiro-oral sensory impairment. Intern Med. 1998. 37:982–985.

22. Hashiguchi K, Igata A. [A case of primary pontine hemorrhage with cheiro-oral syndrome (palm-oral sensory disturbance)]. Shinkei Naika. 1976. 5:79–80.
23. Ide M, Yamamoto M, Jimbo M, Enomoto N. [Cheiro-oral syndrome with pontine infarct--report of a case]. No To Shinkei. 1985. 37:181–186.
24. Kim JS, Lee JH, Lee MC. Patterns of sensory dysfunction in lateral medullary infarction Clinical-MRI correlation. Neurology. 1997. 49:1557–1563.

25. Kumral E, Afsar N, Kirbas D, Balkir K, Ozdemirkiran T. Spectrum of medial medullary infarction: clinical and magnetic resonance imaging findings. J Neurol. 2002. 249:85–93.

26. Norrving B, Cronqvist S. Lateral medullary infarction: prognosis in an unselected series. Neurology. 1991. 41:244–248.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download