Abstract
Purpose
Hepatitis A virus (HAV) has been a leading cause of acute hepatitis in Korea. The reported genotypes of acute hepatitis A in Korea are the subgenotype IA and IB. The aim of the present study is to investigate HAV genotypes in the south-east area of Gyeonggi-do in Korea.
Materials and Methods
From June 2004 to June 2006, 46 acute hepatitis A patients were enrolled prospectively. All had sporadic acute hepatitis A patients. All suspected cases of acute hepatitis A were tested for IgM anti-HAV antibodies. We sequenced 168 bp of nucleotides of the putative VP1/P2A junction and determined the HAV genotype with reverse transcriptase polymerase chain reaction. The clinical and laboratory results of all patients were recorded.
Hepatitis A virus (HAV) is classified as Hepatovirus within the Picornaviridae.1 In virology, HAV is a positively stranded ribonucleic acid (RNA) virus of about 7,500 nucleotides.2 The viral capsid is composed of three exposed polypeptides VP1, VP2, VP3, and a putative VP4, with a highly conserved antigenic structure.3 HAV is transmitted through fecal to oral route and is diagnosed by positive serum IgM anti-HAV antibody test. Isolates of HAV are of a single serotype, but human isolates can be categorized into three genotypes (I, II and III) with 2 subgenotypes (A and B for I and III). Genotype I is the most abundant type worldwide, and particularly IA is found in North America, Europe, China, Japan, the former USSR and Thailand. Strains of subgenotype IIIA have been collected from humans infected with HAV in India, Sri Lanka, Nepal, Malaysia and the USA.3,4 For the past several years, studies on HAV have not been performed because most people in Korea carry the HAV antibody by natural infection. Once HAV antibodies are acquired, they give life-long immunity. Moreover, hepatitis A infection is usually mild in children, and rarely progresses into chronicity and fulminant hepatitis.5,6 However, the high risk for HAV infection in Korea has been focused on young adults and adolescents who, did not get infected in childhood due to improved hygiene measures, and are more prone to infection later in life with more serious disease.7-9 In 2001, sporadic acute hepatitis A was reported in Korea, being subgenotype IA.7 In 2007, an outbreak of acute hepatitis A in a Korean hospital was reported, and the subgenotypes of this hepatitis A virus were found to be IA and IB.10
HAV phylogenetic studies can provide important information for the design of appropriate public health cares and HAV genotypic changes. Therefore, we investigated the genotypes of recently isolated HAV cases in the south-east area of Gyeonggi-do in Korea.
From June 2004 to June 2006, 46 patients from the Bundang CHA Hospital were identified prospectively. All patients, showing clinical and biochemical signs of acute hepatitis A and serological evidence of acute hepatitis A, were classified as acute hepatitis A patients. The serological evidence was obtained with IgM anti-HAV antibody tests (EIA, VIDAS, BioMérieux, Marcy-I'Etoile, France). Patients lived in the south-east area of Gyeonggi-do (Seongnam-si, Icheon-si, Gwangju-si) in Korea and all were Koreans.
During the two study years, there was no reported outbreak of acute hepatitis A in the study area. Routine contact tracing was done. All patients visited a hospital as an outpatient once a week for two or three weeks. All cases were sporadic acute hepatitis A.
Ten mL of whole blood was collected from the veins of each patient in order to analyse the genotype of HAV. Each sample was numbered in order of date. The whole blood was centrifuged to separate the serum. The serum was preserved at -20℃. For the study, sera of the enrolled patients were numbered from 1 to 46. The study was approved by the local ethical committee and conform to ethical guidelines of the Declaration of Helsinki. Informed consent was obtained from each patient enrolled in the study.
Viral RNAs extracted from serum using Viral-spin™ (Intron, Korea) were used for the synthesis of first-strand complementary DNAs (DNAs) by reverse transcriptase. Reverse transcription was performed for 1.5 h at 42℃ in a final reaction volume of 20 µL containing 7.5 µL of the purified total RNA, 4 µL of 5 × reaction buffer (Promega, Madison, WI, USA), 5 µL of dNTPs (each 2 mM), 2 µL of 10 µM hexamer, 0.5 µL of RNasin® RNase Inhibitor (40 U/µL; Promega), and 1 µL of Moloney murine leukemia virus reverse transcriptase (200 U/µL; Promega).
The cDNA obtained was amplified by poly chain reaction (PCR) by using oligonucleotides, designed on the basis of sequence alignments.12 PCR was performed for 40 cycles (0.5 min at 94℃, 1.5 min at 50℃, and 1.5 min at 72℃) in a final reaction volume of 20 µL containing 5 µL of the cDNA reaction mixture, 0.5 µM each primer and 10 µL 2X master mix (Seegene).
The target PCR products within the agarose gel were purified for sequencing using the QIAquick® PCR purification kit (QIAGEN) and cloned into a TOPO TA cloning vector (Invitrogen, Carlsbad, CA, USA) according to the manufacturer's instructions. The cloned plasmids were sequenced in ABI PRISM® 3100 Genetic Analyzer (Applied Biosystems, Foster City, CA, USA).
The target PCR products were re-amplified and extracted from the gel using the GENCLEAN II Kit (Q-BIO gene, Carlsbad, CA, USA), and directly sequenced with ABI PRISM®3100-Avant Genetic Analyzer (Applied Biosystems, Foster City, CA, USA) using a HAV specific primer (5'-GTCTACCAGGCATTCGCTTCAT-3').
The CLUSTAL W (version 1.83) program was used to generate the phylogenetic tree. The putative VP1/2A junction sequences were amplified and sequenced from clinical samples and compared with the corresponding Gene Bank reference sequences for genotypes. IA : AF234864 (KU97-1), AF234876 (KU98-42), AB020567, L07717 (PRC37). IB : L07700 (Ag11). II : L07693 (CF-53). IIIA : AJ299467 (NOR-24), L07668 (GA76), L07688 (H-122), L07725 (India90), L20530 (A-177). IIIB : L07729 (SLF88). The amino acid alignments of the putative VP1/P2A junction in this study summitted to Genebank were numbered : FJ372930 - FJ372970.
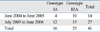
Forty six patients were enrolled in this study. Among the total 46 patients, 21 were male and 25 were female. The mean age was 31 ± 6 years. The mean period of hospitalization was 11 ± 6 days. The baseline clinical and laboratory results are summarized in Table 1. Most clinical and laboratory results of each genotype did not show differences between the genotypes. Case of co-infection with HBV or HCV was not found. The yearly distribution according to genotype is shown in Table 2.
We found that sera from 41 out of 46 patients were positive for HAV-RNA. As can be seen in the phylogenetic tree, the HAV sequrences from 25 patients (60%) out of 41 ones were found to be of subgenotype IIIA , and HAV sequences from 16 patients (40%) were confirmed as subgenotype IA (Fig. 1). Compared to the formerly reported subgenotype IA in Korea,7 the subgenotype IA in our investigation showed > 95% sequence homology.
Several amino acid substitutions were found in subgenotype IA and IIIA. The 2A-19 substitution was found in ten samples of subgenotype IA. The substitution of 2A-19 is identical to fulminant hepatitis of AB020567 in Japan. On the serum No. 37, glutamic acid of 2A-11, on L07717 and L07716 found in China was substituted by aspartic acid. On the serum No. 26, arginine of 2A-6, on L20550 found in Japan was substituted by glycine.
On serum No. 18 of subgenotype IIIA, valine of VP1-288 was substituted by arginine. On serum No. 45, glutamine of 2A-25 was substituted by arginine. On serum No. 7 and 36, methionine of VP1-276 was substituted by arginine. On serum No. 9, methionine of VP1-276 was substutited by leucine, and aspartatic acid of VP1-283 was substituted by glycine. On serum No. 10, lysine of 2A-18 was substituted by glutamic acid.
The founding works on HAV genetic variability made use of discrete, selected partial HAV genomic regions, such as the C terminus of VP3 to the N terminus of VP1 or the putative VP1/P2A junction region. HAV genotype is defined as a group of viruses with > 85% nucleotide sequence identity within one of these regions. Genotypes I and III are further subdivided into two distinct subgroups, which differ in sequence in no more than 7.5% of base positions.3,4,11 The subgenotypes, IA and IB have been reported in Korea.7,10 In conclusion, the three genotypes (IA, IB, IIIA) are co-circulating in Korea. It has been reported before that genetic changes are rare in the HAV genome, which is unlike other RNA viruses.12 Also, nationwide research of HAV genotypic distribution in Korea has not yet been performed. It can be hypothesized that the influx from the other regions of Korea or predominant countries is one of the causes in the subgenotype IIIA circulating in Korea. It was reported that the dominant HAV genotype in India, Sri Lanka, Nepal, and Malaysia is IIIA, even though the research was insufficient.13 Recent reports showed that the HAV subgenotype IIIA in those countries has continuously been the circulating type.14,15 The acute hepatitis A samples gathered from this research area and subgenotype IIIA dominant country need to be compared by further molecular analysis. To verify possible infection from travel, 41 patients, detected with HAV-RNA, were questioned about their travel history. One patient (No. 22, subgenotype IA) had a travel history to Philippines 15 days before hospitalization. Tjon et al.17 reported that HAV subgenotype IIIA was found in homeless, bad hygiene patients and intravenous drug users. However, these trends were not found in this research.
The outbreak of HAV subgenotype IIIA has been reported among intravenous drug users in Europe.16-18 Up to date, HAV has been known to be transmitted through fecal to oral route. However, by the outbreak of the subgenotype IIIA of intravenous drug users and infection of HAV in hemophilia patients by clotting factor,19 it can be possible that HAV is also transmitted by the parenteral route. This change of mode of transmission is likely due to nucleotide variability that reach 4% of the subgenotype IIIA, and it is also possible that HAV has high selection pressure through fecal to oral route and infection through blood has low selection pressure.20,21 The nucleotide variability of the HAV subgenotype IIIA needs to be studied through continuous molecular study in Korea. Through the research, future outbreaks of the subgenotype IIIA in intravenous drug users and blood products can be predicted.
Little information is available on the possible relation between the severity of hepatitis A and the infecting genotype.22,23 It was previously considered that HAV disease severity is linked to individual host factors such as age and underlying liver disease. However, through continuous investigation of HAV, many factors that affect the severity of acute hepatitis A have been proven. First, it has been reported that nucleotide variations in the central portion of the 5' NTR of HAV could affect the severity of acute hepatitis A.24 Low or undetectable HAV viral load and a high bilirubin level could independently affect the progression to fulminant hepatitis. It has also been reported that HAV genotype did not affect the progress to fulminant hepatitis.23 The present study found also similar number of subgenotypes IA and IIIA in the same research area, thus making it possible to directly compare their clinical and laboratory results. Most clinical and laboratory results of each genotype did not reveal any differences between the genotypes, but it showed that mean peak total bilirubin (TB) level in subgenotype IIIA is significantly higher (data not shown). Also, the mean TB level on admission showed a high level of tendency on subgenotype IIIA, even though it is not statistically significant. However, difference has limitations, mostly stemming from this study's small sample size, small area of study and selection of patients. Future work is required to ascertain the difference of total bilirubin according to genotype.
The nucleotide sequence heterogeneity found in our study of the HAV genome of these 41 virus strains results in only limited differences in the amino acid sequence. Among all of the subgenotype IA and IIIA, amino acid sequence differences showed to be maximum 3% (2/56). On the former prevalent subgenotype IA of Korea, it was reported that lysine 2A-10 was substituted by arginine, and glutamine 2A-19 by serine.7 However, our study showed that substitution of 2A-10 did not occur in every sample, and substitution of 2A-19 occurred only in 10 of 16 patients who showed subgenotype IA.
In conclusion, this study examined HAV subgenotype IIIA in Korea, and the results showed that three HAV subgenotypes (IA, IB, IIIA) co-circulate in Korea. The genetic relatedness of HAV from Korea provides valuable new data on the distribution of subgenotype IIIA.
Figures and Tables
Fig. 1
Phylogenetic relationship of HAV gene from DNA extracted with known reference sequences by neighbor-joining analysis using CLUSTAL W (1.83). Bootstrap values above 80% from 100 replicates are also shown (L07700 is genotype IB, L07693 is genotype II, L07729 is genotype IIIB).

References
1. Melnick JL. Properties and classification of hepatitis A virus. Vaccine. 1992. 10:Suppl 1. S24–S26.

2. Martin A, Lemon SM. Hepatitis A virus: from discovery to vaccines. Hepatology. 2006. 43:S164–S172.

3. Robertson BH, Jansen RW, Khanna B, Totsuka A, Nainan OV, Siegl G, et al. Genetic relatedness of hepatitis A virus strains recovered from different geographical regions. J Gen Virol. 1992. 73:1365–1377.

4. Jansen RW, Siegl G, Lemon SM. Molecular epidemiology of human hepatitis A virus defined by an antigen-capture polymerase chain reaction method. Proc Natl Acad Sci U S A. 1990. 87:2867–2871.

5. Gust ID. Epidemiological patterns of hepatitis A in different parts of the world. Vaccine. 1992. 10:Suppl 1. S56–S58.

6. Koff RS. Clinical manifestations and diagnosis of hepatitis A virus infection. Vaccine. 1992. 10:Suppl 1. S15–S17.

7. Byun KS, Kim JH, Song KJ, Baek LJ, Song JW, Park SH, et al. Molecular epidemiology of hepatitis A virus in Korea. J Gastroenterol Hepatol. 2001. 16:519–524.

8. Lee TH, Kim SM, Lee GS, Im EH, Huh KC, Choi YW, et al. [Clinical features of acute hepatitis A in the Western part of Daejeon and Chungnam province: single center experience]. Korean J Gastroenterol. 2006. 47:136–143.
9. Kang CI, Choi CM, Park TS, Lee DJ, Oh MD, Choe KW. Incidence and seroprevalence of Hepatitis A virus infections among young Korean soldiers. J Korean Med Sci. 2007. 22:546–548.

10. Park JY, Lee JB, Jeong SY, Lee SH, Lee MA, Choi HJ. Molecular characterization of an acute hepatitis A outbreak among healthcare workers at a Korean hospital. J Hosp Infect. 2007. 67:175–181.

11. Costa-Mattioli M, Di Napoli A, Ferré V, Billaudel S, Perez-Bercoff R, Cristina J. Genetic variability of hepatitis A virus. J Gen Virol. 2003. 84:3191–3201.
12. Poovorawan Y, Theamboonlers A, Chongsrisawat V, Jantaradsamee P, Chutsirimongkol S, Tangkijvanich P. Clinical features and molecular characterization of hepatitis A virus outbreak in a child care center in Thailand. J Clin Virol. 2005. 32:24–28.
13. Khanna B, Spelbring JE, Innis BL, Robertson BH. Characterization of a genetic variant of human hepatitis A virus. J Med Virol. 1992. 36:118–124.

14. Hussain Z, Das BC, Husain SA, Asim M, Chattopadhyay S, Malik A, et al. Hepatitis A viral genotypes and clinical relevance: Clinical and molecular characterization of hepatitis A virus isolates from northern India. Hepatol Res. 2005. 32:16–24.
15. Arankalle VA, Sarada Devi KL, Lole KS, Shenoy KT, Verma V, Haneephabi M. Molecular characterization of hepatitis A virus from a large outbreak from Kerala, India. Indian J Med Res. 2006. 123:760–769.
16. Spada E, Genovese D, Tosti ME, Mariano A, Cuccuini M, Proietti L, et al. An outbreak of hepatitis A virus infection with a high case-fatality rate among injecting drug users. J Hepatol. 2005. 43:958–964.

17. Tjon GM, Götz H, Koek AG, de Zwart O, Mertens PL, Coutinho RA, et al. An outbreak of hepatitis A among homeless drug users in Rotterdam, The Netherlands. J Med Virol. 2005. 77:360–366.
18. Wells R, Fisher D, Fenaughty A, Cagle H, Jaffe A. Hepatitis A prevalence among injection drug users. Clin Lab Sci. 2006. 19:12–17.
19. Jee YM, Go U, Cheon D, Kang Y, Yoon JD, Lee SW, et al. Detection of hepatitis A virus from clotting factors implicated as a source of HAV infection among haemophilia patients in Korea. Epidemiol Infect. 2006. 134:87–93.

20. Stene-Johansen K, Jonassen Tø, Skaug K. Characterization and genetic variability of Hepatitis A virus genotype IIIA. J Gen Virol. 2005. 86:2739–2745.

21. Cuthbert JA. Hepatitis A: old and new. Clin Microbiol Rev. 2001. 14:38–58.
22. Yokosuka O. Does genotype of hepatitis A virus relate to clinical characteristics of hepatitis A? Hepatol Res. 2005. 32:14–15.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download