Abstract
Purpose
To assess efficacy of the Pentacam (PTC) and the anterior segment optical coherence tomography (AOCT) for detection of occludable angles.
Materials and Methods
Fourty-one eyes with gonioscopically diagnosed occludable angles and 32 normal open-angle eyes were included. Anterior chamber angle (ACA) and anterior chamber depth (ACD) were measured with PTC and AOCT. Receiver operating characteristic (ROC) curve was constructed for each parameter and the area under the ROC curve (AUC) was calculated.
Results
Values of ACA and ACD measured by PTC and AOCT were similar not only in normal open angle eyes but also in occludable angle eyes. For detection of occludable angle, the AUCs of PTC with ACA and ACD were 0.935 and 0.969, respectively. The AUCs of AOCT with ACA and ACD were 0.904 and 0.947, respectively.
Primary angle closure glaucoma (PACG) is known to be highly prevalent among some ethnic groups, especially those of Mongolian descent.1-5 Foster and Johnson2 have estimated that 1.7 million people in China are bilaterally blind from glaucoma and 91% of them are attributable to PACG. The number of people with a predisposing risk of anatomically occludable angles is estimated to be 28.2 million, and 9.1 million with significantly closed angle.3 For several decades, it is believed that proper prophylactic laser peripheral iridotomy prevents occludable angles from the angle closure attack.6,7 As damage by acute angle closure is irreversible; screening for occludable angles in endemic areas of angle closure is important.
PACG is diagnosed in cases that have an occludable angles combined with glaucomatous optic neuropathy and consistent visual field defect. Gonioscopy is the gold standard for identifying occludable angles, but it requires expertise of a highly skilled examiner. In addition, it is a relatively subjective technique, and intra- and inter-observer reproducibility is poor. There are no uniform gonioscopic criteria to identify angles that require treatment.8,9
The Pentacam (PTC, Oculus Inc., Wetzlar, Germany) and the anterior segment optical coherence tomography (AOCT; SL-OCT™, Heidelberg Engineering, GmbH, Germany) can provide more rapid and quantitative images compared to the conventional gonioscopy. Their cross-sectional images of the anterior chamber angle (ACA) and anterior chamber depth (ACD) may be used to screen for occludable angles.
In the present study, we evaluated the efficacy of PTC and AOCT as a screening tool for the detection of occludable angles.
After obtaining approval of the Institutional Review Board, seventy-three participants were enrolled in this study. Informed consent was obtained from each subject. Subjects with any history of previous ocular trauma or intraocular disease/surgery were excluded. One eye in each subject was randomly chosen for the analysis. Occludable angle was defined when the trabecular meshwork was seen in less than 90 degrees of the angle circumference by gonioscopy without indentation.10
For each subject, ACA and ACD were measured by the PTC and AOCT, respectively, under the uniform dim illumination. Angle images were captured using the horizontal linear scan protocol (from 3-o'clock to 9-o'clock direction) because images of the temporal and nasal angles, can be taken more easily than those of superior and inferior angles and they need no eyelid manipulation to expose the limbus.11 ACA was measured automatically by PTC and AOCT [angle at the angle recess area at 500 µm (ARA 500)].12 ACD was defined as the distance from the posterior vertex of the corneal endothelium to the anterior surface of the crystalline lens along the optical axis. All measurements were repeated twice by single investigator, and an average of 2 measurements was used to further analyses.
The receiver operating characteristic (ROC) curve was constructed for each parameter, and the area under the ROC curve (AUC) was calculated to compare the discriminating ability of each parameter of each instrument.
Statistical analyses other than ROC curves were carried out using SPSS for Windows, version 11.0 (SPSS Inc, Chicago, Il, USA), and statistical analysis for the ROC curves was performed using Medcalc for Windows, version 7.6.0.0 (Medcalc Software, Mariakerke, Belgium).
Among all 73 eyes, 41 eyes had an occludable angle and 32 eyes showed normal open angle by gonioscopy without indentation. Mean ages for occludable angle patients and normal controls were 67.5 ± 8.0 years (range, 54 to 81 years) and 62.2 ± 11.5 years (range, 48 to 84 years), respectively (p = 0.024). Thirteen (31.7%) patients in the occludable angle group and 10 (31.3%) patients in the control group were men.
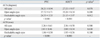
ACA and ACD data obtained by PTC and AOCT are shown in Table 1. Values of ACA measured by PTC and AOCT were similar within each of the two populations (occludable angles; p = 0.012, open angles; p = 0.200). ACD measured by PTC and AOCT showed also similar results in both study groups (occludable angles; p = 0.180, open angles; p = 0.630).
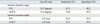
Fig. 1 shows the ROC curves of ACA and ACD, measured by PTC and AOCT. The AUCs of PTC with ACA and ACD were 0.935 (cut-off, 29.5 degrees) and 0.969 (cut-off, 2.27 mm), respectively. The AUCs of AOCT with ACA and ACD were 0.904 (cut-off, 31.8 degrees) and 0.947 (cut-off, 2.45 mm), respectively. Data at these cut-off points are listed in Table 2. With fixed sensitivity of 80.0%, the PTC showed 92.7% (ACA) and 100% (ACD) specificity, and the AOCT showed 85.4% (ACA) and 97.6% (ACD) specificity.
In the present study, anterior chamber images were taken by PTC and AOCT to evaluate their discriminating ability to detect an occludable angle. These two instruments had large AUCs for both ACA and ACD. Especially, ACD by PTC had the largest AUC (0.969), so that ACD measurement by PTC might have the most powerful discriminating ability for the occludable angle detection.
Even though the conventional gonioscopy has been used as a standard method to examine the angle structure, it has several weak points. It requires expertise of a highly skilled examiner, and it uses a relatively subjective classification of angle structure. For these reasons, there have been several attempts to develop new imaging techniques. Redhakrishnan, et al.6,7 reported that there was no significant difference between OCT and ultrasound biomicroscopic parameters of anterior chamber angles. Nolan, et al.13 examined ACA by gonioscopy as well as AOCT. Winifred and associates evaluated sensitivity of OCT in detecting angle closure compared with gonioscopy.14 Using gonioscopy as reference standard, results in AOCT showed a sensitivity of 81.5% and a specificity of 68.5% in the nasal quadrant; 66.1% and 77.2% in the temporal area. However, it was a qualitative comparison of anterior chamber angles. In the present study, these two instruments (AOCT and PTC) showed good results. Therefore, not only AOCT but also PTC may be excellent candidates for screening of occludable angles.
As for inter-device agreement and cut-off value distinguishing occludable angle, ACD was better than ACA using both PTC and AOCT. And, even though statistically not significant, ACA in occludable angle patients showed slight differences between PTC and AOCT (p = 0.012). There are some possible explanations for these findings. It is possible that the contact gonioscopy lens for conventional gonioscopy, when placed on the globe, causes some displacement of anterior segment structures, while the use of Zeiss-type gonioscopic lens causes no pressure on the eye, resulting in opening of the angles. Furthermore, although gonioscopy, PTC, and AOCT examinations are undertaken under dim lighting conditions, the intensity of light illuminated during each examinations is different from each other. This is inevitable for both the production of Scheimpflug images in PTC and the slit beam in case of gonioscopy. Light of varying intensity can open the angle to a different degree, especially in patients with an occludable angle. Ultrasound biomicroscopic studies demonstrate the dramatic changes in angle width that take place when going from dark to light.15 However, unlike ACA; ACD is less influenced by light. This suggests that the difference in light intensity used during each examination could be an important factor for the difference in range of agreement between ACA and ACD.
In conclusion, we have shown that the quantitative angle parameters and anterior chamber depths, as measured by PTC, have similar mean values, reproducibility, and sensitivity-specificity profiles when compared with measurements obtained by AOCT. In this limited data set, these parameters showed discriminative cut-off value in the screening of occludable angles. The ease of image acquisition and the non-contact nature of PTC and AOCT are highly desirable. ACA and ACD using both modalities could have a novel potential application for screening of eyes with occludable instead of gonioscopic examination. Further study with a larger sample size is required to clearly define the utility of PTC and AOCT parameters (ACA, ACD) in screening of occludable angle and angle-closure glaucoma.
Figures and Tables
 | Fig. 1Receiver operating characteristic curves. (A) Anterior chamber angle by Pentacam. (B) Anterior chamber angle by Anterior segment optical coherent tomography. (C) Anterior chamber depth by Pentacam. (D) Anterior chamber depth by anterior segment optical coherent tomography. |
References
1. Bonomi L, Marchini G, Marraffa M, Bernardi P, De Franco I, Perfetti S, et al. Epidemiology of angle-closure glaucoma: prevalence, clinical types, and association with peripheral anterior chamber depth in the Egna-Neumarket Glaucoma Study. Ophthalmology. 2000. 107:998–1003.
2. Foster PJ, Johnson GJ. Glaucoma in China: how big is the problem? Br J Ophthalmol. 2001. 85:1277–1282.

3. Alsbirk PH. Anterior chamber depth and primary angle-closure glaucoma. I. An epidemiologic study in Greenland Eskimos. Acta Ophthalmol (Copenh). 1975. 53:89–104.
5. Dandona L, Dandona R, Mandal P, Srinivas M, John RK, McCarty CA, et al. The Andhra Pradesh eye disease study. Angle-closure glaucoma in an urban population in southern India. Ophthalmology. 2000. 107:1710–1716.

6. Radhakrishnan S, Goldsmith J, Huang D, Westphal V, Dueker DK, Rollins AM, et al. Comparison of optical coherence tomography and ultrasound biomicroscopy for detection of narrow anterior chamber angles. Arch Ophthalmol. 2005. 123:1053–1059.

7. Radhakrishnan S, Huang D, Smith SD. Optical coherence tomography imaging of the anterior chamber angle. Ophthalmol Clin North Am. 2005. 18:375–381. vi

8. Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002. 86:238–242.

10. Foster PJ, Devereux JG, Alsbirk PH, Lee PS, Uranchimeg D, Machin D, et al. Detection of gonioscopically occludable angles and primary angle closure glaucoma by estimation of limbal chamber depth in Asians: modified grading scheme. Br J Ophthalmol. 2000. 84:186–192.

11. Lackner B, Schmidinger G, Skorpik C. Validity and repeatability of anterior chamber depth measurements with Pentacam and Orbscan. Optom Vis Sci. 2005. 82:858–861.
12. Gazzard G, Foster PJ, Friedman DS, Khaw PT, Seah S. Light to dark physiological variation in irido-trabecular angle width. Br J Ophthalmol. 2004. 88:1357–1482. Video report. http://bjo.bmjjournals.com/cgi/content/full/88/11/DC1/1.
13. Nolan WP, See J, Aung T, Ce Z, Radhakrishnan S, Friedman DS, et al. Detection of patients at risk of angle-closure using anterior segment OCT. Invest Ophthalmol Vis Sci. 2005. 46:E-Abstract 145.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download