Abstract
Purpose
The implementation of medical professionalism in education and evaluation is a recent trend in medical education. Although many studies on the subject have been carried out, they have generally been not focused specifically on the level of medical student professionalism, and the perception gaps between medical students and professors on this topic remain unresolved. This study attempts to determine whether such gaps exist.
Materials and Methods
Two hundred fifty fourth-year medical students and 53 professors who were randomly selected from 41 medical schools were asked to complete a survey on the level of the professionalism of medical students. Using 31 core professionalism elements that are required for Korean medical students, students self-assessed their level of professionalism, and professors evaluated the professionalism level of medical students who were about to graduate.
Results
Of the 31 core elements, significant perception gaps were found in 28 elements. The three domains into which the 31 core elements were divided - professional knowledge, professional skills, and professional attitude - all contained perception gaps, and professors' ratings generally were higher than those of the students, a noteworthy observation.
Conclusions
Medical professors need to encourage their students to elevate their professionalism. Furthermore, what the faculty think that they have taught regarding professionalism may not be fully assimilated by students. Therefore, further research is essential to determine the cause of such perceptional differences.
Modern health care requires physicians to collaborate with diverse professionals such as nurses, physician assistants, pharmacists, dietitians, physical therapist, and psychologists in order to provide interdisciplinary health services.1 Medical students need to participate in active learning to acquire the life-long learning skills which are necessary to accommodate the explosion of information in this new era, as well as to foster clinical reasoning and interactive skills.2 In the 1970s, commercialism was introduced into health services, challenging physicians' professional authority.3 Such an atmosphere necessitates an improvement in the doctor-patient relationship. This change gave medical educators the task of training medical students in communication and medical professionalism, which are important in developing good doctor-patient relationships.
In the modern era, the medical education community has emphasized the teaching and evaluation of medical professionalism.4-7 Steinert, et al.4 argued that the traditional method of transmitting professional values by role modeling is no longer adequate, and that professionalism must be taught and evaluated explicitly. Cruess5 suggested the use of situated learning theory to help students internalize professional values and behaviors. Goldie, et al.6 underscored the fact that teaching professionalism in the early years of medical curriculum is important - early clinical contact is an important part of the process of socialization, as it allows students to enter the community of practice that is the medical profession. And the role models can contribute powerfully to students' learning and identify formation. Recently, a comparative study of professionalism in medical students identified ten core elements of medical professionalism.7
Hur, et al.7 pointed out that, in order to provide an adequate curriculum on medical professionalism, the concept of professionalism needs to be properly investigated at the institutional level. To assess this, the status of the current professionalism - related curriculum as well as the level of students' professionalism should be examined. Although many studies deal with the concept of medical professionalism, few research results are available on the level of professionalism in medical students.
The current study goes one step further than my previous study.7-9 I measured the level of medical students' professionalism as assessed by medical school professors and compared them with the students' own perception of their level of professionalism. I wanted to determine whether there were any differences between medical students' and professors' perception of students' professionalism. And, if so, whether the ten core elements of medical professionalism also showed differences.
Eight of the 41 medical schools in Korea were chosen based on region and institution type. Five schools were located in the capital city, Seoul and three were placed in rural areas. Five schools were private institutions, and three were national. From these eight schools, 250 4th year medical students and 53 professors, chosen at random, answered the questionnaire. The questionnaire for medical professors was designed in a five-point Likert scale (1 = "very low", 2 = "low", 3 = "average level", 4 = "high", 5 = "very high") to assess the level of 31 elements of medical students' professionalism which were defined in my previous study.7 These 31 elements, including basic knowledge of training primary medicine, understanding medical humanities and social science, understanding health policy, understanding medical history & Korean society, understanding of alternative medicine, basic skills for training primary medicine, self-restraint, planning, physical & mental health, lifelong learning, intimacy, leadership, teamwork, communication skills, foreign language skills, logical & critical thinking skills, creative thinking skills, problem solving skills, decision-making skills, service oriented, respect for others, caring attitude towards patients, etiquette, medical ethics, self-confidence, integrity & diligence, sense of duty, religious & dilettante life, open & positive mind, self-examination, and physical appearance of medical professionalism. And they were categorized into three domains-professional knowledge, professional skills, professional attitude. The definition of each element was explained in detail in order to minimize unnecessary perception gaps between professors and students. Importance ranks were also measured by professors in five-point Likert scale (1 = "not important at all", 2 = "unimportant", 3 = "average level", 4 = "important", 5 = "very important"). From this, top ten core elements were picked to compare the perception of students' level of these elements between professors and students.
Descriptive statistical analysis and independent t-tests were done with the SPSS program. Two medical education experts certified the validity of the survey for professors, and the questionnaire was quite reliable as the Cronbach's alpha score was 0.90.
The self-assessed medical professionalism level of graduating students and professors' assessments are shown in Table 1. The total score differed significantly (t = 9.40, p = .000), with students' self-assessed mean level being slightly higher than professors' assessment.
There were significant assessment differences in the elements of professional knowledge, with the exception of the 'understanding health policy' element. Most of students' self-assessed mean scores were higher than the scores given by professors (Table 2).
Perception gaps were shown in 12 of the 14 elements of professional skills (Table 3). The students' self-assessed scores were higher than their teachers' in all elements. The professors' mean scores did not exceed 3.0, indicating that the graduating medical students did not have sufficient professional skills whereas the students assessed themselves as slightly above average level. The mean difference in professors' and students' assessments in the professional skills domain was 0.48.
In the professional attitude domain, there were perception gaps in all twelve elements (Table 4). The biggest gap was in 'respect for others (t = 10.28, p < .001)', followed by 'sense of duty' (t = 8.46, p < .001) and 'caring attitude towards patients' (t = 8.42, p < .001. The gaps between the students' and professors' perceptions were quite large, with a mean difference of 0.77 points. The students regarded their professionalism level as slightly above 'average (mean=3.0)', but professors ranked the students as below 'average' level.
Overall, there were significant perception gaps between students and professors in all three domains (professional knowledge, skills, and behavior). I found differences in 27 of the 31 core elements; the students' self-assessed level of professionalism was higher than the professors' perception.
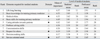
The professors ranked top ten core elements in terms of importance; from most important to least. They were: 'life-long learning', 'basic knowledge for training primary medicine', 'medical ethics', 'basic skills for training primary medicine', 'caring attitudes towards patients', 'problem-solving skills', 'communication skills', 'respect for others', 'decision-making skills', and 'service-oriented mind' (Table 5).
Comparing the core ten elements with the top ten elements which students ranked the highest, some interesting results emerged. The 'basic knowledge for training-primary medicine' element ranked as the second in importance by the professors; students' level of this element ranked the second among 31 elements, and the professors also thought that this element was best learned. For the most important core element, 'life-long learning', the mean score of this element ranked only 11th (self-assessed by students) and 9th (professors' assessment score). And the third most important element, 'medical ethics', was next to the last in students' self-assessment and ranked 18th by the professors. Among the ten core elements only two elements ('basic knowledge for training primary medicine' and 'basic skills for training primary medicine') ranked in top ten by both students and professors. All of the professional attitude elements' that were in the top ten were self-assessed as comparatively very low level.
Medical professionalism is an essential requirement for medical doctors. Despite such importance, not all the essential professional qualities are adequately taught and learned. In addition, there are gaps in the perception of how well these qualities are acquired by students. Such perception gaps are useful resources for assessing and improving medical education curricula. In the development of curriculum, a thorough assessment of needs with a clear understanding of the students' current level is essential.10 Understanding of strengths and weaknesses in the elements of professionalism of our students could possibly indicate the parts of the curriculum which need change or improvement.
A closer look at the research results reveals that, in the professional knowledge domain, the biggest gap was seen in 'understanding of alternative medicine', and students' level assessed by professors was very low. Medical students need to have a sufficient knowledge of alternative medicine.11 Because the concept of alternative medicine differs in different cultures, the medical school curriculum must provide accurate and adequate information on alternative medicine and its' practical use.
In the professional skills domain, the biggest differences were seen in 'communication skills' and 'intimacy'. Because communication skills are basic and essential for physicians, a careful consideration of the systematic approach to organizing communication skills learning is necessary.12 Students self-assessed their level of intimacy as insufficient, implying that we need to develop learning techniques that foster intimacy. 'Intimacy' is very difficult to acquire in traditional lecture-based instruction. A suggested approach is to adopt programs using standardized patients, small group learning and team-based learning; this enhances intimacy between coworkers, but also enhances group cohesiveness, teamwork, and communication skills.13 In a previous study of pre-medical students,6 the biggest perception gap in the professional skills domain was in 'teamwork'. In my current study, students also regarded their 'teamwork' skills as lower than average level. Although the self-assessed 'teamwork' scores rose to slightly above average level by the time when students graduated, the professors' assessment was still below average level. These results are disappointing, considering that teamwork is one of the essential elements required for the doctors in the 21st century; many experts agree that majority or even the entire academic course in medical education should be devoted to teamwork.14-17
The largest gap was seen in the professional attitude domain. The 'respect for others' element had the biggest gap among 31 elements. This finding is in agreement with earlier findings6 in pre-medical students. In today's patientcentered health care, a respectful attitude is one of the basics of clinical medicine.7,18-20 Perception gaps were observed in all domains and in the majority of core elements. Further research is essential to determine the cause of such differences in perception. Moreover, since the students' professionalism level is unsatisfactory, we need to find a way to improve the situation through changes in the curriculum.
The sample size in this study limits the ability to generalize the results. However, there were some interesting trends which highlight the need for further research, including an analysis of the factors that affect the level of medical professionalism. For example, it would be interesting to find whether the level of professionalism changes depending on students' academic achievements, age, and club membership. Identification of students who are satisfied with the professionalism education which they receive, how students acquire their professional attitude, and determination of which academic years the 31 core elements were best learned are also important goals for future research.
Figures and Tables
References
1. Kim S, Hur Y. Medical Professionalism in the 21st Century: How can we teach it? Korean J Med Educ. 2003. 15:171–186.

2. Kasar J, Clark NE. Developing professional behaviors. 2000. New York, NY: Slack Inc.
3. Park J. Medical students' attitudes toward the patient-doctor relationship. Korean J Med Educ. 2007. 19:215–223.

4. Steinert Y, Cruess S, Cruess R, Snell L. Faculty development for teaching and evaluating professionalism: from programme design to curriculum change. Med Educ. 2005. 39:127–136.

5. Cruess RL. Teaching professionalism: theory, principles, and practice. Clin Orthop Relat Res. 2006. 449:177–185.
6. Goldie J, Dowie A, Cotton P, Morrison J. Teaching professionalism in the early years of a medical curriculum: a qualitative study. Med Educ. 2007. 41:610–617.

7. Hur Y, Lee SH, Kim S. Medical students' self assessment on medical professionalism. Korean J Med Educ. 2008. 20:23–35.

8. Hur Y. Core elements of medical professionalism for medical school applicants. Korean J Med Educ. 2006. 18:297–307.

9. Hur Y, Kim S. What qualities do medical school applicants need to have?: secondary publication. Yonsei Med J. 2009. 50:427–436.

10. Lee SH. Curriculum development and evaluation. 2004. Seoul: Yangseowon.
11. Hong SJ, Kim YA. An analysis of trends in reports on alternative medicine in general dailies. J Korean Soc Med Inform. 2005. 11:353–360.

12. Kim S, Lee SJ, Choi CJ, Hur Y. The effectiveness of communication skills of pre-medical students. Korean J Med Educ. 2006. 18:171–182.
13. Michaelsen LK, Parmelee DX, McMahon KK, Levine RE. Team-based learning for health professions education: a guide to using small groups for improving learning. 2008. Sterling, Virginia: Stylus Publishing.
14. O'Connell MT, Pascoe JM. Undergraduate medical education for the 21st century: leadership and teamwork. Fam Med. 2004. 36:S51–S56.
15. Thompson DA, Cowan J, Holzmueller C, Wu AW, Bass E, Pronovost P. Planning and implementing a systems-based patient safety curriculum in medical education. Am J Med Qual. 2008. 23:271–278.

16. Macaulay JO, Nagley P. Student project cases: a learner-centred team activity broadly integrated across the undergraduate medical curriculum. Med Teach. 2008. 30:e23–e33.

17. McNair RP. The case for educating health care students in professionalism as the core content of interprofessional education. Med Educ. 2005. 39:456–464.

18. Choi CJ, Kim JM, Park YG. Patient-centered attitudes and communication skills in medical students after clerkship. Korean J Med Educ. 2004. 16:169–177.

19. Haidet P, Kelly PA, Bentley S, Blatt B, Chou CL, Fortin AH 6th, et al. Not the same everywhere. Patient-centered learning environments at nine medical schools. J Gen Intern Med. 2006. 21:405–409.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download