Abstract
We report a pulmonary infarction in 68-year-old man who was referred for an asymptomatic pulmonary nodule in chest radiography. Computed tomography (CT), positron emission tomography (PET), and transthoracic needle aspiration suggested suspicion for malignancy. Video-assisted thoracoscopic surgery (VATS) was performed for histologic diagnosis. Our case is a pulmonary nodule due to pulmonary infarction diagnosed by VATS in Korea.
Pulmonary infarctions typically present as wedge-shaped peripheral parenchymal opacities on computed tomography (CT).1 Rarely, however, they present as pulmonary nodules or mass.2,3 An undiagnosed pulmonary nodule or mass should be evaluated by CT, positron emission tomography (PET) scan, and lung biopsy to confirm malignancy.4
We report herein a case of pulmonary infarction presenting an asymptomatic pulmonary nodule which was initially suspected of malignancy and was finally confirmed by video-assisted thoracoscopic surgery (VATS).
A 68-year-old man was referred for an undetermined pulmonary nodule which was revealed by a health check up. He had had hypertension for 10 years and was taking antihypertensive medications. He was a 30 pack-year ex-smoker. On admission, his blood pressure was 120 / 70 mmHg, pulse rate 76/minute, respiratory rate 18/minute, and body temperature 36.6℃. He did not complain any chest symptoms. On physical examination, there were no remarkable findings. Laboratory tests showed no abnormal findings. Sputum examinations for acid-fast bacilli were negative and for cytology were negative for malignancy.
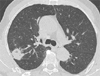
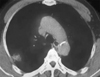
Chest radiography revealed a solitary pulmonary nodule (SPN) in the right upper lobe. Chest CT scan showed a solitary parenchymal opacity with subpleural base, convex borders and focal low attenuation area within density, and 3×2 cm in size in the right upper lobe of the lung. The margin was slightly lobulated, and enhanced by contrast media.
PET-CT scan revealed an abnormal hypermetabolic nodule with maximal standard uptake value of 1.0. CT-guided transthoracic needle aspiration was done for further evaluation of a pulmonary nodule. Cytology showed a few atypical cells and reported suspicion for malignancy. Lung perfusion scan revealed focal perfusion defects in the right upper lobe. To confirm malignancy before radical lung resection, wedge resection was performed by VATS. On gross section, there was a relatively well demarcated mass, measuring 2.3×2.0 cm. The cut surface of mass was yellow, tan colored, necrotic and granular. No thrombi and inflammations around vessels were seen. The doppler ultrasound study of lower extremities revealed no evidence of deep vein thrombosis.
An asymptomatic pulmonary nodule in an elderly patient with 30 pack-year smoking should be evaluated by CT, PET-CT scan and lung aspiration cytology. These studies suspected lung malignancy, but wedge resection via VATS revealed localized pulmonary infarction.
Pulmonary infarctions result from pulmonary thromboembolism, heart failure, vasculitis, infection, and malignancy.1,5 In one study, undiagnosed SPNs or masses were found in 16 patients among 43 patients with pulmonary infarctions diagnosed by surgical lung biopsy.2 Six patients had features suggestive for malignancy on CT scan, PET scan or transthoracic needle aspiration. Fifty-percent of patients received oral anticoagulant therapy, 2 for chronic atrial fibrillation and 1 for deep vein thrombosis.2 In our patient, there were no predisposing factors of venous thromboembolism and no chest symptoms.
Radiologically, pulmonary infarctions appear parenchymal density with broad pleural base, convex borders, linear strands from apex of the infarct toward hilum, truncated apex, broad pleural base, and low attenuation areas within the lesion.6 Pulmonary infarctions could be suggested by peripheral parenchymal opacities with characteristic findings on CT scan. PET-CT scan is usually used in initial and follow up staging of lung cancer. False-positive results can occur in acute inflammation or infectious conditions. Pulmonary embolisms have abnormally hypermetabolic nodules and small occult infarctions also have hypermetabolic nodules in the peripheral lung.7
The transthoracic needle aspiration cytology revealed false-positive results. Histologically, atypical reactive alveolar lining type II cells and metaplastic cells near the infarction can result in this false-positive cytology results.8,9
In cases of the peripheral lung nodules in subpleural regions, the possibility of pulmonary infarctions should be considered, even in the absence of evidence of venous thromboembolism. VATS should be performed to confirm the nature of nodules.
Figures and Tables
References
1. He H, Stein MW, Zalta B, Haramati LB. Pulmonary infarction: spectrum of findings on multidetector helical CT. J Thorac Imaging. 2006. 21:1–7.
2. George CJ, Tazelaar HD, Swensen SJ, Ryu JH. Clinicoradiological features of pulmonary infarctions mimicking lung cancer. Mayo Clin Proc. 2004. 79:895–898.

3. Tsunezuka Y, Hiranuma C, Sato H, Kurumaya H. Pseudotumor due to pulmonary infarction diagnosed by video-assisted thoracoscopic surgery. Ann Thorac Cardiovasc Surg. 1999. 5:402–404.
4. Jeong YJ, Yi CA, Lee KS. Solitary pulmonary nodules: detection, characterization, and guidance for further diagnostic workup and treatment. AJR Am J Roentgenol. 2007. 188:57–68.

5. Tsao MS, Schraufnagel D, Wang NS. Pathogenesis of pulmonary infarction. Am J Med. 1982. 72:599–606.

6. Balakrishnan J, Meziane MA, Siegelman SS, Fishman EK. Pulmonary infarction: CT appearance with pathologic correlation. J Comput Assist Tomogr. 1989. 13:941–945.
7. Kamel EM, McKee TA, Calcagni ML, Schmidt S, Markl S, Castaldo S, et al. Occult lung infarction may induce false interpre-tation of 18F-FDG PET in primary staging of pulmonary malig-nancies. Eur J Nucl Med Mol Imaging. 2005. 32:641–646.

8. Kaminsky DA, Leiman G. False-positive sputum cytology in a case of pulmonary infarction. Respir Care. 2004. 49:186–188.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download