Abstract
Purpose
To observe changes in audiology, intellectual development, behavior development, and physical growth during systematic follow-up of infants with asymptomatic congenital human cytomegalovirus (HCMV) infection.
Materials and Methods
Fifty-two infants diagnosed with asymptomatic congenital HCMV infection from July 2003 to July 2007 served as the infection group, and 21 healthy infants served as the control group. All infants were confirmed to have HCMV infection by Fluorescent Quantative polymerase chain reaction (FQ-PCR). In both the infection and control groups, the neonates and infants at 3 months, 6 months, and 1 year of age underwent examinations.
Results
1) 20 items of National Black Nurses Association (NBNA) scores of neonates 12-14 days after birth in 2 groups were 38.3 ± 1.95 and 38.5 ± 2.29, without significant differences. 2) Auditory test: 50 ears of 25 cases in the infection group showed abnormal auditory thresholds in V waves with an abnormal rate of 14%, while no abnormalities were found in 21 cases in the control group. 3) Mental and psychomotor development index scores in the control group (107.49 ± 11.31 and 107.19 ± 10.98) were compared with those in 41 asymptomatically infected infants at 1 year of age (107.21 ± 9.96 and 108.31 ± 11.25), and no statistically significant difference was noted.
Conclusion
1) An elevated threshold in the V wave was present in asymptomatically infected infants, but could not be detected through otoacoustic emission (OAE) screening. 2) Either in the neonatal or infant periods, asymptomatic congenital HCMV infection did not have a significant influence on nervous behavior or on physical and intellectual development.
Human cytomegalovirus (HCMV) is one of the most common viruses they can be transmitted through the placenta. Congenital HCMV infection has been a focus of perinatal medicine, pediatrics, and virology in recent years. In pregnant women, the incidence of HCMV infection in China accounts for more than 90%, while, the incidence in infants is 1%. Domestic and foreign large-scale studies have shown that 10% of newborns with congenital HCMV infection, are symptomatic and have clinical symptoms at birth, while 90% are asymptomatic. Developing countries have a higher incidence of HCMV infection than developed countries.1-4 However, little attention has been focused on the influence of congenital HCMV infection on children's physical growth and intellectual development. By following-up asymptomatically infected infants from July 2003 to July 2007, we investigated changes in audiology, nervous behavior, intellectual development, and behavioral development in order to find out the impact of asymptomatic congenital HCMV infection.
Fifty-four term neonates who came from the newborn nursery and obstetric ward from July 2003 to July 2007 were diagnosed with asymptomatic congenital HCMV infection in the first two weeks after birth. Fifty-two cases were selected and enrolled in the infection group as previously described, including 30 boys and 22 girls with an average birth weight of 3.39 ± 0.31 kg, whereas 21 cases served as the control group, including 11 boys and 10 girls with an average birth weight of 3.31 ± 0.38 kg.
In this study, congenital HCMV infection was diagnosed if HCMV-DNA of blood cell (WBC) is positive in 14 days. Asymptomatic congenital HCMV infection was identified according to the American Fowler criteria5 and the following conditions:
1) At least 1 positive result for HCMV-immunoglobulin M (IgM) or HCMV-DNA was detected in the mother's blood, urine, or breast milk.
2) 14 d after birth, positive HCMV DNA was found in white blood cell (WBC) in infants, while results of other virologic investigation by Toxoplasma Other Rubella Virus Cytogegalo Virus, Herpes Simplex Virus-II-polymerase chain reaction (TORCH-PCR) were negative (without rubella virus, toxoplasmosis, herpes simplex virus, and others).
3) HCMV-infected infants with the following clinical symptoms were ruled out: ecchymosis, thrombocytopenia, hepatosplenomegaly, hyperbilirubinemia caused by direct increase of bilirubin, and microcephalia.
HCMV-infected infants with the following diseases were excluded: severe asphyxia, hypoxic-ischemic encephalopathy (HIE), central nervous system infection, congenital malformation, family history of hearing impairment, receiving ototoxic drug, or receiving mechanical ventilation.
Infants in the control group were at the same stage as the infection group. Precautions were implemented to ensure that all control group conditions were the same as those of the infection group, with the exception of a negative result upon cytomegalovirus infection examination.
Two mL venous blood of infants were obtained immediately after admission and stored at -20℃ for further detection.
Primers used for HCMV-DNA amplification were as follows: p1 5'-TTT ABA TAT CCT ABA TAA GGT TCA T-3' and p2 5'-TCT TAA AAB ATC TTC TGG GAA TAA GTC-3', with a length of 235 bps products. Fluorescent probe sequence was 5'-ABC CAT CC CAT CTC CCGG CTT ATC CTC-3'. Quality control was performed in strict accordance with operating manual instructions. The automatic fluorescence gene analyzer PE-5700 was provided by Whatman Biometra Company, Germany.
In 2 groups, infants at the neonatal stage underwent 20 neonatal behavioral neurological assessment (NBNA) items. Follow-up occurred at 3 months, 6 months, and 1 year of age, distortion product otoacoustic emission (DPOAE) and auditory brainstem responses (ABR) were conducted to determine hearing loss. At the same time, Bayley Scales of Infant Development Assessment, physical examination, and motor nerve inspection were used to determine intellectual and physical development. The examiners were blinded as to which infants were in the control group and which infants were in the infection group for both hearing and intelligent quotients. Some infants were examined with cranial B-ultrasonography and CT scan.
Five parts (20 items) of the NBNA, including behavioral ability, active muscular tension, passive muscle tension, primitive reflexes, and general condition, were performed on infants at 12 to 14 d after birth. Each of item had 3 graduations in scores 0, 1, and 2, with total score of 40 points.
This was performed in a quiet room by a trained examiner. When examined, the diseased child was quiet and in a sleeping state (without the use of sedative drugs). The external auditory canal was conventionally cleaned, after which a suitable detecting head was placed in the canal with its tip-pinhole aimed at the eardrum.
Doctors specialized in ear nose and throat (ENT) department were responsible for the operation and judgment of results. ABR examination was conducted at 3 to 6 months of age after birth by using auditory evoked potential diagnostic systems (Smart Ep) provided by the American Hearing Company (HIS). After taking sedatives, the sleeping infants were examined in an echoic room.
Separate criteria for the impairment of hearing function were as follows: mild (hearing threshold, 26-40 dBHL), moderate (hearing threshold, 41-55 dBHL), moderate to severe (hearing threshold, 56-70 dBHL), severe (hearing threshold, 71-90 dBHL), and extremely severe (hearing threshold, above 90 dBHL).
The Bayley Scales of Infant Development Assessment comprise an intelligence scale and movement scale which were used by a trained examiner to determine infants' intellectual and physical development. The first and second examinations were performed at 6 months and 1 year after birth, respectively.
Many factors, such as family structure, economic situation, educational background of parents, children's guardian's educational background, and children's early education, can have an impact on children's intellectual development. For this reason, the aforementioned factors in the two groups were compared. However, no significant differences were found. Moreover, no significant differences existed in the physical examination between the two groups. Some signs and symptoms, including bleeding tendency, thrombocytopenia, jaundice, and hepatosplenomegaly, were not observed in both groups.
Infants scores 12 to 14 d after birth in the 2 groups were 38.3 ± 1.95 and 38.5 ± 2.29, respectively, without significant differences (t = 0.88, p > 0.05).
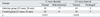
Twenty five cases between 3 months and 6 months of age in the infection group were examined with ABR. Seven ears of 5 cases showed mild abnormal auditory thresholds in V waves with an abnormal rate of 14%, while no abnormalities were found in 21 cases in the control group. Therefore, the difference between the 2 groups was statistically significant. Five ears in 4 cases in the infection group showed prolonged intervals in I-V waves, whereas 3 ears in 2 cases in the control group showed this abnormality without apparent differences. All infants with the increased V wave threshold were subjected to OAE inspection during the neonatal period (Table 1).
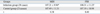
The Bayley Scales of Infant Development Assessment were performed in 41 cases in the infection group at year 1. No significant differences in mental development index (MDI) and psychomtive development index (PDI) were found between the infection and control groups (Table 2).
Considerable diversity in HCMV infection rates (ranging from 82.5% to 95%) appears to occur in child-bearing women of different geographic regions and different ethnic backgrounds. In China, the HCMV infection rate of pregnant women is more than 90%.1 It differs from other viruses with easy vertical transmission such as rubella as HCMV can be transmitted to the fetus even if preconception maternal immunity is present. Congenital HCMV infection is found in approximately 1% of neonates in China, of which 10% are symptomatic and 90% are asymptomatic. If China's annual birth of newborns is 17 to 20 million, it is estimated that nearly 200,000 neonates each year are born with congenital HCMV infection, of which approximately 180,000 have asymptomatic infections. Therefore, this population requires further attention.
Symptomatically congenital HCMV-infected infants have poor prognoses. It has been reported that 30% of diseased children die, while the other 70% have central nervous system impairment of different degrees, including mental retardation, movement disorders, and sensorineural hearing loss (SNHL). It is generally thought that symptomatic congenital HCMV infection is a major cause of death and disablement in children with intrauterine infections. Some research has shown that antiviral therapy for symptomatically infected infants could indeed reduce the incidence of central nervous system sequelae.6 Regarding asymptomatic infection, which affects the highest proportion of infants with congenital HCMV infection, problems related to infected children's growth and early clinical use of antiviral drugs remains unclear.
Our study indicated that asymptomatic congenital HCMV infection had an impact on infant hearing. The ABR abnormality presented mainly as a slightly increased threshold in the V wave (accounting for 14.0%), which was similar to most studies reported abroad. Through comparison with a control group which consisted of siblings or randomly selected children, Fowler, et al.5 reported that SNHL was only found in the infection group, with the infection rate being 7.2%. Numazaki and Fujikawa3 found that, among 17 cases of asymptomatic congenital HCMV infection, 2 children developed late-onset SNHL, including 1 case of moderately binaural hearing loss and 1 case of unilateral hearing loss. In addition, asymptomatic congenital HCMV infection can display delayed and fluctuation phenomena in hearing problems, as described in other studies. Because of the short time used for audiological observation in this study, we did not observe these phenomena. The mechanism of hearing impairment in children with asymptomatic congenital HCMV infection remains unknown at present.
Early examination should be done to screen for HCMV. However, most countries do not undertake HCMV screening, therefore, most congenital HCMV infection, especially congenital asymptomatic infection, would forgo diagnosis due to no obvious clinical manifestations. At present, OAE is commonly used in clinics to screen newborns for hearing loss. However, not all SNHL cases can be detected by OAE, resulting in a lack of early diagnosis of SNHL. Therefore, it is necessary to perform HCMV screening for infants and hearing tests for congenital HCMV-infected newborns. Some scholars believe that urine CMV-PCR testing is convenient and simple,7 and can be used as a supplement for conventional laboratory tests.8
Some factors influencing infant IQ were excluded, including children's family structure, economic situation, pregnancy age, educational background of the parents, body mass of the parents, and children's early education, as well as the children's guardians and their educational background. By following up asymptomatically-infected infants using Bayley Scales of Infant Development Assessment, we found that either MDI or PDI in the control and infection groups had no statistically significant difference. The results agreed with the consequence proposed by Sten-A,9 namely that asymptomatic congenital HCMV infection did not have a significant influence on total IQ of the infants.
Figures and Tables
References
1. Fowler KB, Stagno S, Pass RF. Maternal immunity and prevention of congenital cytomegalovirus infection. JAMA. 2003. 289:1008–1011.

2. Yamamoto AY, Figueiredo LT, Mussi-Pinhata MM. [Prevalence and clinical aspects of congenital cytomegalovirus infection]. J Pediatr (Rio J). 1999. 75:23–28.

3. Numazaki K, Fujikawa T. Chronological changes of incidence and prognosis of children with asymptomatic congenital cytomegalovirus infection in Sapporo, Japan. BMC Infect Dis. 2004. 4:22.

4. van der Sande MA, Kaye S, Miles DJ, Waight P, Jeffries DJ, Ojuola OO, et al. Risk factors for and clinical outcome of congenital cytomegalovirus infection in a Peri-Urban West-African Birth Cohort. PLoS ONE. 2007. 2:e492.

5. Fowler KB, McCollister FP, Dahle AJ, Boppana S, Britt WJ, Pass RF. Progressive and fluctuating sensorineural hearing loss in children with asymptomatic congenital cytomegalovirus infection. J Pediatr. 1997. 130:624–630.

6. Kimberlin DW, Lin CY, Sánchez PJ, Demmler GJ, Dankner W, Shelton M, et al. Effect of ganciclovir therapy on hearing in symptomatic congenital cytomegalovirus disease involving the central nervous system: a randomized, controlled trial. J Pediatr. 2003. 143:16–25.
7. Schlesinger Y, Halle D, Eidelman AI, Reich D, Dayan D, Rudensky B, et al. Urine polymerase chain reaction as a screening tool for the detection of congenital cytomegalovirus infection. Arch Dis Child Fetal Neonatal Ed. 2003. 88:F371–F374.

8. Espy MJ, Uhl JR, Sloan LM, Buckwalter SP, Jones MF, Vetter EA, et al. Real-time PCR in clinical nicrobiology: applications for routine laboratory testing. Clin Microbiol Rev. 2006. 19:165–256.

9. Ivarsson SA, Lernmark B, Svanberg L. Ten-year clinical, developmental, and intellectual follow-up of children with congenital cytomegalovirus infection without neurologic symptoms at one year of age. Pediatrics. 1997. 99:800–803.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download