Abstract
Purpose
Two Korean nationwide studies showed that metallo-β-lactamases (MBLs)-producing-Pseudomonas spp. are not rare. The aim of this study was to assess the trends of MBL-producing isolates among imipenem-resistant isolates of Pseudomonas spp.
Materials and Methods
Imipenem-resistant clinical isolates were collected from 23 hospitals and one commercial laboratory participating in the KONSAR program in 2005. Polymerase chain reaction (PCR) was used to detect MBL genes.
Pseudomonas aeruginosa is one of the most important nosocomial pathogens, while other Pseudomonas spp. are occasional causes of infections. Current isolates of P. aeruginosa are often multiresistant to many classes of potent antimicrobial agents, including β-lactams, aminoglycosides, and fluoroquinolones. Carbapenems are the most potent β-lactams, which are active even against extended-spectrum β-lactamase- and AmpC β-lactamase-producing gram-negative bacilli. Due to acquired metallo-β-lactamase (MBL) production, however, carbapenem resistance in P. aeruginosa and Pseudomonas spp., has increasingly been reported in some countries.1,2 Richet et al.3 initiated an international network and included carbapenemase-producing gram-negative bacilli in the early warning system list for emerging antimicrobial drug-resistant pathogens.
The Korean Nationwide Surveillance of Antimicrobial Resistance (KONSAR) program conducted in the years between 1998 and 2003 showed that P. aeruginosa ranked the 3rd by the number of isolates.4,5 The imipenem resistance rate of P. aeruginosa in 1999 was already relatively high (19%), but the rate rose further to reach 24% in 2004. Two previous studies with clinical isolates of P. aeruginosa, which were collected in 2000-2001 and in 2003 from hospitals participating in the program of KONSAR, showed that over 10% of all imipenem-resistant isolates were VIM-2 type MBL producers.6,7 Other studies also documented the presence of MBL-producing P. aeruginosa in Korean hospitals8,9 as well as the occasional presence of VIM-2-type MBL-producing isolates of Enterobacteriaceae.10,11 Moreover, the emergence of IMP-1-like-producing P. aeruginosa and finding of the fifth MBL, SIM-1-producing Acinetobacter baumannii isolates, were reported from a hospital in Seoul.12
The aim of this study was to determine any change in the prevalence of VIM-2- and IMP-1-like-producing clinical isolates of Pseudomonas spp. and possible emergence of new MBL variants two years after the second nationwide study. The possible presence of MBL-producing Enterobacteriaceae and spreading of blaSIM-1 type MBL gene to Pseudomonas spp. were also investigated.
Non-duplicate, imipenem-resistant strains of P. aeruginosa, Pseudomonas spp., and Enterobacteriaceae, isolated during January to August 2005, were collected from 23 hospitals and one commercial laboratory participating in the KONSAR program. The number of isolates collected from any one hospital was limited to 25 for an individual species. Identification of the species was reconfirmed at the coordinating laboratory through the use of a conventional method13,14 or the ATB 32GN system (bioMerieux, Marcy l'Etoile, France). The MICs of antimicrobial agents for MBL-producing isolates were determined by the NCCLS agar dilution method.15
Carbapenemase production was screened by the imipenem-disk Hodge (cloverleaf) test, using MacConkey agar instead of previously used Mueller-Hinton agar.16 MBL production was screened by the double-disk synergy test using an imipenem disk and an EDTA (750 µg) plus sodium mercaptoacetic acid (SMA, 2 mg) disk on Mueller-Hinton agar with 10 mm distance from the edge to the edge of the disk.16 Commercial imipenem disks and media (Becton-Dickinson, Sparks, MD, USA) were used for these tests, while the EDTA-SMA disks were prepared from commercially available chemicals (Sigma Chemical, St. Louis, MO, USA).
To detect alleles of blaIMP-1, blaVIM-2, and blaSIM-1, DDS-positive isolates were tested by PCR as described previously.12 Briefly, primers used were: IMP1-F 5'-CAT GGT TTG GTG GTT CTT GT-3' and IMP1-R 5'-ATA ATT TGG CGG ACT TTG GC-3'; VIM2-F 5'-ATG TTC AAA CTT TTG AGT AAG-3' and VIM2-R 5'-CTA CTC AAC GAC TGA GCG-3'; SIM1-F 5'-TAC AAG GGA TTC GGC ATC G-3' and SIM1-R 5'-TAA TGG CCT GTT CCC ATG TG-3'. PCR was performed with 1 µL of heat-extracted DNA template, 20 pmol of each primer, and PreMix (Bioneer, Cheongwon, Korea) containing 1 U of Taq DNA polymerase in a total volume of 20 µL. A Mastercycler instrument (Eppendorf, Hamburg, Germany) was used with the following reaction conditions: 94℃ for 5 min, 25 cycles of 94℃ for 30 s, 56℃ for 30 s, and 72℃ for 45 s, and finally, 72℃ for 7 min. Amplicons were visualized by electrophoresis and ethidium bromide staining.
For PFGE, χbaI-digested genomic DNA was prepared according to the instruction of Bio-Rad (Hercules, Calif., USA), and fragments were separated using a CHEF-DR II system (Bio-Rad). We selected 17 isolates which represented PFGE types and performed the sequencing of PCR amplicons using IMP1-F or VIM2-F and Int2 (5'-AAG CAG ACT TGA CCT GA-3'), and IMP1-R or VIM2-R and Int1 (5'-GGC ATC CAA GCA GCA AG-3').
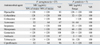
Among the 443 imipenem-resistant isolates collected, the majority were P. aeruginosa (93.7%), whereas 16 isolates were species of Enterobacteriaceae (9 K. pneumoniae, 2 each of E. aerogenes, E. coli, and P. mirabilis, and 1 C. freundii). Of these isolates, 127 were positive for the imipenem-disk Hodge test and 53 were positive for the DDS test (Table 1). Alleles of blaVIM-2 or blaIMP-1 were detected in all 53 DDS-positive isolates. Among all the isolates tested, the MBL-positive isolates comprised 10.8% of P. aeruginosa and 66.7% (8 of 12) of P. putida. MBL was not detected in any of the 16 isolates of Enterobacteriaceae.
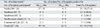
Overall, the proportion of blaVIM-2 allele-positive isolates was greater (73.6%) than blaIMP-1 allele-positive isolates (Table 1). blaSIM-1-allele-positive isolate was not detected. All MBL-producing isolates of Pseudomonas spp. other than P. aeruginosa were identified as P. fluorescens/P. putida by the ATB 32 GN system. However, they were confirmed to have biochemical characteristics of P. putida by conventional tests. Nucleotide sequencing revealed that all the blaVIM-2-like and blaIMP-1-like in P. aeruginosa were VIM-2 and IMP-6. MBLs in P. putida were identified as VIM-2 and IMP-1. We found 13 different PFGE patterns in 23 blaVIM-2-like Pseudomonas spp. and 4 patterns in 7 blaIMP-1-like Pseudomonas spp., indicating that multiple MBL-producing Pseudomonas clones exist in Korea. The MIC50s of various β-lactams for MBL-producing P. aeruginosa were equal to over 64 µg/mL except that of aztreonam (Table 2). The % resistances for aztreonam, piperacillin, amikacin, ciprofloxacin and other β-lactams were 67%, 83%, 87%, 96%, and 100%, respectively.
MBL-producing isolates were detected in 18 of 24 (75%) hospitals/laboratory, as well as in all four regions (Table 3). MBL-producing isolates were mostly derived from specimens of urine, sputum, and wounds (Table 4). All 8 MBL-producing P. putida isolates came either from urine or sputum. The MBL-producers were isolated mainly from inpatients (80: 63% isolates from general ward and 17% isolates from intensive-care unit); while 20% of isolates were from outpatient department.
Antimicrobial resistance surveillance has become increasingly important with the recent increase in the resistant organisms.17 Analysis of the data generated by the participating hospitals in 1998 and 2004 showed an alarming rise in the imipenem resistance rates of P. aeruginosa; from 19% to 24%.4,5 Decrease of carbapenem susceptible P. aeruginosa was also reported in Japan; from 80.7% to 62.0% over the period of 1998-2002.18
Among the β-lactamases, the genetically mobile MBL are among the most feared, because of their ability to hydrolyze virtually all β-lactams, except monobactams,19 and to spread horizontally. As a result of their geographic spread, these enzymes are among the greatest concerns to the medical communities.1,20 The rates of occurrence and number of enzyme types of MBL have escalated since 2000 in Asia, Europe, and Latin America.1,2,21 In the present study, 10.8% of imipenem-resistant-isolates of P. aeruginosa were MBL producers. These proportions were similar to those in the previous study in 2000-2001 and in 2003.6,7 The rate was also similar to that in a Japanese study in 1998-2002.18
In this study, only 12 imipenem-resistant isolates of Pseudomonas spp. other than P. aeruginosa were collected. It is of an interest to note that all 8 MBL-producing isolates were identified as P. putida. P. putida is a species difficult to differentiate from P. fluorescens by commonly used biochemical tests. Although P. putida is an only organism occasionally isolated from clinical specimens,13 the detection of MBL gene in 8 of 12 imipenem-resistant isolates suggests that this organism may play a significant role as an important reservoir of MBL genes.
Only 16 imipenem-resistant Enterobacteriaceae isolates could be collected in this study, and MBL was not detected in any of these isolates. This indicates rarity of Enterobacteriaceae isolates not only producing MBL, but also resistant to imipenem. MBL has been detected only in a few isolates of Enterobacteriaceae in Korea.11,13,22
It is interesting that the first acquired MBL discovered in the early 1990s was IMP-1 in nearby Japan,23 whereas in Korea, VIM-2 was the first MBL type detected and IMP-1 was detected in Acinetobacter spp. in the early 2000s.6 In a study at a hospital in Seoul, IMP-1-like-producing P. aeruginosa was detected in strains isolated in 2003-2004, but the number was only two of 76 isolates of Pseudomonas spp.12 In the present study, 14 of 53 MBL-producing isolates of P. aeruginosa and P. putida had blaIMP-1, indicating spread of this MBL gene to these species (Table 1). However, blaSIM-1 which was discovered in A. baumannii isolates in Seoul has not yet spread to Pseudomonas spp.
Detection of MBL-producing Pseudomonas spp. in isolates collected from 18 of 24 (75.0%) hospitals/laboratory in the present study (Table 3) is a great concern. As in previous studies,6,7 MBL-producing isolates were isolated mostly from urine and sputum specimens (Table 4), indicating that these specimens can serve as the important reservoirs for dissemination of the resistant organisms.
In conclusion, clinical isolates of P. aeruginosa in Korea are increasingly resistant to imipenem, and a significant proportion of the resistance is due to MBL production. blaVIM-2 remains the dominant type, however, IMP-1 variant, IMP-6-producing P. aeruginosa emerged. Extensive amount of effort is required to control further spread of MBL-producing Pseudomonas spp. in hospitals.
Namhee Ryoo, Keimyong University Dong San Medical Center, Daegu; Seok Hoon Jeong, Kosin University Gospel Hospital, Busan; Gyoung-Yim Ha, Dongguk University Kyongju Hospital, Gyeongju; Mi-Na Kim, University of Ulsan College of Medicine, Seoul; Wee-Gyo Lee, Ajou University Hospital, Suwon; Young-Ae Hong, Ulsan Dong-Kang General Hospital, Ulsan; Soung-Eun Cho, Ewha Womans University College of Medicine, Seoul; Young Uh, Yonsei University Wonju Christian Hospital, Wonju; Sook Jin Jang, Chosun University Hospital, Gwangju; Myung Hee Lee, Korea Veterans Hospital, Seoul; Wonkeun Song, Hallym University College of Medicine, Seoul; Tae Yeal Choi, Hanyang University Medical College, Seoul; Jong Hee Shin, Chonnam National University Hospital, Gwangju; Seong Geun Hong, Pochon CHA University Hopsital, Seongnam; Young Ah Kim, National Health Insurance Corporation Ilsan Hospital, Goyang; Dong Hee Cho, Samsung Cheil Hospital, Seoul; Dong Hee Whang, Inje University College of Medicine, Seoul; Seungok Lee, Seoul Clinical Laboratory, Seoul; Seonghee Lee, Hanmaeum Hospital, Jeju.
Figures and Tables
Table 1
Metallo-β-Lactamase Genes Detected in Imipenem-Resistant Isolates of Pseudomonas spp. and Enterobacteriaceae by PCR

ACKNOWLEDGEMENTS
We thank Dr. Jong Hwa Yum for his molecular laboratory work and Ms. Yong Hee Suh and Cha Soon Lee for technical assistance.
References
1. Nordmann P, Poirel L. Emerging carbapenemases in Gram-negative aerobes. Clin Microbiol Infect. 2002. 8:321–331.

2. Walsh TR, Toleman MA, Poirel L, Nordmann P. Metallo-beta-lactamases: the quiet before the storm? Clin Microbiol Rev. 2005. 18:306–325.
3. Richet HM, Mohammed J, McDonald LC, Jarvis WR. Building communication networks: international network for the study and prevention of emerging antimicrobial resistance. Emerg Infect Dis. 2001. 7:319–322.

4. Lee K, Kim YA, Park YJ, Lee HS, Kim MY, Kim EC, et al. Increasing prevalence of vancomycin-resistant enterococci, and cefoxitin-, imipenem- and fluoroquinolone-resistant gram-negative bacilli: a KONSAR study in 2002. Yonsei Med J. 2004. 45:598–608.
5. Lee K, Lim CH, Cho JH, Lee WG, Uh Y, Kim HJ, et al. High prevalence of ceftazidime-resistant Klebsiella pneumoniae and increase of imipenem-resistant Pseudomonas aeruginosa and Acinetobacter spp. in Korea: a KONSAR program in 2004. Yonsei Med J. 2006. 47:634–645.
6. Lee K, Lee WG, Uh Y, Ha GY, Cho J, Chong Y. Korean Nationwide Surveillance of Antimicrobial Resistance Group. VIM- and IMP-type metallo-beta-lactamase-producing Pseudomonas spp and Acinetobacter spp in Korean hospitals. Emerg Infect Dis. 2003. 9:868–871.

7. Lee K, Ha GY, Shin BM, Kim JJ, Kang JO, Jang SJ, et al. Metallo-beta-lactamase-producing Gram-negative bacilli in Korean Nationwide Surveillance of Antimicrobial Resistance group hospitals in 2003: continued prevalence of VIM-producing Pseudomonas spp. and increase of IMP-producing Acinetobacter spp. Diagn Microbiol Infect Dis. 2004. 50:51–58.

8. Oh EJ, Lee S, Park YJ, Park JJ, Park K, Kim SI, et al. Prevalence of metallo-beta-lactamase among Pseudomonas aeruginosa and Acinetobacter baumannii in a Korean university hospital and comparison of screening methods for detecting metallo-beta-lactamase. J Microbiol Methods. 2003. 54:411–418.

9. Kim IS, Lee NY, Ki CS, Oh WS, Peck KR, Song JH. Increasing prevalence of imipenem-resistant Pseudomonas aeruginosa and molecular typing of metallo-beta-lactamase producers in a Korean hospital. Microb Drug Resist. 2005. 11:355–359.

10. Jeong SH, Lee K, Chong Y, Yum JH, Lee SH, Choi HJ, et al. Characterization of a new integron containing VIM-2, a metallo-beta-lactamase gene cassette, in a clinical isolate of Enterobacter cloacae. J Antimicrob Chemother. 2003. 51:397–400.

11. Lee HK, Park YJ, Kim JY, Chang E, Cho SG, Chae HS, et al. Prevalence of decreased susceptibility to carbapenems among Serratia marcescens, Enterobacter cloacae, and Citrobacter freundii and investigation of carbapenemases. Diagn Microbiol Infect Dis. 2005. 52:331–336.

12. Lee K, Yum JH, Yong D, Lee HM, Kim HD, Docquier JD, et al. Novel acquired metallo-beta-lactamase gene, bla(SIM-1), in a class 1 integron from Acinetobacter baumannii clinical isolates from Korea. Antimicrob Agents Chemother. 2005. 49:4485–4491.

13. Kiska DL, Gilligan PH. Murray PR, Baron EJ, Jorgen Sen JH, Pfaller MA, Yolken RH, editors. Pseudomonas. Manual of Clinical Microbiology. 2003. 8th ed. Washington DC: American Society of Microbiology;719–728.
14. Farmer JJ III. Murray PR, Baron EJ, Jorgensen JH, Pfaller MA, Yolken RH, editors. Enterobacteriaceae: introduction and identification. Manual of Clinical Microbiology. 2003. 8th ed. Washington DC: American Society of Microbiology;636–653.
15. National Committee for Clinical Laboratory Standards. M100-S14. Performance standards for antimicrobial susceptibility testing; Fourteenth informational supplement. 2004. Wayne, PA: NCCLS.
16. Lee K, Lim YS, Yong D, Yum JH, Chong Y. Evaluation of the Hodge test and the imipenem-EDTA double-disk synergy test for differentiating metallo-beta-lactamase-producing isolates of Pseudomonas spp. and Acinetobacter spp. J Clin Microbiol. 2003. 41:4623–4629.

17. Cornaglia G, Hryniewicz W, Jarlier V, Kahlmeter G, Mittermayer H, Stratchounski L, et al. European recommendations for antimicrobial resistance surveillance. Clin Microbiol Infect. 2004. 10:349–383.

18. Jones RN, Deshpande LM, Bell JM, Turnidge JD, Kohno S, Hirakata Y, et al. Evaluation of the contemporary occurrence rates of metallo-beta-lactamases in multidrug-resistant Gram-negative bacilli in Japan: report from the SENTRY Antimicrobial Surveillance Program (1998-2002). Diagn Microbiol Infect Dis. 2004. 49:289–294.

19. Bush K. Metallo-beta-lactamases: a class apart. Clin Infect Dis. 1998. 27:S48–S53.
20. Livermore DM, Woodford N. Carbapenemases: a problem in waiting? Curr Opin Microbiol. 2000. 3:489–495.

21. Jones RN, Biedenbach DJ, Sader HS, Fritsche TR, Toleman MA, Walsh TR. Emerging epidemic of metallo-beta-lactamase-mediated resistances. Diagn Microbiol Infect Dis. 2005. 51:77–84.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download