Abstract
Purpose
This study was aimed to describe a vancomycin-resistant enterococci (VRE) outbreak across three intensive care units (ICUs) of a Korean hospital from September 2006 to January 2007 and the subsequent control strategies.
Materials and Methods
We simultaneously implemented multifaceted interventions to control the outbreak, including establishing a VRE cohort ward, active rectal surveillance cultures, daily extensive cleaning of environmental surfaces and environmental cultures, antibiotic restriction, and education of hospital staff. We measured weekly VRE prevalence and rectal acquisition rates and characterized the VRE isolates by polymerase chain reaction (PCR) of the vanA gene and Sma1-pulsed-field gel electrophoresis (PFGE).
Results
During the outbreak, a total of 50 patients infected with VRE were identified by clinical and surveillance cultures, and 46 had vancomycin-resistant Enterococcus faecium (VREF). PFGE analysis of VREF isolates from initial two months disclosed 6 types and clusters of two major types. The outbreak was terminated 5 months after implementation of the interventions: The weekly prevalence rate decreased from 9.1/100 patients-day in September 2006 to 0.6/100 by the end of January 2007, and the rectal acquisition rates also dropped from 6.9/100 to 0/100 patients-day.
Vancomycin-resistant enterococci (VRE) are recognized as significant nosocomial pathogens that are predictive of mortality and a longer duration of hospitalization.1 Nationwide surveillance data in Korea showed increasing resistance of Enterococcus faecium to vancomycin among clinical isolates, ranging from 2.9% in 1997 to 16% in 2006.2 Outbreaks and endemicity of VRE have also been reported in Korean hospitals.3,4 The increasing prevalence of VRE poses important problems because of limited effective antimicrobial therapy for VRE infection and the increasing risk for transfer of vancomycin-resistance genes to methicillin-resistant Staphylococcus aureus (MRSA) in Korean hospitals where MRSA have been endemic.
Hospital Infection Control Practices Advisory Committee (HICPAC) recommendations and the Society for Healthcare Epidemiology of America (SHEA) guidelines have been developed for preventing transmission and endemicity of VRE and have widely been circulated.5,6 These extensive guidelines have proven to be effective for control of nosocomial spread or outbreaks of VRE, but might be too expensive to implement, especially in a setting where resources are limited. In Korea, there are limited experiences regarding the current guidelines for intervention strategies for control of VRE outbreak.
In September 2006, we identified a VRE outbreak across three intensive care units (ICUs) of our hospital. This prompted us to implement intensified control measures for the following 5 months. In this study, we describe the molecular epidemiology of the outbreak, as well as the intervention strategies that resulted in successful control of the outbreak.
Our study was conducted in the 52 ICU beds of an 850-bed tertiary care hospital: 20 beds for medical ICU (MICU), 20 for surgical ICU (SICU), and 12 for combined ICU (CICU). All three ICUs are located on the same floor. Standard infection control measures, including alcohol-based hand hygiene practices and contact isolation for all patients colonized or infected with VRE, were in place in the ICUs before the VRE outbreak.
A patient in CICU was identified as an index case; this patient was admitted on June 20, 2006 and received hemodialysis due to acute renal failure. She was complicated with bloody diarrhea and E. faecium sepsis. After her death on July 18, 2006, surveillance cultures detected VRE in 4 samples of 12 patients' rectal swabs, 2 of 25 environmental surfaces and 2 of 25 health care workers' (HCWs) hands; the immediate response was contact isolation of the colonized patients, extensive cleaning of the environmental surfaces, and strengthening of hand hygiene. However, follow-up surveillance cultures on September 4, 2006 detected VRE in 4 samples of 9 patients' rectal swabs and one of 29 environmental surfaces in the CICU. In addition, we found three patients with VRE isolation from clinical culture in MICU and SICU: one had been transferred from CICU to MICU on July 22, 2006 and the other two patients had been cared for by doctors who had cared for VRE patients in CICU. The hospital infection control unit recognized these findings as dissemination of VRE across three ICUs, and urgently established a VRE cohort in the CICU and simultaneously implemented intensified control measures.
The task force team for VRE control was composed of two infectious disease specialists, three head nurses from the three ICUs, and an infection control practitioner. The team weekly monitored the VRE acquisition rates and made decisions on control measures.
Starting on September 10, 2006, two cohorts of patients were established on each side of the CICU for a month. All VRE-infected or colonized patients were placed in the VRE zone where strict contact precautions with gowns and gloves were maintained. Patients who had VRE-negative rectal swabs on admission were placed in the designated clean zone. Four beds between the two zones were closed. Each cohort had a dedicated nursing staff and patient-care equipment, and movement of nursing staff between the two zones was strictly prohibited. Portable radiologic examinations were conducted under strict barrier precautions. Transfer of patients to the VRE zone had to be approved by the VRE control team. VRE cases in MICU and SICU were placed in isolated rooms under strict contact precautions.
To detect and monitor patients with new VRE acquisition, we conducted weekly rectal surveillance cultures for all patients who stayed in the ICUs for more than 24 hours throughout the study period. Acquisition rate and prevalence were calculated every week by surveillance and clinical cultures to monitor the trends of VRE outbreak in all three ICUs.
Environmental decontamination was conducted with extensive cleaning practices for environmental surfaces in all three ICUs. Environmental surfaces were rigorously cleaned three times a day throughout the outbreak. The decontamination included cleansing with 5% sodium hypochlorite. Environmental surveillance cultures for VRE were performed to monitor environmental contamination. Swab samples were taken from the vicinity of patients (i.e., the locker, over-bed table, mattress, pillow, the oxygen supply and suction apparatuses, etc.) and general areas (i.e., equipment, nurses' station, and computer keyboards and terminals).
Our hospital has a computerized antibiotic prescription system with a restriction policy for the use of 15 agents, including vancomycin and ceftriaxone, requiring approval from infectious diseases specialists. During the period of outbreak control, doctors were encouraged to limit empirical use of vancomycin and all third-generation cephalosporins in ICU patients. Consumption of third-generation cephalosporins and vancomycin was calculated to monitor monthly quantities and expressed as antimicrobial use density (AUD; defined daily doses per 1,000 patients-day).7
We informed all health care workers (HCWs) of the VRE outbreak through the hospital's intranet. Heightened infection control measures, especially hand hygiene, and enhanced auditing of these measures were enforced. We noted whether each person washed his hands before and after visits to the ICUs. The conducted rate of hand washing was about 95% after monitoring began.
To isolate VRE, clinical specimens were inoculated on 5% sheep blood agar and incubated for 48 h at 35℃ in a 5% CO2 atmosphere. Rectal and environmental swabs were inoculated on Enterococcosel culture plates (Difco Laboratories, Detroit, MI, USA) containing 15 µg/mL vancomycin and 8 µg/mL clindamycin at 35℃ in ambient air for 48 h. Presumptive Enterococcus species were identified by conventional biochemical methods, including chromogenic agar for VRE screening (bioMerieux, Marcy I'Etoile, France) and the Vitek 2 GP card (bioMerieux).
A multiplex polymerase chain reaction (PCR) was performed to detect vanA genes, as described previously.8 Vancomycin and teicoplanin multifaceted control interventions were determined by E-test (AB Biodisk, Solna, Sweden) using Mueller-Hinton agar.
Genomic DNA, prepared from patients' and environmental isolates, were digested with the restriction endonuclease SmaI and analyzed by pulsed-field gel electrophoresis (PFGE) on the CHEF-DRII system (Bio-Rad, Hercules, CA, USA) as previously described.9 The banding patterns were interpreted according to the published criteria.10
A total of 50 VRE-positive patients were identified through surveillance (n = 39) and clinical cultures (n = 11) in three ICUs during the study period from September 4, 2006 to January 29, 2007. With implementation of the intensified intervention, the weekly prevalence of VRE decreased gradually from 9.1/100 patients-day in early September to 0.6/100 patients-day by the end of January, 2007 (Fig. 1).
We performed a total of 756 rectal surveillance cultures and identified 43 (5.7%) VRE carriers. Among the VRE isolates, E. faecium was the most common isolate (90.7%, 39/43). E. faecalis was isolated from 2 patients, and E. avium and E. gallinarium were detected from one patient each. Four patients simultaneously showed VRE isolation from clinical cultures. The weekly rectal acquisition rate of VRE was 6.9/100 patients-day in early September and dropped to 0/100 patients-day by the end of January 2007 when we declared the termination of the VRE outbreak in the ICUs.
Environmental surveillance cultures for VRE were performed three times (July, September and October 2006) before and after implementation of the extensive cleaning practices for environmental surfaces in the ICUs. A total of 113 environmental samples were examined. Out of a total of 54 environmental surveillance cultures from the CICU in July 2006, three (5.6%) samples were VRE-positive. After environmental cleaning was introduced, subsequent cultures performed in September and October 2006 showed no VRE isolation except one VRE-positive sample from a computer keyboard in the MICU.
We calculated the monthly consumption of third-generation cephalosporin and vancomycin, and compared them to the respective amounts in the pre-intervention period (from April 2006 to August 2006) and the intervention period (from September 2006 to January 2007). There was a decreasing trend in the use of third-generation cephalosporins (AUD, 292.7 ± 39.9 vs. 256.2 ± 27.6, p = 0.132) and vancomycin (AUD, 360.6 ± 25.9 vs. 310.8 ± 48.6, p = 0.078) between the two means, however, the difference was not statistically significant (Fig. 2).
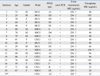
Twenty-one VRE isolates collected from surveillance cultures during the two early months of the outbreak were available for molecular analysis, including vancomycin-resistant Enterococcus faecium (VREF) (n = 19) and vancomycin-resistant E. faecalis (n = 2). All 21 isolates carried the vanA gene according to the multiplex PCR assay and E-test. PFGE analysis of 19 VREF isolates showed polyclonality of 6 types (A to F), with two predominant types, A (31.6%) and D (36.8%) (Table 1). Distribution of the PFGE types in the three ICUs over the initial six weeks is shown in Fig. 3. The A and D clonal types were associated with two small clusters with inter-ICU spread: The cluster of clonal type A with an environmental isolate (A2) occurred initially in CICU and then spread to SICU and MICU. Clonal type D clustered in SICU in mid-October 2006 and then spread to MICU.
Herein, we described a VRE outbreak across all three ICUs of a university hospital and the successful control of VRE following implementation of multifaceted interventions. Although a number of administrative obstacles regarding reimbursement and staffing issues remained to be solved, establishment of a cohort ward, active rectal surveillance for VRE, contact isolation, and extensive environmental cleaning and cultures were carried out simultaneously to prevent VRE endemicity and the rising threat of vancomycin-resistant Staphylococcus aureus in our ICUs.
The initial transmission of VRE was identified in patients and environments in an ICU that housed the index case which was complicated with VREF sepsis and profuse diarrhea. Hand hygiene practices were reinforced, and contaminated environmental surfaces were cleaned, however, contact isolation of the VRE carriers was not adequate due to the limited numbers of single rooms available. Transmission of VRE to two adjacent ICUs soon followed and might have been facilitated by frequent movement of patients between ICUs and HCWs' poor compliance to contact precautions.
A total of 50 patients colonized or infected with VRE were identified in three ICUs during the control of the outbreak from September 2006 to January 2007. Molecular analysis of VRE isolates from rectal surveillance cultures during the initial two months of the outbreak revealed that E. faecium carrying the vanA gene was likely the epidemic strain. Polyclonal distribution of the VREF genotypes over three ICUs indicated inter-ICU transmission of these clones, as well as potential horizontal transfer of the mobile vanA gene element.11,12 In addition, two clusters of A and D clonal types suggested that clonal spread might have occurred among patients via the contaminated hands of HCWs involved in the care of infected or colonized patients.13-15 Isolation of the same epidemic type from environmental cultures also indicated the role of environmental contamination in this outbreak.
In our study, we applied an aggressive strategy to control the VRE outbreak immediately after the outbreak was recognized in the units. It consisted of cohorting of VRE cases and staff in a dedicated ward, active surveillance cultures for monitoring and early detection of VRE transmission in the units, and daily environmental decontamination, according to previous studies and SHEA guidelines.6,16-21
In particular, the VRE cohort ward in one of the three ICUs was quickly established from the beginning of the intervention, because there were limited numbers of single rooms available for isolation of several patients with VRE who still were being treated under critical care. Cohorting can be very effective for physical segregation of VRE patients, potential staff carriers and environmental reservoirs. These are known risk factors associated with VRE outbreak. An additional advantage of cohorting is intensified compliance with isolation guidelines.20,22 Nonetheless, we maintained the cohorting for only a month due to administrative obstacles. The remaining VRE patients were then placed in single rooms in the ICUs or general wards.
Although active rectal surveillance for VRE acquisition and isolation practices have not still been generalized in ICUs of Korean hospitals, we confirmed that this practice allowed earlier detection of colonized patients, prompted proper conduct of contact precautions, and decreased person-to-person transmission.21,23 Moreover, weekly monitoring and reporting of the rectal VRE acquisition rates to HCWs were useful tool for evaluating the effect of ongoing control measures and provided good feedback.
As reported by others,14,24 our findings on environmental contamination with VRE which is identical to the epidemic strain suggest that the environment may play a major role as a reservoir in this outbreak, probably through transmission from the unwashed hands of HCWs. Therefore, extensive cleaning of the environmental surfaces was an important part of our intensified interventions and might have affected the outbreak control.
In our study, the antibiotic control policy to limit empirical use of vancomycin and third-generation cephalosporins did not significantly reduce the consumption of the antibiotics, probably due to the high prevalence of serious conditions in the target population of our ICUs, especially where methicillin-resistant S. aureus (MRSA) had been highly endemic. Although recommended as one of the strategies to control VRE outbreak,5,25-27 other studies have shown that controlled vancomycin use did not reduce VRE transmission.28,29 Furthermore, VRE eradication was achieved with use of other control measures in the absence of other antibiotic control except for vancomycin restriction, as well as with a continued high prevalence of antibiotic use in the ICU.13,30
Our study has several limitations. We found it difficult to evaluate the impact of each individual intervention on the control of the outbreak. However, we believe that simultaneous implementation of these measures played a role in more rapid and effective control of the outbreak, as we identified multiple mechanisms of VRE transmission that were probably involved in the occurrence of this outbreak. The cost-effectiveness of the multifaceted control measures was not determined in this study. We applied contact isolation to all VRE carriers detected during the outbreak, including two carriers with E. avium and E. gallinarium. We did not confirm the presence of the vanA gene in E. avium and E. gallinarium isolates, however, the potential of the vanA gene transfer between them and E. faecium needs to be addressed.
In conclusion, our study characterized the VRE outbreak across three ICUs at the molecular level and disclosed potential factors associated with VRE transmission. Our study further suggests that an aggressive multifaceted control strategy might be a rapid and effective approach for controlling VRE outbreak in non-endemic hospitals.
Figures and Tables
Fig. 1
Weekly prevalence and acquisition rates of vancomycin-resistant enterococci cases in surveillance cultures during the 5-month outbreak control period (cases per 100 patients-day).

Fig. 2
Monthly consumption of third-generation cephalosporins and vancomycin in intensive care units during outbreak control. The amount of third-generation cephalosporins and vancomycin used is expressed as defined daily doses (DDD) per 1000 patients-day. AUD, antimicrobial use density, defined daily doses per 1,000 patients-day.

Fig. 3
Time course of pulsed-field gel electrophoresis typing during the vancomycin-resistant enterococci outbreak.

ACKNOWLEDGEMENTS
This study was financially supported in part by City of Seoul grant no. 10920 and by KICOS project (Battelle Institute-Korea University) grant.
References
1. Bhavnani SM, Drake JA, Forrest A, Deinhart JA, Jones RN, Biedenbach DJ, et al. A nationwide, multicenter, case-control study comparing risk factors, treatment, and outcome for vancomycin-resistant and -susceptible enterococcal bacteremia. Diagn Microbiol Infect Dis. 2000. 36:145–158.
2. Lee K, Jang SJ, Lee HJ, Ryoo N, Kim M, Hong SG, et al. Increasing prevalence of vancomycin-resistant Enterococcus faecium, expanded-spectrum cephalosporin-resistant Klebsiella pneumoniae, and imipenem-resistant Pseudomonas aeruginosa in Korea: KONSAR study in 2001. J Korean Med Sci. 2004. 19:8–14.
3. Oh HS, Kim EC, Oh MD, Choe KW. Outbreak of vancomycin resistant enterococcus in a hematology/oncology unit in a Korean University Hospital, and risk factors related to patients, staff, hospital care and facilities. Scand J Infect Dis. 2004. 36:790–794.
4. Yoo SJ, Sung H, Cho YU, Kim MN, Pai CH, Kim YS. Role of horizontal transfer of the transposon Tn1546 in the nosocomial spread of vanA vancomycin-resistant enterococci at a tertiary care hospital in Korea. Infect Control Hosp Epidemiol. 2006. 27:1081–1087.

5. Recommendations for preventing the spread of vancomycin resistance. Recommendations of the Hospital Infection Control Practices Advisory Committee (HICPAC). MMWR Recomm Rep. 1995. 44:1–13.
6. Muto CA, Jernigan JA, Ostrowsky BE, Richet HM, Jarvis WR, Boyce JM, et al. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus. Infect Control Hosp Epidemiol. 2003. 24:362–386.

7. WHO Collaborating Centre for Drug Statistics Methodology. ATC Index with DDDs. 2001. Norway: WHO.
8. Dutka-Malen S, Evers S, Courvalin P. Detection of glycopeptide resistance genotypes and identification to the species level of clinically relevant enterococci by PCR. J Clin Microbiol. 1995. 33:24–27.

9. Murray BE, Singh KV, Heath JD, Sharma BR, Weinstock GM. Comparison of genomic DNAs of different enterococcal isolates using restriction endonucleases with infrequent recognition sites. J Clin Microbiol. 1990. 28:2059–2063.

10. Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, Persing DH, et al. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol. 1995. 33:2233–2239.

11. Nelson RR, McGregor KF, Brown AR, Amyes SG, Young H. Isolation and characterization of glycopeptide-resistant enterococci from hospitalized patients over a 30-month period. J Clin Microbiol. 2000. 38:2112–2116.

12. de Lencastre H, Brown AE, Chung M, Armstrong D, Tomasz A. Role of transposon Tn5482 in the epidemiology of vancomycin-resistant Enterococcus faecium in the pediatric oncology unit of a New York City Hospital. Microb Drug Resist. 1999. 5:113–129.

13. Byers KE, Anglim AM, Anneski CJ, Germanson TP, Gold HS, Durbin LJ, et al. A hospital epidemic of vancomycin-resistant Enterococcus: risk factors and control. Infect Control Hosp Epidemiol. 2001. 22:140–147.

14. Noskin GA, Stosor V, Cooper I, Peterson LR. Recovery of vancomycin-resistant enterococci on fingertips and environmental surfaces. Infect Control Hosp Epidemiol. 1995. 16:577–581.

15. Zachary KC, Bayne PS, Morrison VJ, Ford DS, Silver LC, Hooper DC. Contamination of gowns, gloves, and stethoscopes with vancomycin-resistant enterococci. Infect Control Hosp Epidemiol. 2001. 22:560–564.

16. Kurup A, Chlebicki MP, Ling ML, Koh TH, Tan KY, Lee LC, et al. Control of a hospital-wide vancomycin-resistant Enterococci outbreak. Am J Infect Control. 2008. 36:206–211.
17. McCarthy KM, Van Nierop W, Duse A, Von Gottberg A, Kassel M, Perovic O, et al. Control of an outbreak of vancomycin-resistant Enterococcus faecium in an oncology ward in South Africa: effective use of limited resources. J Hosp Infect. 2000. 44:294–300.

18. Christiansen KJ, Tibbett PA, Beresford W, Pearman JW, Lee RC, Coombs GW, et al. Eradication of a large outbreak of a single strain of vanB vancomycin-resistant Enterococcus faecium at a major Australian teaching hospital. Infect Control Hosp Epidemiol. 2004. 25:384–390.
19. Hachem R, Graviss L, Hanna H, Arbuckle R, Dvorak T, Hackett B, et al. Impact of surveillance for vancomycin-resistant enterococci on controlling a bloodstream outbreak among patients with hematologic malignancy. Infect Control Hosp Epidemiol. 2004. 25:391–394.

20. Jochimsen EM, Fish L, Manning K, Young S, Singer DA, Baker R, et al. Control of vancomycin-resistant enterococci at a community hospital: efficacy of patient and staff cohorting. Infect Control Hosp Epidemiol. 1999. 20:106–109.

21. Siddiqui AH, Harris AD, Hebden J, Wilson PD, Morris JG Jr, Roghmann MC. The effect of active surveillance for vancomycin-resistant enterococci in high-risk units on vancomycin-resistant enterococci incidence hospital-wide. Am J Infect Control. 2002. 30:40–43.

22. Lucet JC, Armand-Lefevre L, Laurichesse JJ, Macrez A, Papy E, Ruimy R, et al. Rapid control of an outbreak of vancomycin-resistant enterococci in a French university hospital. J Hosp Infect. 2007. 67:42–48.

23. Hendrix CW, Hammond JM, Swoboda SM, Merz WG, Harrington SM, Perl TM, et al. Surveillance strategies and impact of vancomycin-resistant enterococcal colonization and infection in critically ill patients. Ann Surg. 2001. 233:259–265.

24. Brown AR, Amyes SG, Paton R, Plant WD, Stevenson GM, Winney RJ, et al. Epidemiology and control of vancomycin-resistant enterococci (VRE) in a renal unit. J Hosp Infect. 1998. 40:115–124.

25. Quale J, Landman D, Saurina G, Atwood E, DiTore V, Patel K. Manipulation of a hospital antimicrobial formulary to control an outbreak of vancomycin-resistant enterococci. Clin Infect Dis. 1996. 23:1020–1025.

26. Edmond MB, Ober JF, Weinbaum DL, Pfaller MA, Hwang T, Sanford MD, et al. Vancomycin-resistant Enterococcus faecium bacteremia: risk factors for infection. Clin Infect Dis. 1995. 20:1126–1133.

27. Handwerger S, Raucher B, Altarac D, Monka J, Marchione S, Singh KV, et al. Nosocomial outbreak due to Enterococcus faecium highly resistant to vancomycin, penicillin, and gentamicin. Clin Infect Dis. 1993. 16:750–755.

28. Morris JG Jr, Shay DK, Hebden JN, McCarter RJ Jr, Perdue BE, Jarvis W, et al. Enterococci resistant to multiple antimicrobial agents, including vancomycin. Establishment of endemicity in a university medical center. Ann Intern Med. 1995. 123:250–259.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download