Abstract
Purpose
The aim of this study was to evaluate new cardiac deformity indexes (CDIs) for diagnosis of pectus excavatum as well as morphological assessment of heart on computed tomography (CT).
Materials and Methods
We retrospectively evaluated the CT images of the control group (n=200), and the pectus excavatum before and after correction groups (n=178), and calculated the CDIs; cardiac compression index (CCI), and cardiac asymmetry index (CAI). We also calculated chest wall compression index (CWCI) and asymmetry index (CWAI) on the axial images. We performed logistic regression analysis using each index and age as predictor variables.
Results
The CDIs (CCI and CAI) were significant (p < 0.05) in the diagnosis of pectus excavatum, regardless of age (p = 0.4033, p = 0.8113). The CWCI and CWAI were significant (p < 0.05) and significantly affected by age (p < 0.05). If we selected 1.82 as the cutoff of the CCI, the sensitivity and specificity were 99.4% and 98%, respectively. The following cutoffs and the sensitivity and specificity were obtained: 1.15 for the CAI gave 94.4% and 94.5%, 3.05 for the CWCI gave 92.1% and 92%, and 1 for the CWAI gave 62.4% and 65%, respectively. The CCI after repair improved from 2.83 ± 0.84 to 1.84 ± 0.33, while the CWCI improved from 4.49 ± 1.61 to 2.57 ± 0.44.
Pectus excavatum, also known as funnel or sunken chest, consists of a depression of the sternum so that the ribs on each side protrude anteriorly more than the sternum itself. It is generally believed to be due to a genetically determined abnormality of the sternum and portions of the diapgram.1 The vast majority of patients are asymptomatic, except for the anxiety in some patients due to their phy-sical deformity.1 Nevertheless, cardiac or respiratory symptoms are occasionally attributed to this abnormality.2
Chest surgeons are convinced that children with severe pectus excavatum can safely be corrected with predictably normal chest wall growth and development during their pubertal growth spurt. The severity of the defect is best quantified by computed tomography (CT) or magnetic resonance imaging. The "chest wall compression index (so called Haller index)" can be derived by dividing the transverse diameter of the chest by the anteroposterior (AP) diameter. Individual patients may have chest characteristics that impact the result of repair, some of which would unlikely be measured by the Haller index. For example, asymmetry of the chest and morphological changes of the heart secondary to pectus excavatum are not included.
The purpose of this study was to develop new cardiac deformity indexes (CDIs) on CT scan for the evaluation of pectus excavatum, and to compare the CDIs with pre-existing chest wall compression index. We also evaluated the result of repair using CDIs and chest wall indexes. To our best knowledge, the new CDIs of pectus excavatum, measured by our technique, have not been described.
In this retrospective study, two hundred patients (100 men and 100 women; age range, 3-22 years; mean age, 13 years) without cardiac disease, chronic illness, or chest wall deformity were included in the control group. Ten patients (5 men and 5 women) were included in each of the age.
We also included 178 consecutive patients in the pectus excavatum group (137 men and 41 women; age range, 3-30 years; mean age, 10 years) who had surgical correction of their pectus excavatum between March 2006 and May 2007. All patients underwent multidetector CT (MDCT) before and after (1-2 weeks) the surgical procedure. In our study design, we included three groups: a control group and two groups of before and after correction of pectus excavatum.
MDCT scans were obtained using a commercial 64-channel MDCT (Brilliance 64; Philips, Cleveland, Ohio, USA). MDCT scans were performed with the scanners set at 120 kVp and 35-50 mAs using the automatic tube current modulation with a pitch of 0.673 and collimation of 40-mm (64 × 0.625). The rotation time was 0.75. Dose modulation (D-DOM) was applied during acquisitions.
Images were reconstructed at 5.0 mm thick sections with a soft tissue algorithm. Patients were scanned craniocaudally during a full-inspiration breath hold. No patients received intravenous contrast material in the pectus excavatum group. In the control group, all of 200 patients except one patient received intravenous nonionic contrast material (2 mL/Kg, Ultravist 370; Schering, Berlin, Germany).
We (M. K and K. Y. L) independently selected two transverse images from each of the 556-MDCT scans and measured 7 diameters as variables. Measurements were made at 2 levels for each examination as follow; at level 1 (the upper xiphoid process, bone or cartilage, a little below the xiphisternal junction) for the chest wall index, and at level 2 (one or two of the upper image of level 1; the lowest part of the ovoid cardiac contour) for the cardiac index (Fig. 1).
The depression in the pectus excavatum is usually deepest a little above the xiphisternal junction.2 The xiphisternal junction can hardly be detected in some children by the transverse image alone, because the image shows cartilage, but not sufficient ossification. The upper portion of the xiphoid process was a constant, easily identifiable landmark in the control and pectus excavatum groups, regardless of the ossification. The transverse (T), middle AP (D), right AP (R), and left AP (L) diameters were the variable for determining the chest wall index. The transverse (H), middle AP (M), and paramedian (P) diameters were the variable for determining the CDIs.
Measurements were made from the soft copy using a picture archive and communication system, using a one by one format, for each of the two selected levels (Fig. 1).
The CDIs are cardiac compression index (CCI) derived by H/M ratio and cardiac asymmetry index (CAI) derived by P/M ratio. The T/D ratio indicates the chest wall compression index (CWCI), and the L/R ratio indicates the chest wall asymmetry index (CWAI) (Fig. 1).
The values measured from two readers were averaged, and the mean values for continuous variables were then reported as mean ± standard deviation.
The following analyses were performed. For the descriptive data analysis, the distribution of 7 diameters (T, D, R, L, H, M, P) were graphically depicted as a box-and-whisker for the three groups. We then calculated 4 indexes (CCI, CAI, CWCI, CWAI) and depicted the box-and-whisker plots for the three groups (not shown).
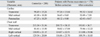
To determine the ability to detect the presence of pectus excavatum, we performed logistic regression analysis using SAS/STAT (version 9.1; SAS, Cary, NC) software. A p value of less than 0.05 was considered to indicate statistical significance. The predicted probability of having pectus excavatum was computed from the fitted model. We obtained a series of sensitivities and specificities from each fitted logistic regression model, and used the area under the ROC curve (AUC) to compare with the performance discrimination. We got individual subtraction of 4 indexes before and after correction of pectus excavatum for evaluation of the result after corrective operation. In addition, we performed logistic regression analysis using each index and age as predictive variables to discriminate the before correction group from the control group. From the results of Table 3, we plotted the 4-ROC curve for evaluating the performance of the 4 indexes. The ROC curves of the CCI and CAI were obtained after removing the age variable from the model. The ROC curves of the CWAI and CWAI were obtained from the model that contained the age variable. It is true that the larger the area under the curve (AUC), the better the predictions.
The inter-observer correlation coefficient for the 7 variables was very high (0.934-0.998).
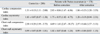
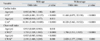
Means and standard deviations of the 7 variables of the heart and chest wall in the three groups are listed in Table 1. Table 2 shows means and standard deviations of the 2 cardiac funnel and chest wall indexes in the three groups.
The CCI (H / M) was 2.83 ± 0.84 before and 1.84 ± 0.33 after correction due to increased middle AP diameter (M: 52.49 ± 7.20) after correction. The CWCI (T / D) was 4.49 ± 1.61 before and 2.57 ± 0.44 after correction due to decreased transverse diameter (T: 191.81 ± 36.7) and increased middle AP diameter (D: 75.46 ± 12.22) after correction.
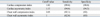
We calculated AUC of each model (Fig. 2) for CCI (0.999), CAI (0.989), CWCI (0.978) and CWAI (0.702). In general, the discrimination was excellent (AUC > 0.8) or outstanding (AUC > 0.9). Therefore, except for CWAI, three of the indexes seemed to be outstanding. In particular, the CCI showed the best performance among the indexes. If we selected 1.15 as the cutoff of the CAI, the sensitivity and specificity were then 94.4% and 94.5%, respectively, without the age variable. If we selected the cutoff of the CWCI as 3.05, then this gave 92.1% and 92% for the sensitivity and specificity, respectively, and CWAI 1 gave 62.4% and 65% for the sensitivity and specificity, respectively, without the age variable (Table 3).
The results of the logistic regression analyses are presented in Table 4. The results indicate that CCI and CAI were significant (p < 0.05, p < 0.05, respectively), however, the age factor was not significant (p > 0.05, p > 0.05, respectively), implying that, if we use the CCI and CAI to discriminate pectus excavatum in the before correction group from the control group, then it is not necessary to consider the age factor. In contrast, CWCI and CWAI (p > 0.05, p > 0.05, respectively) and age (p > 0.05) were all significant, indicating that the use of CWCI or CWAI for discrimination of pectus excavatum needs to consider the age of patient.
Preoperative CCI in 178 patients with pectus excavatum was 2.83 ± 0.84, and it significantly improved to 1.84 ± 0.33 and the CWCI also improved from 4.49 ± 1.61 to 2.57 ± 0.44. Preoperative CAI of pectus excavatum was 1.75 ± 0.55 and decreased to 1.20 ± 0.19 after Nuss procedure. CWAI was 1.02 ± 0.07 preoperatively and decreased to 0.99 ± 0.04 postoperatively (Table 2).
The radiographic findings of pectus excavatum have been well described, and they include displacement of the heart into the left hemithorax with mild clockwise rotation and a pancake-like appearance of the heart with an increase of the frontal silhouette to the left.2 The possible mechanisms that produce circulatory problems in individuals with pectus excavatum include: 1) decreased inflow due to cardiac rotation and twisting of the great veins; 2) cardiac compression, especially of the atria, resulting in supraventricular; 3) impaired diastolic expansion; and 4) decreased respiratory effort.2
Minimally invasive repair of pectus excavatum (MIRPE) is a new surgical technique, recently developed by Nuss, and has extensively been practiced by our group (HJP). This procedure involves slipping one or more concave steel bars into the chest, underneath the sternum. The bar is flipped to a convex position so as to push outward on the sternum, thereby correcting the deformity. The bar usually stays in the body for about two years in children, but three or four years in adults. The closed or Nuss procedure for pectus excavatum results in a significant improvement in better cosmetic appearance3-6 and cardiopulmonary function.7-10 In the present study, CCI and CWCI were improved after Nuss procedure, indicating decompression of the heart and chest wall.
In determination of the need for surgery, only CWCI has been used for several decades to evaluate the severity of pectus excavatum. In one series, the normal value of this index was found to be 2.56 (± 0.35 SD), and the investigators suggested that patients with a ratio of 3.25 or greater require surgical correction. A similar index derived from CT measurements has been employed to assess the results of surgical repair and Kim et al. developed new indexes for assessment of chest wall deformity.12,13 However, their indexes are focused mainly on chest wall shape rather than the cardiac shape. In the present study, we found that CDIs were highly reliable for diagnosing pectus excavatum and evaluating the result of repair as well as the cardiac shape. For the discussion of cardiopulmonary improvement after repair, anatomical evaluation using imaging studies is essential. The CCI (cutoff; 1.82), the CAI (cutoff; 1.15) and the CWCI (cutoff; 3.05) guarantee more than 90% for the sensitivity and specificity to discriminate pectus excavatum. The CCI has the best performance among the indexes and showed high correlation with CWCI. We, therefore, can propose objective numerical values by using the CDIs for quantifying cardiac compression and cardiac asymmetry. We consider that the CDIs can provide information about the degree of cardiac compression and asymmetry, and that impact on the surgical outcome would help physicians counsel patients as to what surgical outcome they could expect. To be considered as an effective tool that fulfills this purpose, the CDIs showed reproducibility by individual observers and solid inter-observer agreement. Furthermore, according to our present result, we must consider the age of patient as a predictive variable if we use the Haller index as a predictive variable to discriminate the before correction group from the control group. On the other hand, it is not necessary to consider the patient's age if we use CDIs as the predictive variable. The CDIs were consistent, and are expected to be useful for determination of the prognosis on follow-up CT after correction with Haller index.
The limitations of our study include the followings: 1), there was no absolute anatomical reference standard for measuring the cardiac diameter. We determined the upper xiphoid process to be the narrowest AP diameter of the chest wall. To determine two reference levels, we sometimes accepted the consensus of two readers as a reference standard for the level before measurement. It seemed even more difficult to assess the diameter after repair, because of beam hardening artifact which was caused by one or two metallic bars, 2) we did not study preoperative and postoperative function to assess the cardiac function such as 2-D echocardiography because this was a retrospective study. Therefore, more studies are necessary to identify the correlation between CDIs and cardiac function.
In conclusion, the CDIs such as CCI and CAI focusing the cardiac deformity are potentially useful tools to evaluate pectus excavatum preoperatively and estimate the result of repair with the use of chest wall compression index. Furthermore, they will be useful in predicting physiological outcomes of the heart.
Figures and Tables
Fig. 1
Pre-enhanced transverse CT images in a 20-year-old man with pectus excavatum. (A) CT image obtained at the upper xiphoid process shows 4 variables for the thoracic index before correction. The line T (transverse diameter of the chest wall) indicates the widest inner transverse diameter of the thoracic cage. The line D (AP diameter of the chest wall) indicates the narrowest inner diameter from the xiphoid process to the anterior surface of the vertebral body. The lines R and L indicate the widest AP diameter in both, respectively. (B) CT image obtained at one upper level of (A) shows the 3 variables for the CDIs before correction. The line H (transverse diameter of heart) indicates the widest transverse diameter of the heart. The line M (AP diameter of the heart) indicates the narrowest diameter of the heart at the xiphoid process. The line P (paramedian diameter of the heart) indicates the widest paramedian AP diameter of the heart. (C) The CT image obtained at one upper level of the upper xiphoid process shows 3 variables for the CDIs after correction.

Fig. 2
Receiver operating characteristic (ROC) curves show the ability of cardiac compression (CCI), cardiac asymmetry (CAI), chest wall compression (CWCI), and chest wall asymmetry (CWAI) to reveal pectus excavatum as defined (A) without and with (B) age applied as a variable. AUC, area under the curve.
Table 1
Mean Values of 7 Diameters in the Control Group and the of before and after Correction of Pectus Excavatum Groups
References
1. Guller B, Hable K. Cardiac findings in pectus excavatum in children: review and differential diagnosis. Chest. 1974. 66:165–171.

2. Wachtel FW, Ravitch MM, Grishman A. The relation of pectus excavatum to heart disease. Am Heart J. 1956. 52:121–137.
3. Nuss D, Kelly RE Jr, Croitoru DP, Katz ME. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg. 1998. 33:545–552.
4. Park HJ, Lee SY, Lee CS, Youm W, Lee KR. The Nuss procedure for pectus excavatum: evolution of techniques and early results on 322 patients. Ann Thorac Surg. 2004. 77:289–295.

5. Park HJ, Lee SY, Lee CS. Complications associated with the Nuss procedure: analysis of risk factors and suggested measures for prevention of complications. J Pediatr Surg. 2004. 39:391–395.

6. Park HJ. Technical Innovations in minimally invasive approach for pectus excavatum: a paradigm shift through 630 patients. Innovations. 2007. 2:25–28.

7. Sigalet DL, Montgomery M, Harder J. Cardiopulmonary effects of closed repair of pectus excavatum. J Pediatr Surg. 2003. 38:380–385.

8. Borowitz D, Cerny F, Zallen G, Sharp J, Burke M, Gross K, et al. Pulmonary function and exercise response in patients with pectus excavatum after Nuss repair. J Pediatr Surg. 2003. 38:544–547.

9. Bawazir OA, Montgomery M, Harder J, Sigalet DL. Midterm evaluation of cardiopulmonary effects of closed repair for pectus excavatum. J Pediatr Surg. 2005. 40:863–867.

10. Coln E, Carrasco J, Coln D. Demonstrating relief of cardiac compression with the Nuss minimally invasive repair for pectus excavatum. J Pediatr Surg. 2006. 41:683–686.

11. Nakagawa Y, Uemura S, Nakaoka T, Yano T, Tanaka N. Evaluation of the Nuss procedure using pre-and postoperative computed tomographic index. J Pediatr Surg. 2008. 43:518–521.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download