Abstract
Purpose
There is a paucity of information on the serum soluble vascular endothelial growth factor receptor-2 (sVEGFR-2) concentrations, membranous VEGFR-2 expression and the mechanism involved in their modulations during the clinical onset of pre-eclampsia. This cross-sectional study was conducted to evaluate the concentration of sVEGFR-2 in serum and to investigate the expression of membranous VEGFR-2 in placentae of pre-eclampsia group.
Materials and Methods
The serum levels of sVEGFR-2 (n = 120) and the expression of membranous VEGFR-2 in placentae (n = 100) were analysed at third trimester of pregnancy by enzyme linked immunosorbent assay (ELISA) and immunohistochemistry respectively. The diagnostic parameters of sensitivity, specificity and association of soluble and membranous VEGFR-2 in these patients were evaluated.
Results
The serum levels of sVEGFR-2 in pre-eclampsia patients were found to be significantly reduced (p = 0.01, p = 0.001) in early and late pre-eclamptic sub-groups as compared to their respective third trimester control sub-groups. Also, the receiver operating characteristic (ROC) curve analysis showed a cut-off value of 7350.4 pg/mL, higher sensitivity (76%) and specificity (76%) for sVEGFR-2 in late onset (> 34 weeks) pre-eclamptic group. Significant down-regulation of membranous VEGFR-2 immunoreactivity was observed in all the placental cells (p = 0.0001) at > 34 weeks preeclamptic group.
Conclusion
The reduced serum levels of soluble VEGFR-2 and the down-regulated expression of membranous VEGFR-2 in the study group denoted abnormality in VEGF mediated placental function in all placental cells and thus VEGFR-2 may be a key factor, intimately associated with pre-eclampsia. This study shows the clinical utility of soluble and membranous VEGFR-2 in pre-eclampsia patients.
Pre-eclampsia is a life threatening complication of pregnancy which contributes to maternal and perinatal morbidity and mortality.1 The exact pathogenesis of preeclampsia remains unclear. It has been suggested that endothelial dysfunction may play a central role in the development of pre-eclampsia. Impaired trophoblastic invasion of the maternal placental bed is considered to be the initial event of endothelial dysfunction in pre-eclampsia. Uterine artery Doppler abnormalities are suggestive of increased impedance to blood flow in the uterine circulation2 as well as a failure of physiologic transformation of the spiral arteries diagnosed by examination of placental bed biopsies.3 Consequently, reduction of uteroplacental blood perfusion by shallow implantation results in local placental hypoxia. A hypoxic/ischemic placenta may then release placental factors into maternal circulation eventually causing endothelial dysfunction, which leads to the main clinical symptoms of pre-eclampsia. The identification of circulating factors that mediate endothelial dysfunction has been of great research interest for decades. Vascular endothelial growth factor (VEGF) is necessary to maintain normal endothelial health in the adult vasculature, which extends beyond angiogenesis. VEGF is a dimeric glycoprotein with potent angiogenic properties and promotes endothelial cell proliferation, migration and survival and exerts biologic effects through two high-affinity tyrosine kinase receptors i.e. Vascular endothelial growth factor receptor-1 (VEGFR-1) / fms-like tyrosine kinase-1 (flt-1) and Vascular endothelial growth factor receptor-2 / kinase insert domain containing receptor (KDR) / fetal liver kinase-1 (Flk-1). VEGFR-1 is considered to be a 'decoy' receptor and VEGFR-2, the major mediator of the mitogenic, angiogenic, permeability enhancing4 and endothelial survival effects of VEGF. Both VEGFR-1 and VEGFR-2 have two isoforms: a membranous isoform and a soluble isoform.
Both receptors share common features such as seven immunglobulin-like extracellular domains, a single transmembrane region and a consensus tyrosine kinase sequence interrupted by a kinase insert domain, and are highly glycosylated.5,6 Although VEGFR-1 binds to VEGF with substantially higher affinity, most of the biological effects of VEGF seem to be mediated via VEGFR-2.7
The effect of blockage of VEGF action on the pathophysiology of pre-eclampsia has been suggested recently by several studies in both animals and humans. Administration of anti-VEGF compounds can induce hypertension and proteinuria in non-pregnant animals8 and humans enrolled in anti angiogenic trials.9 Furthermore, anti-VEGF therapy in patients with cancer has been associated with hypertension, proteinuria and the reversible posterior leukoencephalopathy syndrome, all of which are the hallmarks of pre-eclampsia and eclampsia.10,11
Accumulating evidence suggests that a balance among VEGF, placental growth factor (PLGF) and their receptors is important for effective vasculogenesis, angiogenesis and placental development during pregnancy. In our previous study on pre-eclampsia, a significant up-regulation of soluble and membranous VEGFR-1 was observed.12 Recently, sVEGFR-2 has been detected in human plasma.13 The recombinant form of this protein has anti-angiogenic activity.14 Plasma sVEGFR-2 concentrations are lower in patients with systemic lupus erythematosus disease15 and higher in those with acute leukemia, compared to healthy controls.16 There is a paucity of information on serum sVEGFR-2 concentrations, placental VEGFR-2 expression, and the mechanisms involved in their modulations before and during the clinical onset of pre-eclampsia.17 Therefore, a cross-sectional study was undertaken to appraise the serum soluble VEGFR-2 concentration as well as placental membranous VEGFR-2 changes in pre-eclampsia and their coalition with the disease.
One hundred and twenty volunteers for this cross-sectional study were recruited from the out patient department (OPD) clinic between the years 2004 to 2006 from the Department of Obstetrics and Gynaecology, Safdarjang Hospital, after obtaining written consent from patients. The Research and Ethics Committee of Vardhman Mahavir Medical College and Safdarjang Hospital (New Delhi, India) approved the study. Pre-eclampsia was defined as diastolic blood pressure above 90 mmHg and systolic blood pressure above 140 mmHg in at least two consecutive measurements, six hours apart, oedema and proteinuria ≥ 300 mg in a 24 hour urine collection or ≥ 1+ dipstick on a random urine sample. Patients with a history of hyperten-sion, or any renal disease pre-eclampsia were excluded from the study. Healthy pregnant women with uncompli-cated pregnancies without any history of chronic medical illness served as the control group. All the subjects were classified and numbered subsequently before any laboratory analysis to avoid bias in results.
A total of 120 serum samples were collected, of which 20 were from non-pregnant women, and 50 from third trimester pre-eclampsia patients were compared with 50 gestationally matched uncomplicated pregnant women (control group). Blood samples from pre-eclampsia patients were collected after the manifestation of disease. The samples from control group were matched with study groups by gestational weeks. Serum was separated by centrifugation and stored at -80℃ till analysed.
One hundred placentae were collected from patients of normotensive third trimester control group (n = 50) and pre-eclampsia group (n = 50). Tissues were randomly sampled from each placenta and were immersion-fixed in 10% formalin and embedded in paraffin.
All the tissue and serum samples were sub-classified as either early pre-eclampsia (≤ 34 weeks) or late preeclampsia (> 34 weeks) disease, as well as gestationally matched preterm (≤ 34 weeks) and term (> 34 weeks) control group according to the gestational age.
Serum levels of sVEGFR-2 in all the samples were quantified by enzyme linked immunosorbent assay (ELISA; Quantikine human soluble VEGFR-2, R&D Systems Europe Ltd, Barton Lane, Abingdon Science Park, Abingdon, United Kingdom). All assays were performed in respective duplicate samples. ELISA employs a quantitative sandwich immunoassay technique. Briefly, recombinant human VEGFR-2 standards and maternal plasma specimens were incubated in duplicate wells of the microtiter plates pre-coated with monoclonal antibodies specific for VEGFR-2. After an incubation period, the assay plates were subjected to a wash step to remove unbound antibody-enzyme reagent. Then, an enzyme-linked polyclonal antibody specific to VEGFR-2 was added to the wells. Following a wash to remove any unbound antibody-enzyme reagent, a substrate solution (tetramethyl-benzidine) was added to the wells. Colour developed in the assay plates, proportionally to the amount of VEGFR-2 bound in the initial step. The optical density was determined by subtracting readings at 540 nm from readings at 450 nm. The protein levels were calculated using a standard curve derived from a known concentration of respective recombinant proteins. The minimum detection dose of assays was 3.5 pg/mL. The inter and intra-assay coefficients of variation were 6.5% and 3.5%, respectively. The sensitivity of the assay was 4.6 pg/mL. Assays were performed by personnel who were unaware of the outcome of the pregnancy. Samples were randomly ordered for analysis.
Serial sections of each tertiary villi of placental tissue were collected on poly-L-lysine coated slides (Sigma, St. Louis, MO, USA), dewaxed, and dehydrated, and antigen retrieval treatment was carried out in a water bath at 100℃ for 20 minutes. After washing in 0.01M Tris buffered saline (pH-7.4), sections were then incubated with primary monoclonal anti-human anti body of VEGFR-2 (Flk-1, A-3, sc-6251, Santa Cruz Biotechnology, Inc., Delaware Avenue, Santa Cruz, USA) at a dilution of 1 : 100 and incubated at 4℃. Sections were then washed with 0.05% Tween-20 in 0.01M TBS. The sections were incubated in secondary antibody for 45 minutes at room temperature, followed by incubation with biotinylated link antibody and peroxidase-labelled streptavidin for 45 minutes (LSAB + System-HRP, Dako Cytomation, Glostrup, Denmark). Staining was completed after incubation with substrate-chromogen solution (liquid DAB, Dako, Code: K0679) and was applied until the maximum level of reaction product was obtained. Sections were then counter-stained with Mayer's haematoxylin solution and mounted with disterene dibutyl phthalate xylene (DPX). Negative control stainings were performed using IgG non-immune serum (Dako) in all the slides and for positive control; rabbit anti-human choriogonadotropin(hCG, A-023102, Dako, Denmark) was used to identify trophoblast, endothelial and Hofbauer cells. Photomicrographs were taken under an Olympus microscope [(model BX-51) Olympus America, Inc, Melville, NY, USA)], and the images were captured by charge coupled device (CCD) camera and an "Olysia Bio-report" software-linked personal computer. Tissue sections were evaluated for protein localization and intensity. The intensity of immunoreactivity was semi-quantitatively evaluated as follows.
Positively stained cells were grouped according to the following categories: (no staining), +1 (weak, but detectable), +2 (moderate), +3 (intense). In each slide, five different areas were evaluated under a microscope using 400× original magnification. For each tissue, an H-score value was calculated by adding the percentage of cells grouped in one intensity category and multiplying this number with the weighed intensity of the staining, using the formula Hscore = Pc (s + 1), where s represents the intensity scores and Pc is the corresponding percentage of the cells. In each slide, five different areas were evaluated under a microscope using 400× magnification.18 All tissues were examined by three observers who were blinded to the slides (i.e. patient's identity, clinical details and gestational ages).
Statistical analysis was performed using statistical software STATA 9.0 (College station, Texas, USA). Data were presented as number (%), and mean ± SD as the requirement. The difference in means among the groups was compared using Mann-Whitney test / One Way ANOVA / Kruskal-Wallis test with Bonferroni correction.
The receiver operating characteristic (ROC) curve analysis was also performed to identify the cut-off of serum levels for pre-eclamptic patients in comparison to normal subjects. The p value < 0.05 was considered statistically significant.
There were no significant differences in maternal age, baby weight, and placental weight between the control group and in the pre-eclamptic group. At ≤ 34 weeks, the primigravidae women were found to be 52% and 56% in control group and pre-eclamptic group, respectively. However, at > 34 weeks, the primigravidae women were found to be 48% and 60% in the control group and in the pre-eclamptic group respectively. The difference in mean systolic blood pressure and diastolic blood pressure was significant in the study group than in the control group (Table 1).
The mean serum concentration of sVEGFR-2 in the control group was significantly higher (p = 0.02) at > 34 weeks (8693.8 ± 2829.7 pg/mL) as compared to ≤ 34 weeks (7645.8 ± 1938.0 pg/mL) while the sVEGFR-2 concentrations in pre-eclampsia were found to be down-regulated at > 34 weeks (Mean ± SD: 6266.6 ± 1824.2 pg/mL) as compared to ≤ 34 weeks (mean ± SD: 6541.6 ± 3285.8 pg/mL). Nevertheless, these levels were found to be substantially lower and significant (p = 0.01, p = 0.001) in pre-eclamptic sub-groups (≤ 34 and > 34 weeks) as compared to their respective control groups (Table 2, Fig. 1). Therefore, there was an inverse association between the serum concentrations of sVEGFR-2 in control and pre-eclampsia group as the gestation advances (Table 2). There was no significant difference in the mean serum concentration of sVEGFR-2 between the non-pregnant women (mean ± SD: 8497.6 ± 2968.8 pg/mL) and the women with normal pregnancy (p = 0.85, Table 2).
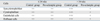
According to the ROC curve analysis (Fig. 2), the serum sVEGFR-2 level in pre-eclampsia in early onset (≤ 34 weeks) had the sensitivity and specificity of 60% and area under curve (AUC = 0.69). However, we observed the sensitivity and specificity of 76% and AUC = 0.79 in the late onset of disease (> 34 weeks). Serum sVEGFR-2 had the highest positive likelihood ratio (LR - 1.5) women with pre-eclampsia at ≤ 34 weeks and at > 34 weeks highest positive LR is 3.1 (Table 3).
At ≤ 34 weeks, in the control group as well as in the pre-eclampsia group, moderate membranous VEGFR-2 immunoreactivity was observed in the cells (sycytiotrophoblast, cytotrophoblast, endothelial and Hofbauer) of tertiary villi of placenta as shown in Figs. 3C, D.
At > 34 weeks, in control group, as the pregnancy progressed, the intensity of VEGFR-2 immunoreactivity was found to increase as compared to ≤ 34 weeks control placentae in all cells - sycytiotrophoblast, cytotrophoblast, endothelial and Hofbauer cells (p = 0.0001; Fig. 3E). However, membranous VEGFR-2 expression in the pre-eclampsia group was found to be significantly down-regulated than those of ≤ 34 weeks pre-eclamptic placenta (p = 0.0001) in all the cells. Also, significantly reduced VEGFR-2 immunoreactivity was found in these cells of the pre-eclamptic group as compared to the gestationally matched control patients (p = 0.0001, Table 4, Fig. 3F). Down-regulation of membranous VEGFR-2 immunoreactivity in pre-eclampsia patients at ≤ 34 weeks and > 34 weeks has been depicted in the bar diagram (Fig. 4).
VEGFR-2 is the major mediator of mitogenic and angiogenic effects of VEGF. The natural soluble form of VEGFR-2 has recently been detected in both mouse and human plasma.13 In contrast to sVEGFR-1, little is known about sVEGFR-2. There are clinical studies on sVEGFR-2 as a surrogate biomarker for tumour progression or survival in melanoma,19 myelodysplastic,20 leukaemia21-23 and pre-eclampsia patients.24 However, no clear pattern has yet emerged to indicate the utility of monitoring circulating sVEGFR-2 in relation to tumour growth, pre-eclampsia progression and the underlying mechanisms governing the observed changes.
Ebos et al.13 detected the soluble form of VEGFR-2 in conditioned media (CM) obtained from human endothelial cells, suggesting that endothelial cells are one source of plasma sVEGFR-2. However, the possibility that this soluble form of VEGFR-2 may be the result of alternative alternate messenger RNA (mRNA) splicing/or proteolytic cleavage of the membrane-bound receptor/or by some other mechanisms was remains to be elucidated.13 Also, it is unclear what biological agents could stimulate sVEGFR-2 levels. Till now, only Wen et al.25 showed sVEGFR-2 has been shown as a result of mRNA splicing, demonstrating the alternative splicing of VEGFR-2 mRNA in rat retinal cells that resulted in truncated form of VEGFR-2 which encoded a functional form of receptor lacking of a portion of the intracellular domain. A splice variation for VEGFR-2 encoding for the VEGFR-2 ectodomain also has not yet been detected.
sVEGFR-2 is able to bind VEGF, however, in contrast to sVEGFR-1 receptor-ligand complex, is heparin-dependent.26 Maynard et al.27 suggested that the administration of adenovirus encoding murine sVEGFR-2 to non-pregnant rats induces hypertension and proteinuria, showing anti-angiogenic properties of sVEGFR-2. This biological effect, however, was not observed in pregnant rats, possibly due to high levels of unopposed PLGF (which does not bind to sVEGFR-2) secreted by the placenta in the pregnant state. Another study supporting the role of sVEGFR-2 as an anti-angiogenic factor was reported after a local injection of recombinant sVEGFR-2 which inhibited retinal neovascularisation.14
So far, there are less data available describing the role of sVEGFR-2 in pre-eclamptic pregnancy. Masuyama et al.17 noticed that there was no significant difference in the mean serum concentration of sVEGFR-2 between patients with pre-eclampsia and women with normal pregnancies. However, Chaiworapongsa et al.24 reported the association of pre-eclampsia with lower plasma concentrations of sVEGFR-2. The mean serum concentration of sVEGFR-2 in the umbilical vein was observed in the same range as in maternal blood and was reported to be lower in both patients with pre-eclampsia and those with SGA than in women with normal pregnancies.28 Also, it was observed that the concentration of sVEGFR-2 in plasma [ethylenediaminetetraacetic acid (EDTA), citrate, or heparin] was not significantly different from that in serum.13
To date, no study has described the time period of altered sVEGFR-2 concentrations at different intervals of third trimester of pre-eclamptic pregnancy. Thus, there is still not enough evidence to support the view that altered levels of this angiogenic factor in maternal plasma/serum of pre-eclamptic women are the consequence or the cause of a placental insufficiency. Therefore, in this cross-sectional study, we measured sVEGFR-2 concentration at the early (≤ 34 weeks) and late (> 34 weeks) onset of pre-eclampsia, and the result showed that the mean serum sVEGFR-2 concentration in women with normal pregnancies was similar to that of non-pregnant women which agrees with the study conducted by Masuyama et al.17 It was also noticed that the mean serum concentration of sVEGFR-2 in control group was significantly higher (p = 0.02) at > 34 weeks (term), compared to ≤ 34 weeks (preterm). However, in the early (≤ 34 weeks) and late onset (> 34 weeks) pre-eclampsia group, the sVEGFR-2 concentrations were found to be down-regulated at > 34 weeks, compared to ≤ 34 weeks, but the value was not significant (p = 0.34). Our findings are partially consistent with the study conducted by Chaiworapongsa et al.24 which showed that patients with early (≤ 34 weeks) and late onset (> 34 weeks) pre-eclamptic group had a much lower median serum sVEGFR-2 concentration as compared to their respective controls. However, this finding was unexpected because pre-eclampsia itself is considered to be an anti-angiogenic state.27
Furthermore, our findings suggest the serum levels of this anti-angiogenic factor for the diagnostic utility of sVEGFR-2 as a sensitive and specific biomarker for pre-eclampsia in the late onset of disease. The positive LR of this marker can increase the probability of having pre-eclampsia required to alter clinical decision making. The AUC comparison showed that serum sVEGFR-2 is a significantly better test to differentiate the late onset (> 34 weeks) with an early onset (≤ 34 weeks) of pre-eclampsia.
Soluble VEGFR-1 has a higher affinity for VEGF than VEGFR-2 and reduces the availability of free VEGF to bind VEGFR-2.29 This agrees to the observation that plasma VEGF concentration in pre-eclampsia is lower than normal pregnancy. Robinson et al.30 reported that the reduced concentrations of free VEGF could interfere with endothelial cell function and survival. Although it was previously shown that sVEGFR-2 can bind to VEGF,13 it remains unknown whether sVEGFR-2, like other soluble receptors such as sVEGFR-1,31 can bind and sequester VEGF in vivo, thereby influencing binding and activation of VEGFRs. Therefore, it was hypothesised that the lower concentration of sVEGFR-2 in patients with pre-eclampsia may result from the low availability of free VEGF to stimulate VEGFR-2 in endothelial cells.27,32 Thus, serum sVEGFR-2 concentration could be a surrogate marker of endothelial cell function in the maternal circulation, since VEGF signalling through VEGFR-2 is essential for endothelial cell function and survival.33
The lower sVEGFR-2 plasma concentrations in patients with pre-eclampsia, might reflect low regenerative capacity of endothelial cells.34 The circulating endothelial progenitor cells are phenotypically defined by flow cytometry as cells that express CD34 and VEGFR-2,35 are capable of mobilizing to the sites of tissue or endothelial cell injuries for repair purposes, and correlate inversely with the risk of future death in patients with coronary artery disease.36 Alternatively, plasma concentrations of sVEGFR-2 in patients with pre-eclampsia might reflect low endothelial cell regenerative capacity. It may be due to lower number of circulating endothelial progenitor cells and lower plasma concentrations of sVEGFR-2 in patients with pre-eclampsia than women with normal pregnancies.34,37 The numbers of these cells have been proposed to reflect regenerative capacity of endothelial cells.36 Consistent with this hypothesis, several lines of evidence suggest that patient with pre-eclampsia, especially in the early onset group, or women who delivered a low birth weight neonate have increased risk of developing cardiovascular disease.38,39 Hence, this study showed that these pre-eclamptic women were more susceptible to low regenerative capacity for endothelial cells, and thus, might be at risk for cardiovascular disease.
Membranous VEGFR-2 is the major positive signal transducer for both physiological and pathological angiogenesis. VEGFR-2 knocks-out mice die at E8.0 - 8.5 due to lack of vasculogenesis which indicates that the VEGFR-2 signalling is essential for the differentiation of VEGFR-2 positive endothelial precursor cells into vascular endothelial cells as well as for their proliferation.40 Takahashi et al.41 noticed that VEGFR-1 by itself does not generate a strong signal for vascular permeability activity; it cooperates with VEGFR-2 to significantly enhance the permeability and is involved in several diseases. Hence, VEGFR-2 plays a more important functional role in mediating signalling events involved in endothelial cell mitogenesis, migration, survival and vascular permeability.45 The production and localization of VEGF and its receptor in trophoblast, endothelial cells, and Hofbauer cells in placenta villi have been already investigated.42-44 A low level of expression for the membranous form of VEGFR-2 was also observed in neurons, osteoblasts, pancreatic duct cells, retinal progenitor cells, and megakaryocytes.40 VEGFR-2 mRNA and protein at term are localized almost exclusively to vascular endothelial cells of the placenta in contrast to VEGFR-1, which is expressed mainly on trophoblasts.43,46 Although the membranous isoform of VEGFR-2 was found to be localized mainly on endothelial cells, a fraction of hematopoietic cells, also known as circulating endothelial progenitor cells, also expressed VEGFR-2.40,47 There is an evidence to indicate that VEGFR-2 is expressed on cytotrophoblast stem cells and cells in the proximal columns of chorionic villi during the first and second trimesters of pregnancy48 showing its fundamental role in cytotrophoblast differentiation and survival during placentation. Several authors observed no significant difference in the expression of VEGFR-2 mRNA49 and protein48 in the placenta of patients with pre-eclampsia and that of women with normal pregnancies. However, a study using Western blot analysis of protein extracted from placentas showed that a lower expression of sVEGFR-2 was associated with pre-eclampsia patients as compared to normal patients.50 Alhough it is unclear what biological agents could stimulate VEGFR-2 expression, the expression of the membranous isoform of VEGFR-2 is stimulated by VEGF and TNF-alpha.51,52 Conflicting results have been reported regarding the effect of hypoxia on VEGFR-2 expression: either no change in umbilical vein33 decreased in the skin53 or increased in the brain54 depending on the cell type. The present study depicted the expression of VEGFR-2 in control and pre-eclamptic placentae at ≤ 34 weeks and at > 34 weeks in syncytiotrophoblast, cytotrophoblast, and endothelial and Hofbauer cells. This complex pattern of VEGFR-2 immunoreactivity suggests that it may be involved not only in the regulation of placental angiogenesis but also in trophoblast invasion. At > 34 weeks, the VEGFR-2 immunoreactivity was significantly reduced (p = 0.0001) in villous trophoblasts, and endothelial cells and Hofbauer cells of placenta villi in the pre-eclamptic group as compared to the control group. However, at ≤ 34 weeks, there was no change found in immunoreactivity of the pre-eclamptic group as compared to the control one. Therefore, it is highly likely that the VEGF ligand receptor system, apart from its endothelial mitogenic effect, must have additional roles when expressed in non-endothelial cells. Moreover, abnormal trophoblast invasion and differentiation are associated with pre-eclampsia.47,50 Pre-eclampsia is also associated with endothelial dysfunction which is characterized by an increased endothelial cell-mediated vasoconstriction, increased vascular permeability and an increased endothelial-mediated platelet aggregation which may lead to maternal hypertension, and proteinuria.55 Since VEGFR-2 is also expressed in endothelial cells and in Hofbauer cells, the altered expression of VEGFR-2 in endothelial cells and Hofbauer cells in pre-eclamptic placentae may interfere with VEGF mediated actions on these cells. This may affect normal fusion of angiogenic cell cords and organization of vascular capillaries. It suggests that VEGFR-2 is a key factor associated with pre-eclamptic pregnancies and its varying expression may alter VEGF mediated function on trophoblast, endothelial cells and Hofbauer cells.
Our results may be explained by VEGF-mediated receptor down-regulation from the cell surface, as membranous VEGFR-2 is in direct contact with maternal blood in intervillous space, which in turn leads to reduced sVEGFR-2 levels in serum in an autocrine manner, thus implying that expression levels of VEGFR-2 and its soluble forms are linked together. These results suggest that the decrease of sVEGFR-2 and membranous VEGFR-2 is inversely proportional to the progression of pre-eclampsia during pregnancy, indicating a potential role of these proteins in the pathogenesis of this disorder. VEGF binding and activation of the VEGFR-2 may lead to down-regulation of the receptor from the cell surface56,57 which, in turn may lead to correlative decreases in sVEGFR-2 production. However, it remains unknown whether the sVEGFR-2 is a product of ectodomain cleavage from cell-surface VEGFR-2 or a product of alternative mRNA splice variation.
Our findings strongly suggest the clinical utility of sVEGFR-2 and membranous VEGFR-2 in pregnancies complicated by pre-eclampsia patients. This information of significant down-regulation of serum sVEGFR-2 levels and membranous VEGFR-2 expression in pre-eclampsia patients may be used as a strategy for mapping out the management plans to pre-eclamptic patients. Furthermore, this may lead to better insights into the diagnosis and treatment of pre-clampsia by angiogenic and anti-angiogenic therapy, and in turn may improve further understanding and utilization of sVEGFR-2 as a potential biomarker for monitoring pre-eclampsia progression.
Figures and Tables
 | Fig. 1sVEGFR-2 concentrations (pg/mL) in maternal serum of control and pre-eclamptic patients. The median serum concentration of sVEGFR-2 was significantly decreased in pre-eclmpsia patients. The horizontal lines indicate the mean values of the study groups. (A) In ≤ 34 weeks (p = 0.01). (B) In > 34 weeks (p = 0.001). sVEGFR-2, soluble vascular endothelial growth factor receptor-2 ; VEGFR-2, vascular endothelial growth factor receptor-2. |
 | Fig. 2Receiver Operating Characteristic (ROC) curve analysis of sVEGFR-2 in pre-eclampsia showing the ability of maternal serum sVEGFR-1 to differentiate pre-eclampsia from normal pregnancies. (A) At ≤ 34 weeks (AUC = 0.69), (B) At > 34 weeks (AUC = 0.76). AUC, area under curve. sVEGFR-2, soluble vascular endothelial growth factor receptor-2 . |
 | Fig. 3Immunohistochemical staining for VEGFR-2 in normal and pre-eclamptic placenta. (A) Negative control - VEGFR-2 control sections incubated with IgG non-immune serum (omitted primary antibody) showing syncytiotrophoblast (S) cytotrophoblast (C), Endothelial cells (E) Hofbauer cells (H) with no staining (Scale bar- 5 µm). (B) Positive control -hCG- Showing placental villi showing intense staining of syncytiotrophoblast (S), cytotrophoblast (C), Endothelial cells (E) and Hofbauer cells (H) (Scale bar- 5 µm). (C) 28 weeks (≤ 34 weeks) control placentae showing moderate VEGFR-2 expression in syncytiotrophoblast (S), cytotrophoblast (C), Endothelial (E), Hofbauer cells (H) (Scale bar - 5µm). (D) 28weeks (≤ 34 weeks) pre-eclamptic placentae showing moderate VEGFR-2 expression in syncytiotrophoblast (S), cytotrophoblast (C), Endothelial (E), Hofbauer cells (H) (Scale bar- 5 µm). (E) 37 weeks (> 34 weeks) control placentae showing intensed VEGFR-2expression in syncytiotrophoblast (S), Endothelial (E) and Hofbauer cells (H) (Scale bar- 5 µm). (F) 37 weeks (> 34 weeks) pre-eclamptic placentae showing mild VEGFR-2 expression in syncytiotrophoblast (S), Endothelial (E) and Hofbauer cells (H) (Scale bar- 5 µm). VEGFR-2, vascular endothelial growth factor receptor-2; IgG, immunoglobulin G; hCG, human Chorio-gonadotropin. |
 | Fig. 4Comparison of immunohistochemical H-scores for membranous VEGFR-2 in the cells of control and pre-eclamptic patients at ≤ 34 and > 34 weeks. Data are expressed as Mean values (At > 34 weeks, p = 0.0001, pre-eclampsia vs. control). |
Table 2
Serum Concentration of sVEGFR-2 in Control and Preeclampsia Cases
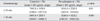
VEGFR-2, vascular endothelial growth factor redeptor-2; sVEGFR-2, soluble vascular endothelial growth factor receptor-2.
VEGFR-2 level of non-pregnant group (n = 20), 8497.6 ± 2968.8, p = 0.85 (mean ± SD).
Total sVEGFR-2 level of control group was 7617.74 ± 3223.6.
Total sVEGFR-2 level of Pre-eclamptic group was 6956.2 ± 1988.
p < 0.05 is considered to be significant.
ACKNOWLEDGEMENTS
This work was supported by a grant of Council of Scientific and Industrial Research (CSIR Project No.27-0133/04/EMR II), New Delhi, India. Ms. Richa Tripathi is a recipient of the Senior Research Fellowship of Indian Council of Medical Research (ICMR), New Delhi, India.
References
1. Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in pregnancy. Am J Obstet Gynecol. 2000. 183:S1–S22.
2. Talbert DG. Uterine flow velocity waveform shape as an indicator of maternal and placental development failure mechanisms: a model-based synthesizing approach. Ultrasound Obstet Gynecol. 1995. 6:261–271.

3. Guzin K, Tomruk S, Tuncay YA, Naki M, Sezginsoy S, Zemheri E, et al. The relation of increased uterine artery blood flow resistance and impaired trophoblast invasion in pre-eclamptic pregnancies. Arch Gynecol Obstet. 2005. 272:283–288.
4. Ferrara N, Gerber HP, LeCouter J. The biology of VEGF and its receptors. Nat Med. 2003. 9:669–676.

5. Kondo K, Hiratsuka S, Subbalakshmi E, Matsushime H, Shibuya M. Genomic organization of the flt-1 gene encoding for vascular endothelial growth factor (VEGF) receptor-1 suggests an intimate evolutionary relationship between the 7-Ig and the 5-Ig tyrosine kinase receptors. Gene. 1998. 208:297–305.
6. Hornig C, Behn T, Bartsch W, Yayon A, Weich HA. Detection and quantification of complexed and free soluble human vascular endothelial growth factor receptor-1 (sVEGFR-1) by ELISA. J Immunol Methods. 1999. 226:169–177.

7. Holash J, Davis S, Papadopoulos N, croll SD, HO L, Russell M, et al. VEGF-Trap: a VEGF blocker with potent antitumor effects. Proc Natl Acad Sci U S A. 2002. 99:11393–11398.

8. Aiello LP, Pierce EA, Foley ED, Takagi H, Chen H, Riddle L, et al. Suppression of retinal neovascularization in vivo by inhibition of vascular endothelial growth factor using soluble VEGF-receptor chimeric proteins. Proc Natl Acad Sci U S A. 1995. 92:10457–10461.

9. Rodesch F, Simon P, Donner C, Jauniaux E. Oxygen measurements in endometrial and trophoblastic tissues during early pregnancy. Obstet Gynecol. 1992. 80:283–285.
10. Yang JC, Haworth L, Sherry RM, Hwu P, Schwartzentruber DJ, Topalian SL, et al. A randomized trial of bevacizumab, an antivascular endothelial growth factor antibody, for metastatic renal cancer. N Engl J Med. 2003. 349:427–434.

11. Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, et al. Areversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996. 334:494–500.
12. Tripathi R, Rath G, Jain A, Salhan S. Soluble and membranous vascular endothelial growth factor receptor-1 in pregnancies complicated by pre-eclampsia. Ann Anat. 2008. 190:477–489.

13. Ebos JM, Bocci G, Man S, Thorpe PE, Hicklin DJ, Zhou D, et al. A naturally occurring soluble form of vascular endothelial growth factor receptor 2 detected in mouse and human plasma. Mol Cancer Res. 2004. 2:315–326.
14. Agostini H, Boden K, Unsöld A, Martin G, Hansen L, Fiedler U, et al. A single local injection of recombinant VEGF receptor 2 but not of Tie2 inhibits retinal neovascularization in the mouse. Curr Eye Res. 2005. 30:249–257.

15. Robak E, Sysa-Jedrzejewska A, Robak T. Vascular endothelial growth factor and its soluble receptors VEGFR-1 and VEGFR-2 in the serum of patients with systemic lupus erythematosus. Mediators Inflamm. 2003. 12:293–298.
16. Wierzbowska A, Robak T, Wrzesien-Kus A, Krawczynska A, Lech-Maranda E, Urbanska-Rys H. Circulating VEGF and its soluble receptors sVEGFR-1 and sVEGFR-2 in patients with acute leukemia. Eur Cytokine Netw. 2003. 14:149–153.
17. Masuyama H, Suwaki N, Nakatsukasa H, Masumoto A, Tateishi Y, Hiramatrsu Y. Circulating angiogenic factors in preeclampsia, gestational proteinuria, and preeclampsia superimposed on chronic glomerulonephritis. Am J Obstet Gynecol. 2006. 194:551–556.

18. Demir R, Kayisli UA, Seval Y, Celik-Ozenci C, Korgun ET, Demir-Weusten AY, et al. Sequential expression of VEGF and its receptors in human placental villi during very early pregnancy: differences between placental vasculogenesis and angiogenesis. Placenta. 2004. 25:560–572.

19. Tas F, Duranyildiz D, Oguz H, Camlica H, Yasasever V, Topuz E. Circulating serum levels of angiogenic factors and vascular endothelial growth factor receptors 1 and 2 in melanoma patients. Melanoma Res. 2006. 16:405–411.

20. Cortelezzi A, Fracchiolla NS, Mazzeo LM, Silvestris I, Pomati M, Somalvico F, et al. Endothelial precursors and mature endothelial cells are increased in the peripheral blood of myelodysplastic syndromes. Leuk Lymphoma. 2005. 46:1345–1351.

21. Aref S, El Sherbiny M, Goda T, Fouda M, Al Askalany H, Abdalla D. Soluble VEGF/sFLt1 ratio is an independent predictor of AML patient out come. Hematology. 2005. 10:131–134.

22. Faderl S, Do KA, Johnson MM, Keating M, O'brien S, Jillani I, et al. Angiogenic factors may have a different prognostic role in adult acute lymphoblastic leukemia. Blood. 2005. 106:4303–4307.

23. Hu Q, Dey AL, Yang Y, Shen Y, Jilani IB, Estey EH, et al. Soluble vascular endothelial growth factor receptor 1, and not receptor 2, is an independent prognostic factor in acute myeloid leukemia and myelodysplastic syndromes. Cancer. 2004. 100:1884–1891.

24. Chaiworapongsa T, Romero R, Gotsch F, Espinoza J, Nien JK, Goncalves L, et al. Low maternal concentrations of soluble vascular endothelial growth factor receptor-2 in preeclampsia and small for gestational age. J Matern Fetal Neonatal Med. 2008. 21:41–52.

25. Wen Y, Edelman JL, Kang T, Zeng N, Sachs G. Two functional forms of vascular endothelial growth factor receptor-2/Flk-1 mRNA are expressed in normal rat retina. J Biol Chem. 1998. 273:2090–2097.

26. Roeckl W, Hecht D, Sztajer H, Waltenberger J, Yayon A, Weich HA. Differential binding characteristics and cellular inhibition by soluble VEGF receptors 1 and 2. Exp Cell Res. 1998. 24:161–170.

27. Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. Excess placental soluble fms-like tyrosine kinase-1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest. 2003. 111:649–658.

28. Wallner W, Sengenberger R, Strick R, Strissel PL, Meurer B, Beckmann MW, et al. Angiogenic growth factors in maternal and fetal serum in pregnancies complicated by intrauterine growth restriction. Clin Sci (Lond). 2007. 112:51–57.

29. Nagamatsu T, Fujii T, Kusumi M, Zou L, Yamashita T, Osuga Y, et al. Cytotrophoblasts up-regulate soluble fms-like tyrosine kinase-1 expression under reduced oxygen: an implication for the placental vascular development and the pathophysiology of preeclampsia. Endocrinology. 2004. 145:4838–4845.

30. Robinson CJ, Stringer SE. The splice variants of vascular endothelial growth factor (VEGF) and their receptors. J Cell Sci. 2001. 114(Pt 5):853–865.

31. Kendall RL, Thomas KA. Inhibition of vascular endothelial cell growth factor activity by an endogenously encoded soluble receptor. Proc Natl Acad Sci U S A. 1993. 90:10705–10709.

32. Reuvekamp A, Velsing-Aarts FV, Poulina IE, Capello JJ, Duits AJ. Selective deficit of angiogenic growth factors characterises pregnancies complicated by pre-eclampsia. Br J Obstet Gynaecol. 1999. 106:1019–1022.

33. Gerber HP, Condorelli F, Park J, Ferrara N. Differential transcriptional regulation of the two vascular endothelial growth factor receptor genes. Flt-1, but not Flk-1/KDR, is up-regulated by hypoxia. J Biol Chem. 1997. 272:23659–23667.

34. Kim SY, Park SY, Kim JW, Kim YM, Yang JH, Kim MY, et al. Circulating endothelial progenitor cells, plasma VEGF, VEGFR-1 andVEGFR-2 levels in pre-eclampsia. Am J Obstet Gynecol. 2005. 193:S74.
35. Khan SS, Solomon MA, McCoy JP Jr. Detection of circulating endothelial cells and endothelial progenitor cells by flow cytometry. Cytometry B Clin Cytom. 2005. 64:1–8.

36. Werner N, Kosiol S, Schiegl T, Ahlers P, Walenta K, Link A, et al. Circulating endothelial progenitor cells and cardiovascular outcomes. N Engl J Med. 2005. 353:999–1007.

37. Sugawara J, Mitsui-Saito M, Hayashi C, Hoshiai T, Senoo M, Chisaka H, et al. Decrease and senescence of endothelial progenitor cells in patients with preeclampsia. J Clin Endocrinol Metab. 2005. 90:5329–5332.

38. Ray JG, Vermeulen MJ, Schull MJ, Redelmeier DA. Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet. 2005. 366:1797–1803.

39. Smith GD, Sterne J, Tynelius P, Lawlor DA, Rasmussen F. Birth weight of offspring and subsequent cardiovascular mortality of the parents. Epidemiology. 2005. 16:563–569.

40. Shibuya M. Differential roles of vascular endothelial growth factor receptor-1 and receptor-2 in angiogenesis. J Biochem Mol Biol. 2006. 39:469–478.

41. Takahashi H, Hattori S, Iwamatsu A, Takizawa H, Shibuya M. A novel snake venom vascular endothelial growth factor (VEGF) predominantly induces vascular permeability through preferential signaling via VEGF receptor-1. J Biol Chem. 2004. 279:46304–46314.

42. Cooper JC, Sharkey AM, McLaren J, Charnock-Jones DS, Smith SK. Localization of vascular endothelial growth factor and its receptor, flt, in human placenta and deciduas by immunohistochemistry. J Reprod Fertil. 1995. 105:205–213.

43. Clark DE, Smith SK, Sharkey AM, Charnock-Jones DS. Localization of VEGF and expression of its receptors flt and KDR in human placenta throughout pregnancy. Hum Reprod. 1996. 11:1090–1098.

44. Vuckovic M, Ponting J, Terman BI, Niketie V, Seif MW, Kumar S. Expression of the vascular endothelial growth factor receptor, KDR, in human placenta. J Anat. 1996. 188(Pt 2):361–366.
45. Shibuya M. Structure and dual function of vascular endothelial growth factor receptor-1 (Flt-1). Int J Biochem Cell Biol. 2001. 33:409–420.

46. Peichev M, Naiyer AJ, Pereira D, Zhu Z, Lane WJ, Williams M, et al. Expression of VEGFR-2 and AC133 by circulating human CD34(x) cells identifies a population of functional endothelial precursors. Blood. 2000. 95:952–958.

47. Zhou Y, McMaster M, Woo K, Janatpour M, Perry J, Karpanen T, et al. Vascular endothelial growth factor ligands and receptors that regulate human cytotrophoblast survival are dysregulated in severe preeclampsia and hemolysis, elevated liver enzymes, and low platelets syndrome. Am J Pathol. 2002. 160:1405–1423.

48. Helske S, Vuorela P, Carpén O, Hornig C, Weich H, Halmesmäki E. Expression of vascular endothelial growth factor receptors 1, 2 and 3 in placentas from normal and complicated pregnancies. Mol Hum Reprod. 2001. 7:205–210.

49. Tsatsaris V, Goffin F, Munaut C, Brichant JF, Pignon MR, Noel A, et al. Overexpression of the soluble vascular endothelial growth factor receptor in preeclamptic patients: pathophysiological consequences. J Clin Endocrinol Metab. 2003. 88:5555–5563.

50. Rajakumar A, Brandon HM, Daftary A, Ness R, Conrad KP. Evidence for the functional activity of hypoxiainducible transcription factors overexpressed in preeclamptic placentae. Placenta. 2004. 25:763–769.

51. Giraudo E, Primo L, Audero E, Gerber HP, Koolwijk P, Soker S, et al. Tumor necrosis factor-alpha regulates expression of vascular endothelial growth factor receptor-2 and of its coreceptor neuropilin-1 in human vascular endothelial cells. J Biol Chem. 1998. 273:22128–22135.

52. Shen BQ, Lee DY, Gerber HP, Keyt BA, Ferrara N, Zioncheck TF. Homologous up-regulation of KDR/Flk-1 receptor expression by vascular endothelial growth factor in vitro. J Biol Chem. 1998. 273:29979–29985.

53. Detmar M, Brown LF, Berse B, Jackman RW, Elicker BM, Dvorak HF, et al. Hypoxia regulates the expression of vascular permeability factor/vascular endothelial growth factor (VPF/VEGF) and its receptors in human skin. J Invest Dermatol. 1997. 108:263–268.

54. Elvert G, Kappel A, Heidenreich R, Englmeier U, Lanz S, Acker T, et al. Cooperative interaction of hypoxia-inducible factor-2alpha (HIF-2alpha) and Ets-1 in the transcriptional activation of vascular endothelial growth factor receptor-2 (Flk-1). J Biol Chem. 2003. 278:7520–7530.

55. Roberts JM, Lain KY. Recent insights into the pathogenesis of pre-eclampsia. Placenta. 2002. 23:359–372.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download