Abstract
Colorectal cancers (CRC)-and probably all cancers-are caused by alterations in genes. This includes activation of oncogenes and inactivation of tumor suppressor genes (TSGs). There are many ways to achieve these alterations. Oncogenes are frequently activated by point mutation, gene amplification, or changes in the promoter (typically caused by chromosomal rearrangements). TSGs are typically inactivated by mutation, deletion, or promoter methylation, which silences gene expression. About 15% of CRC is associated with loss of the DNA mismatch repair system, and the resulting CRCs have a unique phenotype that is called microsatellite instability, or MSI. This paper reviews the types of genetic alterations that can be found in CRCs and hepatocellular carcinoma (HCC), and focuses upon the epigenetic alterations that result in promoter methylation and the CpG island methylator phenotype (CIMP). The challenge facing CRC research and clinical care at this time is to deal with the heterogeneity and complexity of these genetic and epigenetic alterations, and to use this information to direct rational prevention and treatment strategies.
Cancers are caused by alterations in genes. However, there are many different types or classes of alterations and diverse genetic targets that can be found in cancers. This review is focused on the genetic, and epigenetic, alterations associated with colorectal cancer (CRC).
It must be understood at the outset that there is not a single mechanism for carcinogenesis that is common to all CRCs. There are at least three general patterns that can be found, and there is a complex interaction among these, in which one type of genetic signature is a consequence of one or another of the other two. Furthermore, some of these diverse changes can be found in any CRC, at least to some degree. Typically, one type of genomic instability predominates, and creates a principal "genetic signature" in most CRCs. These signatures provide insight into how that tumor developed, and may provide roadmaps in the future from which prevention and treatment strategies may be developed.
Three different genetic signatures are characteristically seen in CRC; to be precise, two of these are truly genetic, and the third is more properly considered epigenetic.
The first of these, chromosomal instability or CIN, is a process that creates genetic deletions, duplications and chromosomal rearrangements in the nucleus of a tumor cell. This is manifested as aneuploidy, which is readily recognized using cytogenetic techniques (and even the light microscope), and is commonly present in all types of cancer. Chromosomal rearrangements that put growth-supporting genes under the control of an inappropriately active gene promoter are commonly seen in many types of leukemias and lymphomas. However, this has not been found to be a prominent mechanism in CRC. At least 50% of CRCs have a prominent CIN phenotype1,2, and some have speculated that all CRCs have some degree of this, if one examines the chromosomes carefully.3 There is no accepted mechanism that explains CIN or aneuploidy in a generalized way for all cancers, but mutations or abnormal expression of multiple different genes have been proposed to explain this.4-8 The basis of CIN remains an open question, and a fundamental one for the understanding of all cancer.
A second type of genetic signature is microsatellites instability, or MSI, which is a "mutator phenotype" that occurs in about 15% of CRC. Interestingly, most CRCs with MSI are apparently diploid or near-diploid.9 MSI is the consequence of inactivation of the DNA mismatch repair (MMR) system, and is characterized by very frequent mutations at simple repeat sequences (microsatellites). In this case, the predominant outcome is inactivation of tumor suppressor genes that have microsatellite sequences (typically a mononucleotide that is repeated 7-10 times) that are strategically located in the gene. The characteristic signature of MSI is the deletion of one element in the repetitive sequence, which creates a frameshift in the coding sequence, inactivating gene expression.
Such critically-located microsatellite sequences are relatively uncommon in human genes, but a few human genes encoding microsatellites happen to be critical in the control of epithelial cell growth.10 Examples of these genes are the transforming growth factor beta-1 receptor II gene, which encodes a sensitive A10 sequence in exon 3,11 and the BAX gene,12 which encodes a G8 sequence, just to name two. This phenotype is always caused by loss of the DNA mismatch repair system, and is seen either in association with germline mutations in the DNA MMR genes (Lynch Syndrome), or the acquired methylation-induced silencing of the MLH1 gene.13
Promoter methylation results in gene silencing, a process that normally accompanies aging. However, substantial increases in the amount of methylation can be found in certain CRCs which can lead to the silencing of certain tumor suppressor genes. It is less certain whether different genes are more likely to be affected when methylation is seen in cancers. In any event, when it occurs in tumor DNA, the phenotype is called the CpG Island methylator phenotype (CIMP).14 About half of the promoters of human genes are embedded in CpG islands, and are susceptible to methylation-induced silencing, but certain genes are more frequently affected than others. CpG islands typically encompass 1-2 kb of the promoter regions, but can also extend to 5'-untranslated regions within the first exon of certain tumor suppressor genes.15 CIMP is also referred to as an 'epigenetic' phenomenon since this does not involve a permanent change (a 'genetic event' such as a point mutation or deletion) in the target DNA sequence, but simply reflects a potentially reversible alteration due to methylation of the cytosine nucleotides that occur in context of CpG dinucleotide. The mechanism responsible for CIMP is unknown. Although most investigators in the field accept the concept that there is a "methylator phenotype", there is a minority opinion on the subject that is not so sure.16
The discovery of CIMP is an interesting example of serendipity and opportunities taken in biological research. The first evidence of a CIMP-like phenomenon was made in 1997, when a group of investigators was investigating aberrant methylation of several tumor suppressor genes including p16, TSP-1 and IGF2 in sporadic CRCs. They observed that CRCs with MSI were more frequently hypermethylated compared to microsatellite stable (MSS) tumors.17 In this study, more than 60% of sporadic MSI CRCs showed concordant methylation of ≥ 2 loci compared with MSS cancers.17 The same group subsequently proposed a panel of 7 methylation loci, or markers, that were frequently methylated in tumors, and referred to them as MINT clones: MINT 1, 2, 12, 17, 25, 27, and 31.14 However, the biological relevance of methylation at these loci and the general importance of CIMP were not fully appreciated until it was recognized that methylation at the MINT clones was associated with the transcriptional silencing of the DNA MMR gene MLH1, a mechanism that is the cause of the majority of sporadic MSI CRCs.18
In an effort to classify subsets of sporadic CRCs, Issa and colleagues then proposed that concordant methylation of these methylation loci in colonic tumors may be defined as CIMP, and suggested that this reflected a unique epigenetic pathway in colorectal carcinogenesis.14 In this context, a recent study has proposed a newer set of CIMP markers that is different from the original panel, but show comparable specificity for identifying CRCs with a methylator phenotype.19
Following the initial description of CIMP in sporadic CRC, the next several years witnessed independent efforts to determine whether the CIMP markers were adequate for the reproducible identification of a unique group of tumors. Some investigators proposed that promoter hypermethylation might be present in all aging tissues, and to some degree, in all CRCs. The discoverers of CIMP suggested that methylation occurred in a bimodal distribution in CRC, and proposed that CIMP-associated neoplasms would have unique biological or clinical features. The majority of studies have favored existence of CIMP as a unique carcinogenic pathway. However, a handful of studies have raised the contrary opinion that CIMP in CRC may not be the distinct mechanism of epigenetic instability that was initially proposed.16,20 However, the weight of the accumulating evidence suggests that CIMP represents a unique pathway and phenotype in CRC.21-23
However, there is not yet a consensus on what markers and criteria should be used to define CIMP in CRC. This is essentially because of the absence for a standardized panel of CIMP-markers, use of different methylation assays, and non-uniform thresholds for methylation among various studies.
During the past decade, while other laboratories were involved in defining CIMP, we became interested in understanding the relationship between various forms of genomic instability in CRC. We proposed the hypothesis that some form of genomic instability would be present in every CRC, and that every CRC could be categorized based upon the mutational (or epigenetic) signature present in the DNA of the tumor. We began by characterizing 209 stage II or III CRC for either CIN (looking for loss of heterozygosity or LOH at loci on 1p, 2p, 3p, 5q, 17p or 18q) or MSI (using a National Cancer Institute recommended panel of markers). In this study, 14% of CRC showed MSI (specifically, MSI-high), and 51% had LOH at 1 or more loci (Fig. 1A). Of the 107 cancers with at least one LOH event, only 6.5% were MSI, indicating some degree of overlap, at least with these LOH markers. The most unexpected and provocative finding was that 38% of the non-MSI tumors had no LOH.2 This led to the hypothesis that another type of genetic or nuclear abnormality was operative in CRC. We proposed that the unidentified abnormality might be CIMP.
Therefore, we next examined 126 sporadic CRCs, and categorized them as having MSI, LOH, or neither using 6 markers previously linked to CIMP, and 6 new putative methylation loci linked to likely tumor suppressor genes (TSGs). As shown in Fig. 1B, we found that there was a significant degree of methylation at the previously-identified CIMP-associated loci (MINT-1, -2, -31, p16, p14, MLH1), as well as in our 6 new TSG markers (PTEN, TIMP3, RUNX3, HIC1, APC, and RARβ2). We also tested for a mutation in the BRAF gene that had been linked with CIMP, as defined by the traditional CIMP-associated markers. BRAF V600E mutations were associated with MSI, and with the non-MSI/non-LOH CRCs. There was a significant inverse relationship between frequencies of LOH and the degree of methylation in CRC (p < 0.0001; Fig. 1C). We recognized that most of the non-MSI/non-LOH CRCs were associated with CIMP, suggesting that these are two independent pathways for tumor development. Furthermore, most of the MSI tumors were associated with CIMP, and methylation of the DNA MMR gene, MLH1.22 The exceptions to this are CRCs associated with Lynch Syndrome, which is caused by germline mutations in a DNA MMR gene, accompanied by loss of the wild type allele, often through an LOH event. Thus, CRCs with MSI are either caused by CIMP and methylation of the MLH1 gene, or they are found in patients Lynch Syndrome. With this in mind, one can consider MSI to be a consequence of either CIMP or Lynch syndrome plus the loss of the wild type copy of the DNA MMR gene with the germline mutation. In the latter situation, the loss of the wild type allele could be due to an LOH event, which would explain the apparent overlap between MSI and CIN. Current evidence supports a role for either LOH24 or methylation25 as the mechanism for the second hit in Lynch syndrome.
The MGMT gene is a DNA repair gene generally involved in the removal of mutation-inducing DNA adducts, and is specifically responsible for removing O6-methylguanine residues which are formed by the acquired (and presumably accidental) methylation of guanine residues. Persistence of these adducts give rise to G : C to A : T mutations, which are common mutations found in two of the most important genes altered in CRC : KRAS and p53.26 Mutational inactivation of MGMT is rare, and does not play a prominent role in CRC. Interestingly, the MGMT promoter has two CpG clusters that are sensitive to methylation. One, termed the Mp region, is upstream of exon 1 and includes the minimal promoter. The second, termed the Eh region, is downstream of Mp, and contains several enhancer elements that are involved in the regulation of gene expression. We examined DNA from 233 CRCs, 104 adenomatous polyps (APs) and 220 normal colonic tissues for evidence of methylation at the Mp and Eh regions of MGMT. We found that methylation was extensive in the CRCs, there was partial methylation in the APs, and there was significantly less methylation in the normal colonic tissues. Additionally, there was less methylation in the normal colonic tissues from patients who did not have CRC compared with those that did. We found a significant correlation between extensive methylation (which was seen principally in the CRCs) and reduced or absent expression of the MGMT protein. Another important observation was made in these experiments; MGMT methylation was significantly associated with G:A mutations in the KRAS gene. Thus, methylation was quantitatively more involved in the more advanced neoplastic lesions, was associated with gradual loss of protein expression, and was linked to activating mutations in the RAS-RAF signaling pathway. These findings suggest the interpretation that methylation-induced silencing of the MGMT gene occurs in a gradual or step-wise manner, and is quantitatively correlated with progressive multistep carcinogenesis in the colon.27
KRAS and BRAF are signal transduction proto-oncogenes involved in the regulation of cell growth and proliferation. These two proteins participate in the same serial signaling pathway that begins with the epidermal growth factor receptor (EGFr) on the plasma membrane of the intestinal epithelial cell, and eventually triggers the proliferation program in the nucleus. Activating KRAS and BRAF mutations are commonly found in CRCs, but the two mutations rarely are found in the same tumor, as there would be little added fitness or growth advantage for having both. KRAS was the first oncogene in which activating mutations were found in CRC, and these occur in about half of all CRCs.28,29 Activating mutations in BRAF were later found to be common in cancer,30 and the V600E mutation was linked with CIMP in CRC.19 Although the mechanism linking BRAF mutation and CIMP remains elusive, it has been suggested that finding mutations in either KRAS or BRAF may be important for our understanding of the pathogenesis and clinical behavior of tumors that have one or the other of these.
Therefore, we used 14 methylation markers (7 classic CIMP markers, and 7 additional TSG loci) to evaluate the promoter methylation status of 487 colorectal specimens, including 243 CRCs and their corresponding normal mucosa, and 36 samples of colonic tissue obtained from individuals without colorectal neoplasia at colonoscopy. The CRC group included 21 samples from patients with Lynch syndrome, and another 15 cases of sporadic MSI (caused by hypermethylation of the MLH1 gene). We then correlated the methylation data with mutations in KRAS and BRAF.
First, we found relatively little methylation in the normal colonic tissues, whether they came from CRC patients or those without colorectal neoplasia. We then found that aberrant methylation of the 7 canonical CIMP markers was highest (mean 3.6 of 7) in BRAF-mutated CRCs compared with KRAS-mutated CRCs (mean 1.2; p < 0.001), or CRCs with wild type KRAS and BRAF genes (0.7, p < 0.0001; Fig. 2A). By contrast, analysis of the 7 non-canonical CIMP markers showed different associations. These novel markers were associated with the same number of aberrantly methylated loci in either BRAF or KRAS-mutated CRCs (4.4 and 4.3 respectively). CRCs with sporadic MSI had significantly more methylation (8.4 markers of all 14), but the Lynch syndrome CRCs had slightly more methylation than the non-MSI tumors. Additionally, we found only BRAF (but never KRAS) mutations in the sporadic MSI CRCs, and only KRAS (but never BRAF) mutations in the Lynch syndrome tumors. BRAF mutations were found in 10/15 of the sporadic MSI tumors, making it a reliable marker for excluding the diagnosis of Lynch syndrome in an ambiguous situation of an MSI CRC with absence of MLH1 expression. In a general way, the associations between CIMP and KRAS/BRAF mutations in CRCs with MSI are dependent upon the marker panel used. The canonical CIMP markers associate best with sporadic MSI and the V600E mutation in BRAF.31
Lynch syndrome, sometimes called hereditary non-polyposis colorectal cancer (HNPCC), is an autosomal dominant inherited disease, which is caused by germline mutations in DNA MMR genes, most often MLH1 and MSH2. Mutations in MMR genes cause MMR-deficiency that results in MSI, a mutational signature present in more than 90% of Lynch syndrome cancers.32 Although Lynch syndrome tumors harbor germline mutation in one allele of the involved MMR gene, a second inactivating event is imperative for the loss of MMR activity in these cancers. The somatic inactivation of the remaining wild-type allele (or 'second hit') could be a genetic change such a somatic mutation or LOH event,33 or alternatively an epigenetic alteration asso-ciated with hypermethylation of the promoter.34 Although somatic mutations and deletions in MMR genes have been described in these tumors,24,35 none of the previous studies have reported conclusive evidence for the role of aberrant methylation in Lynch syndrome cancers.24
We addressed this question in a recent study in which we determined methylation frequencies in a series of 21 Lynch syndrome subjects and compared this with sporadic MSS and MSI CRCs, using a panel of 14 methylation makers comprised of 7 CIMP-canonical markers and 7 additional loci.31 We further correlated methylation profiles with the presence of BRAF and KRAS mutations in these tumors. Not surprisingly, we found that the mean methylation was highest for each of the 14 methylation markers in sporadic MSI CRCs (Fig. 2B). Interestingly however, we also observed frequent aberrant methylation in Lynch syndrome tumors. The average methylation in Lynch syndrome CRCs was consistently higher than in non-MSI tumors, regardless of whether we analyzed all 14 markers (average 5.1 vs. 4.5 in MSI-L and 4.4 in MSS) or used only the 7 canonical CIMP markers (average 1.5 vs. 1.0 in MSI-L and 0.89 in MSS). Additionally, we did not find V600E BRAF mutations in any Lynch syndrome cancer, but one third of these tumors showed KRAS mutations. These findings indicate that CIMP in CRC is associated with activating mutations in either BRAF or KRAS, and that aberrant DNA methylation is a common event, not only in sporadic CRC, but also in Lynch syndrome CRCs.31 In this scenario, aberrant methylation of a DNA MMR gene may provide the 'second hit' necessary to inactivate the wild-type allele in some proportion of Lynch syndrome patients.
Although CIMP was historically discovered in the colon and is probably best investigated in this organ, the existence of this unique phenotype is not confined to CRC, and has also been identified in several other malignancies including gastric cancer,36 leukemia37 and hepatocellular carcinoma.38
As mentioned, the mechanism responsible for promoter methylation is unknown, which limits our understanding of how the process occurs, and inhibits the development of strategies to prevent or modify this process. To test the potential role of virally-induced inflammation in CIMP, we studied a cohort of 81 HCCs and 77 non-cancerous liver tissues, because of the well-documented role of chronic viral infections in these tumors. First, we analyzed the tumors for CIN and for mutations in a number of potential oncogenes. CIN was determined using 400 microsatellite markers in the 81 HCCs, looking for allelic imbalance compared with the normal, non-neoplastic liver (available in 77 of these). We also analyzed for methylation abnormalities, using 21 promoters, and quantitated the degree of methylation using combined bisulfite restriction analysis (called COBRA).
First, we found that methylation was significantly higher in the HCCs than in the matched normal liver for 18 of the 21 methylation loci (p values ranged from 0.035 to < 0.0001; Fig. 3). Using quantitative methylation data, we correlated CIMP with the mutational studies, which segregated the tumors into two groups by hierarchical clustering. One group was characterized by mutations in the p53 gene, and these tumors had significantly higher degrees of CIN (as measured by "fractional allelic loss", or FAL scores), and lower levels of methylation. The other group was characterized by mutations in the beta-catenin gene and significantly higher levels of methylation. Thus, HCCs were similar to CRCs, in that the tumors could be placed into two separate groups: CIN or CIMP. The first type is associated with p53 mutations, and the second with beta-catenin.39
We used a supplemented cohort to correlate CIMP in HCC with age and chronic infection with viral hepatitis. We used our matched pairs of HCC/normal liver, and added to this, 22 samples of normal liver tissue removed from patients who had undergone resections for metastatic CRC. For this study, we had 15 HCCs from patients who had documented infections with hepatitis B, 46 who had been chronically infected with hepatitis C, and 18 who had no evidence for infection with either virus. We used a variety of statistical analyses to determine associations between viral infection and methylation at 19 target loci (see the primary manuscript for the details40).
Analysis of methylation segregated the target loci into three groups. Normal tissues from patients who did not have HCC showed methylation at seven "group 1" loci, which included HIC-1, CASP8, GSTP1, SOCS1, RASSFIA, p16, and APC. Group 1 loci were more highly methylated than five markers in "group 2" (CDH1, RUNX3, RIZ1, SFRP2, and MINT31) or seven "group 3" (COX2, MINT1, CACNA1G, RASSF2, MINT2, Reprimo, and DCC). The non-cancerous hepatic tissue from patients with HCCs showed significant increases in methylation at group 1 and 2 loci. Finally, methylation was significantly greater in the HCC tissues in each of the loci from all 3 groups, where the methylation was both more frequent, and denser.
Methylation at the group 1 loci was significantly associated with increasing patient age, and quantitatively, methylation levels at all but one of the group 1 loci was significantly higher in patients ≥ 65 years old compared with those younger than 65. This observation underscores the role of aging and methylation at TSGs in the development of HCC. Interestingly, methylation in the non-neoplastic liver was significantly elevated at group 1 and 2 loci in the patients chronically infected with hepatitis C (compared to non-neoplastic liver from hepatitis B patients). In the HCC tissues, although methylation was extensive at the group 1 loci regardless of the associated viral infection, chronic hepatitis C infection was associated with higher levels of methylation at group 2 and 3 loci compared with the virus-negative HCCs.
Finally, we calculated the difference in methylation at each locus in the non-cancerous liver and HCC for each patient. Using hierarchical clustering analysis, we could categorize HCCs into two groups. Group B HCC patients (n = 36) had significantly more methylation than group A HCC patients (n = 39). Among the group B patients, 81% had chronic hepatitis C infections, 14% were positive for hepatitis B, and 5% (only 2) had neither virus; fully 94% had evidence for chronic viral hepatitis. However, in group A patients, 38% had hepatitis C, 21% had hepatitis B infections, and 41% were virus-negative (p = 0.0002 by χ2 analysis). All of these results support the hypothesis that chronic viral hepatitis infection, and prominently hepatitis C, may cause the methylator phenotype that is seen in HCC as summarized in Table 1.
Since the initial discovery almost two decades ago that the pRb gene can be a target of aberrant hypermethylation,41 it has been appreciated subsequently that aberrant methylation has consequences for transcriptional silencing of many cancer-related genes.42,43 However, the molecular mechanisms underlying the initiation and maintenance of aberrant methylation are unclear. In this regard, dietary and lifestyle factors have been proposed to influence aberrant methylation of tumor suppressor genes in different individuals.44 An association between cigarette smoking and CIMP has been described in a large cohort study.45 Similarly, It is believed that chronic exposures to yet other 'epi-mutagens' may provide a favorable environment for epigenetic modification of genomes in susceptible individuals. There are data to suggest that Helicobacter pylori (H. Pylori) infection closely correlates with aberrant methylation in gastric cancer.46,47 The precise mechanisms by which H. pylori may regulate aberrant hypermethylation in gastric cancer are still unclear, but reversal of hypermethylation following eradication of this organism from the stomach has resulted in demethylation of previously methylated genes.48,49 Along similar lines, viruses have also been etiologically linked to human cancers, and recent estimates suggest that as many as 15% of all cancers worldwide may be associated with chronic viral infections. We and others have provided provocative data to suggest that chronic exposure to viruses may be related to aberrant methylation of genes in several malignancies including colon cancer,50 hepatocellular carcinoma, 40,51 and gastric cancer.52
A body of literature suggests that adult cancers are derived from stem cells or early progenitor cells. Data gathered in recent years also indicate that aberrant methylation of genes is not a completely independent event, but acts in concert with epigenetic modifications that occur at the histone complexes within nucleosomes. The promoter chromatin state for the most hypermethylated genes in adult cancers is virtually identical between embryonic stem cells and adult cancer cells.53 In embryonic stem cells, these genes are held in a 'transcriptionally ready' status which is mediated by a bivalent promoter chromatin pattern that consists of a repressive mark (histone H3 methylation at Lys 27; H3K27) and an active mark (histone 3 dimethylation at Lys 4; H3K4), regulated by the polycomb group proteins (PcG).54 During conditions of abnormal cell renewal, such as cell stress, inflammation or chronic injury and repair, PcG complexes recruit additional repressive marks (H3K27me3 and H3K9me2) to these gene promoters, thus establishing an abnormal DNA methylation pattern, and the resultant silencing of specific growth regulatory genes. The loss of function of these critical genes in turn locks these aberrantly methylated stem cells in a state of abnormal clonal expansion that begins a process of neoplastic initiation and transformation.53,54 It is just a matter of time before we gain sufficient understanding of these events, which will eventually allow us to assemble the puzzle of the dynamics of aberrant DNA methylation in human cancer.
The identification of specific methylation events occurring early in multistep carcinogenesis and the suggestion that epigenetic silencing of genes plays a causative role in tumor development, have generated significant interest in the use of DNA methylation as a diagnostic marker of CRC. Multiple studies have indicated that aberrantly regulated DNA methylation is one of the key mechanisms for tumor suppressor gene silencing during the adenoma-to-carcinoma and serrated adenoma-to-carcinoma sequence in the colon. The aberrant methylation of certain tumor suppressor genes, such as p16, has been reported in colonic adenomas and aberrant crypt foci.55,56 To explore this, we investigated aberrant methylation of MGMT in a series of CRCs, adenomatous polyps and normal colonic mucosa specimens. We found a gradual increase in MGMT hypermethylation in a normal-to-adenoma-to-carcinoma progression, suggesting that methylation at this DNA repair gene may evolve and spread throughout the promoter in a gradual manner as the colonic epithelial cells move through the progressive, multistep cascade.27 In another study, we asked whether loss of one Netrin-1 receptor, UNC5C, were mediated via epigenetic silencing of its promoter region in the colon.57 We analyzed a group of 147 CRCs, 52 adenomas and 21 normal mucosal tissues. Interestingly, we found only rare evidence of UNC5C methylation in the normal colon, but an increased frequency of methylation in adenomas (63%) and CRCs (76%). When these data were compared with allelic losses at a second Netrin-1 receptor, DCC, we found that UNC5C methylation occurred predominantly in the earlier lesions (adenomas and early stage CRCs), whereas DCC losses occurred frequently in advanced CRCs. These data clarified the importance of epigenetic silencing as an earlier event (UNC5C methylation), compared to genetic alterations (DCC loss) that happen at later stages in multistep colorectal carcinogenesis.57 Another interesting feature is that these hypermethylated genes are not only pathogenic events in the adenoma-to-cancer progression, but are neoplasm-specific molecular events that have the potential to be used as molecular biomarkers of pre-malignant tumors in the colon.
In fact, novel approaches to the early detection of CRC that are possibly less expensive and might be better accepted by patients are being compared to the most commonly used screening methods. Pilot studies have shown promise for an approach using tumor-derived DNA mutations in the feces of cancer patients for the early detection of CRC. However, the use of assays based on methylated genes for the detection of colon polyps has not been as well studied to date.58-60 There is evidence to suggest that epigenetic signatures can be detected in the blood61 and stools61,62 of patients with colon polyps and cancer.
Promoter methylation analysis may also provide useful prognostic markers of disease progression and response to therapy. Specific methylation events have been associated with different tumor stages and with worse prognoses.63 Epigenetic changes are also under investigation as potential predictors of response to traditional chemotherapy.64 Unlike genetic events (mutations and allelic losses) that occur at tumor suppressor genes, epigenetic modifications are potentially reversible. The reversibility of DNA methylation has led to the development of novel therapies based on restoring the activity of methylation-silenced genes by inhibiting DNA methylation. At present, the most widely investigated inhibitors of methylation are the nucleoside analogs, 5-azacytidine (which has the commercial name, Vidaza), and 5-aza-2'-deoxycytidine (5-AZA, with the commercial name Decitabine), which are incorporated into DNA and prevent the activity of DNA methyltransferases (DNMTs).65
Aberrant methylation of genes may be important for chemosensitivity to various drugs currently used to treat cancer. Because multiple genes become methylated in individual cancers, many epigenetic targets can be affected by a single demethylating drug. Furthermore, the chemotherapeutic effect might be predictable prior to the administration of such drugs through an analysis of hypermethylated genes in a patient's tumor. The expression of a methylation-silenced tumor suppressor gene can be restored by treatment with a demethylating agent. Thus, even if a tumor has become resistant to anticancer drugs, this might be reversed, making the drugs effective at the usual therapeutic concentrations. As mentioned previously, 12% of sporadic CRCs show MSI due to MLH1 hypermethylation, and these tumors are typically resistant to various chemotherapeutic agents, including 5-fluorouracil (5-FU). Using an in vitro cell culture model, we tested the hypothesis that demethylation of the MLH1 promoter in hypermethylated colon cancer cells would restore MMR proficiency and sensitivity to 5-FU.66 We studied a panel of MMR-deficient CRC cell lines including SW48 (methylated at MLH1), HCT116, HCT116 + chr2 (both mutated at MLH1) and the MMR-proficient cell line HCT116 + chr3, in which the MLH1 gene was reconstituted by the stable transfer of chromosome 3 (Fig. 4A). We observed that 5-AZA treatment resulted in the demethylation of MLH1, and restored both mRNA and protein expression of the gene in SW48 cells. As demonstrated in the figure, 5-FU treatment strongly reduced the cell growth (as measured by colony formation activity) only in MMR-proficient HCT116 + chr3 cells, but was significantly less effective in all MMR-deficient cell lines.
Combined treatment of SW48 cells with 5-AZA and 5-FU resulted in the same growth inhibition as seen in 5-FU treated HCT116 + chr3 cells (Fig. 4B). These data clearly demonstrate that resistance to 5-FU can be overcome by reexpression of MLH1 protein through 5-AZA-induced demethylation. These findings could have a significant impact on the development of future chemotherapy strategies.66
One of the key limitations of these nucleoside analogs is that they do not act in a gene-specific manner; they cause global hypomethylation of all genes with CpG sequences. Nonetheless, these agents have progressed into clinical trials of several human cancers.67 To date the treatment outcome appears to be better in hematopoietic cancers than solid tumors.68 The toxicity of nucleoside analogs due to non-specific hypomethylation of potential proto-oncogenes and retrotranspoons has necessitated the development of other direct or indirect inhibitors of DNMT activity, including procainamide, green tea polyphenol, epigallocatechin-3-gallate (EGCG), and antisense oligodeoxynucleotides.69 These compounds are less potent inhibitors of DNMT activity compared to 5-AZA-based compounds, but offer less toxicity, and potentially can be used as an adjunct to nucleoside analog therapy.
JCV is a polyomavirus that infects most humans, and usually is associated with no apparent disease. However, JCV encodes a viral oncogene that induces cancer in two different animal models.70-72 We have reported that most CRCs harbor JCV DNA, and that over half of these express the viral transforming protein, T-antigen (T-Ag).73,74 JCV DNA and protein expression can be found in adenomatous polyps of the colon as well.75 This has been reproduced and supported by several other laboratories.76-78 Although nearly 90% of CRC tissues harbor JCV DNA, we have found a significant relationship between the expres-sion of T-Ag protein in the CRC nuclei and both CIN and CIMP (Fig. 5).50 It has been suggested by others previously that the methylator phenotype might be a cellular strategy to escape viral infection, and we are pursuing this hypothesis at present.
Moreover, transfection of the JCV genome into the CRC cell line RKO, which is near-diploid, induces CIN and aneuploidy.79 This is not an unexpected result, as the simian relative of JCV, SV40, regularly transforms cells in the laboratory, in association with the induction of an aneuploid phenotype. It remains to be proven whether JCV can induce CIMP in a controlled laboratory setting, but this result would add to the speculation that this common human virus might play a role in inducing all of the "forms" of CRC. If the mechanisms responsible for the generation of CIN and CIMP were known, it would facilitate thinking about rational strategies required to delay or prevent the development of colorectal neoplasia.
In summary, there is convincing evidence that aberrant methylation plays a pivotal role in human carcinogenesis. It is becoming increasing clear that a distinct methylator phenotype exists in the colon, and that as many as half of all sporadic CRCs may evolve through a pathway involving transcriptional silencing of several tumor suppressor genes. Additionally, it would appear that CIMP and CIN constitute the two major mechanisms of genomic instability in the colon, and that sporadic MSI tumors represent a subset of tumors with hypermethylation of the MLH1 gene. Although defining CIMP tumors is still a challenge, it is hoped that efforts in the near future will resolve this issue and allow the development of a uniform strategy to identify these tumors. Although future studies are necessary to validate the role of JCV in gastrointestinal carcinogenesis, it is likely that JCV may be an answer to the elusive questions about the molecular mechanisms responsible for CIMP and CIN. Although it may seem that our current understanding of CIMP is plagued with more questions than the answers, there is no doubt that future studies hold the promise to elucidate the terra incognita of CIMP in CRC.
Figures and Tables
Fig. 1
The relationships among various forms of genomic instability in CRC. (A) The pie chart illustrates the characterization of 209 sporadic CRCs for MSI and CIN.2 As shown, 48% of tumors had evidence of LOH, while 14% of tumors had MSI, including a minority of tumors (3%) that overlapped with LOH. We were most interested in the observation that nearly one third of the tumors (38%) did not have either MSI or LOH. (B) The bars demonstrate the mean methylation index based upon the number of markers methylated in the three subsets of CRCs.80 Methylation alterations were analyzed at 12 markers including 6 canonical CIMP markers (MINT-1, -2, -31, p16, p14 and MLH1) and 6 additional tumors suppressor genes (PTEN, TIMP3, RUNX3, HIC1, APC, and RARβ2). The three vertical columns represent the mean methylation ratios in MSI (blue), MSI-/LOH-(red) and LOH (white) CRCs. The error bars denote the S.D. The filled circles (color matched with vertical columns) represent the 95% confidence interval (CI) of the mean methylation ratios. The rectangular boxes in the upper panels represent the pair-wise correlation between the mean methylation ratios in each subset of CRC; p-values were calculated by the Wilcoxon test. As shown in the three panels, analysis of the methylation ratios using only four CIMP-related markers (versus using 12 or 6 CIMP-related markers) demonstrates a significant positive association for MSI and MSI-/LOH-tumors, but an inverse correlation for LOH CRCs. (C) The relationship between methylation ratios calculated using all 12 methylation markers was compared with LOH ratios in the total cohort of 126 CRCs. As shown, an inverse correlation was observed (p = -0.3690; p < 0.0001) between the methylation ratio and LOH.
CRC, colorectal cancers; MSI, microsatellite instability; LOH, loss of heterozygosity.

Fig. 2
KRAS and BRAF signaling play a role in aberrant methylation, and may contribute to epigenetic alterations in Lynch Syndrome cancers. (A) These 3 boxes show the average number of methylated loci in various subgroups of CRCs categorized by their BRAF/KRAS mutation status as published previously.31 The average number of methylated loci in each subset was calculated using all fourteen markers ("All Loci"), seven canonical CIMP markers ("CIMP") and the seven additional markers ("Non-CIMP"). The p values are based on Kruskal-Wallis one way analysis of variance on ranks, and represent the statistical differences among all three subsets of CRCs (BRAF-mutated, KRAS-mutated or wild type for both). BRAF-mutated cancers showed the highest degree of methylation at CIMP-related loci, and as a consequence, the highest degree of methylation when data were analyzed from "All Loci". KRAS mutated tumors exhibited methylation not only at the CIMP-markers, but interestingly, when data were analyzed from the additional (Non-CIMP) markers, there was a minimal difference in the number of markers methylated between BRAF- and KRAS-mutated cancers. (B) These 3 bar charts illustrate the average number of methylated loci in sporadic MSI (MSI-H), Lynch syndrome and non-MSI (MSI-L and MSS) CRCs.31 As expected, sporadic MSI tumors were most frequently methylated at all markers (CIMP and Non-CIMP). Lynch syndrome CRCs also demonstrated frequent methylation at canonical-CIMP markers, which was surprisingly slightly higher compared to the non-MSI tumors.
CRC, colorectal cancers; CIMP, CpG island methylator phenotype; MSI, microsatellite instability; MSS, microsatellite stable.

Fig. 3
Hepatocellular carcinomas (HCCs) are classified based upon methylation and mutational status. In the upper figure, all 81 HCCs are classified by hierarchical clustering analysis based upon the degree of methylation and β-catenin or p53 mutations as published previously.39 The heat map (green-black-red) shows the tumors with a lower methylation density as green, and higher methylation density as red. The Y-axis shows the loci analyzed. A solid triangle represents a tumor with a β-catenin mutation, and an open triangle indicates a HCC with a p53 mutation. As depicted, β-catenin mutations were significantly associated with the Group 2 HCCs on the right (p < 0.0001). The table in the lower half of the figure highlights the significant association between higher methylation in Group 2 HCCs and β-catenin mutations. FAL indicates the "fractional allelic loss", or proportion of analyzed loci with allelic imbalance, or LOH.

Fig. 4
Treatment with a demethylating agent restores sensitivity to 5-FU toxicity in a MMR-deficient CRC cell line. (A) The top schematic summarizes the treatment plan and results from the in-vitro experiments. Four CRC cell lines - HCT116 and HCT116 + 2 (both MMR-deficient due to mutation in MLH1), HCT116 + 3 (MMR-proficient following restoration of MLH1 gene with chromosome 3 transfer in HCT116 cells) and SW48 (MMR-deficient due to hypermethylation of MLH1) - were cultivated in growth medium or exposed to 5-AZA for 24 h.66 Culture medium was exchanged and cells were allowed to form colonies over a period of 10-12 days. During this time, the cells were continuously exposed to increasing concentrations of 5-FU. Cells were washed, fixed, stained and colonies counted. MLH1 methylation status, its expression (mRNA and protein), and sensitivity to 5-FU sensitivity were monitored in each experiment. (B) A representative graph (in the left panel) depicts the mean ± S.D. of three different experiments for the colony forming assay from CRC cell lines exposed to different doses of 5-FU (1 µM, 2.5 µM, and 5 µM). Cells were allowed to form colonies for 10-12 days. The means and S.D. of three independently performed experiments are shown. As indicated, only HCT116 + 3 cells (MMR proficient cells) are sensitive to 5-FU, while all MMR-deficient cells demonstrate more colonies, indicating resistance to the chemotherapeutic drug. However, when SW48 cells were pretreated with 5 µM 5-Aza for 24 h before 5-FU exposure, MMR activity is restored, and they behave similarly to the MMR-proficient HCT116 + 3 cells (right panel).
MMR, mismatch repair; CRC, colorectal cancers.
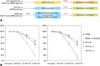
Fig. 5
An integrated model for different forms of genetic and epigenetic instability in CRC. Tumors can develop via chromosomal instability (CIN), microsatellite instability (MSI), or CpG island methylator phenotype (CIMP) pathways. MSI may develop either from Lynch syndrome (the hereditary form), or via the CIMP pathway (a presumably acquired form). Ultimately, all pathways converge pathologically as cancer. Based upon our current understanding, CIN and CIMP represent the two primary processes of genetic and epigenetic instability respectively, in the colon. In essence, MSI in sporadic CRCs originates because of CIMP, and once MLH1 becomes methylated, the tumors acquire MSI. Thus far the molecular mechanisms for CIN and CIMP are not clear, however, there are data to suggest that JC virus (JCV) may be a putative unifying mechanism for genetic and epigenetic instability in CRC.
CRC, colorectal cancers; MMR, mismatch repair.

ACKNOWLEDGEMENTS
This work was supported by NIH grants CA72851 and CA 98572 from the National Cancer Institute, and funds from the Baylor Research Institute.
References
1. Vogelstein B, Fearon ER, Kern SE, Hamilton SR, Preisinger AC, Nakamura Y, et al. Allelotype of colorectal carcinomas. Science. 1989. 244:207–211.

2. Goel A, Arnold CN, Niedzwiecki D, Chang DK, Ricciardiello L, Carethers JM, et al. Characterization of sporadic colon cancer by patterns of genomic instability. Cancer Res. 2003. 63:1608–1614.
3. Li R, Sonik A, Stindl R, Rasnick D, Duesberg P. Aneuploidy vs. gene mutation hypothesis of cancer: recent study claims mutation but is found to support aneuploidy. Proc Natl Acad Sci U S A. 2000. 97:3236–3241.

4. Lengauer C, Kinzler KW, Vogelstein B. Genetic instability in colorectal cancers. Nature. 1997. 386:623–627.

5. Nishida N, Nagasaka T, Kashiwagi K, Boland CR, Goel A. High copy amplification of the Aurora-A gene is associated with chromosomal instability phenotype in human colorectal cancers. Cancer Biol Ther. 2007. 6:525–533.

6. Rodriguez J, Frigola J, Vendrell E, Risques RA, Fraga MF, Morales C, et al. Chromosomal instability correlates with genome-wide DNA demethylation in human primary colorectal cancers. Cancer Res. 2006. 66:8462–9468.

7. Sieber OM, Heinimann K, Gorman P, Lamlum H, Crabtree M, Simpson CA, et al. Analysis of chromosomal instability in human colorectal adenomas with two mutational hits at APC. Proc Natl Acad Sci U S A. 2002. 99:16910–16915.

8. Boland CR, Komarova NL, Goel A. Chromosomal instability and cancer: not just one CINgle mechanism. Gut. 2009. 58:163–164.

9. Muleris M, Chalastanis A, Meyer N, Lae M, Dutrillaux B, Sastre-Garau X, et al. Chromosomal instability in near-diploid colorectal cancer: a link between numbers and structure. PLoS ONE. 2008. 3:e1632.

10. Duval A, Reperant M, Compoint A, Seruca R, Ranzani GN, Iacopetta B, et al. Target gene mutation profile differs between gastrointestinal and endometrial tumors with mismatch repair deficiency. Cancer Res. 2002. 62:1609–1612.
11. Markowitz S, Wang J, Myeroff L, Parsons R, Sun L, Lutterbaugh J, et al. Inactivation of the type II TGF-beta receptor in colon cancer cells with microsatellite instability. Science. 1995. 268:1336–1338.

12. Rampino N, Yamamoto H, Ionov Y, Li Y, Sawai H, Reed JC, et al. Somatic frameshift mutations in the BAX gene in colon cancers of the microsatellite mutator phenotype. Science. 1997. 275:967–969.

13. Grady WM, Carethers JM. Genomic and epigenetic instability in colorectal cancer pathogenesis. Gastroenterology. 2008. 135:1079–1099.

14. Toyota M, Ahuja N, Ohe-Toyota M, Herman JG, Baylin SB, Issa JP. CpG island methylator phenotype in colorectal cancer. Proc Natl Acad Sci U S A. 1999. 96:8681–8686.

15. Herman JG, Baylin SB. Gene silencing in cancer in association with promoter hypermethylation. N Engl J Med. 2003. 349:2042–2054.

16. Yamashita K, Dai T, Dai Y, Yamamoto F, Perucho M. Genetics supersedes epigenetics in colon cancer phenotype. Cancer Cell. 2003. 4:121–131.

17. Ahuja N, Mohan AL, Li Q, Stolker JM, Herman JG, Hamilton SR, et al. Association between CpG island methylation and microsatellite instability in colorectal cancer. Cancer Res. 1997. 57:3370–3374.
18. Kane MF, Loda M, Gaida GM, Lipman J, Mishra R, Goldman H, et al. Methylation of the hMLH1 promoter correlates with lack of expression of hMLH1 in sporadic colon tumors and mismatch repair-defective human tumor cell lines. Cancer Res. 1997. 57:808–811.
19. Weisenberger DJ, Siegmund KD, Campan M, Young J, Long TI, Faasse MA, et al. CpG island methylator phenotype underlies sporadic microsatellite instability and is tightly associated with BRAF mutation in colorectal cancer. Nat Genet. 2006. 38:787–793.

20. Eads CA, Danenberg KD, Kawakami K, Saltz LB, Danenberg PV, Laird PW. CpG island hypermethylation in human colorectal tumors is not associated with DNA methyltransferase overexpression. Cancer Res. 1999. 59:2302–2306.
21. Samowitz WS, Albertsen H, Herrick J, Levin TR, Sweeney C, Murtaugh MA, et al. Evaluation of a large, population-based sample supports a CpG island methylator phenotype in colon cancer. Gastroenterology. 2005. 129:837–845.
22. Goel A, Nagasaka T, Arnold CN, Inoue T, Hamilton C, Niedzwiecki D, et al. The CpG island methylator phenotype and chromosomal instability are inversely correlated in sporadic colorectal cancer. Gastroenterology. 2007. 132:127–138.
23. Ogino S, Odze RD, Kawasaki T, Brahmandam M, Kirkner GJ, Laird PW, et al. Correlation of pathologic features with CpG island methylator phenotype (CIMP) by quantitative DNA methylation analysis in colorectal carcinoma. Am J Surg Pathol. 2006. 30:1175–1183.
24. Tuupanen S, Karhu A, Järvinen H, Mecklin JP, Launonen V, Aaltonen LA. No evidence for dual role of loss of heterozygosity in hereditary non-polyposis colorectal cancer. Oncogene. 2007. 26:2513–2517.
25. Kaz A, Kim YH, Dzieciatkowski S, Lynch H, Watson P, Kay Washington M, et al. Evidence for the role of aberrant DNA methylation in the pathogenesis of Lynch syndrome adenomas. Int J Cancer. 2007. 120:1922–1929.
26. Wood LD, Parsons DW, Jones S, Lin J, Sjöblom T, Leary RJ, et al. The genomic landscapes of human breast and colorectal cancers. Science. 2007. 318:1108–1113.
27. Nagasaka T, Goel A, Notohara K, Takahata T, Sasamoto H, Uchida T, et al. Methylation pattern of the O6-methylguanine-DNA methyltransferase gene in colon during progressive colorectal tumorigenesis. Int J Cancer. 2008. 122:2429–2436.

28. Forrester K, Almoguera C, Han K, Grizzle WE, Perucho M. Detection of high incidence of K-ras oncogenes during human colon tumorigenesis. Nature. 1987. 327:298–303.

29. Bos JL, Fearon ER, Hamilton SR, Verlaan-de Vries M, van Boom JH, van der Eb AJ, et al. Prevalence of ras gene mutations in human colorectal cancers. Nature. 1987. 327:293–297.

30. Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, et al. Mutations of the BRAF gene in human cancer. Nature. 2002. 417:949–954.

31. Nagasaka T, Koi M, Kloor M, Gebert J, Vilkin A, Nishida N, et al. Mutations in both KRAS and BRAF may contribute to the methylator phenotype in colon cancer. Gastroenterology. 2008. 134:1950.e1–1960.e1.

32. Aaltonen LA, Peltomäki P, Mecklin JP, Järvinen H, Jass JR, Green JS, et al. Replication errors in benign and malignant tumors from hereditary nonpolyposis colorectal cancer patients. Cancer Res. 1994. 54:1645–1648.
33. Tannergård P, Liu T, Weger A, Nordenskjöld M, Lindblom A. Tumorigenesis in colorectal tumors from patients with hereditary non-polyposis colorectal cancer. Hum Genet. 1997. 101:51–55.

34. Esteller M, Fraga MF, Guo M, Garcia-Foncillas J, Hedenfalk I, Godwin AK, et al. DNA methylation patterns in hereditary human cancers mimic sporadic tumorigenesis. Hum Mol Genet. 2001. 10:3001–3007.

35. Sanchez de Abajo A, de la Hoya M, van Puijenbroek M, Godino J, Díaz-Rubio E, Morreau H, et al. Dual role of LOH at MMR loci in hereditary non-polyposis colorectal cancer? Oncogene. 2006. 25:2124–2130.

36. Kim WS, Son HJ, Park JO, Song SY, Park C. Promoter methylation and down-regulation of DAPK is associated with gastric atrophy. Int J Mol Med. 2003. 12:827–830.
37. Garcia-Manero G, Bueso-Ramos C, Daniel J, Williamson J, Kantarjian HM, Issa JP. DNA methylation patterns at relapse in adult acute lymphocytic leukemia. Clin Cancer Res. 2002. 8:1897–1903.
38. Shen L, Ahuja N, Shen Y, Habib NA, Toyota M, Rashid A, et al. DNA methylation and environmental exposures in human hepatocellular carcinoma. J Natl Cancer Inst. 2002. 94:755–761.

39. Nishida N, Nishimura T, Nagasaka T, Ikai I, Goel A, Boland CR. Extensive methylation is associated with beta-catenin mutations in hepatocellular carcinoma: evidence for two distinct pathways of human hepatocarcinogenesis. Cancer Res. 2007. 67:4586–4594.

40. Nishida N, Nagasaka T, Nishimura T, Ikai I, Boland CR, Goel A. Aberrant methylation of multiple tumor suppressor genes in aging liver, chronic hepatitis, and hepatocellular carcinoma. Hepatology. 2008. 47:908–918.
41. Greger V, Passarge E, Höpping W, Messmer E, Horsthemke B. Epigenetic changes may contribute to the formation and spontaneous regression of retinoblastoma. Hum Genet. 1989. 83:155–158.

43. Li E. Chromatin modification and epigenetic reprogramming in mammalian development. Nat Rev Genet. 2002. 3:662–673.

44. Slattery ML, Curtin K, Sweeney C, Levin TR, Potter J, Wolff RK, et al. Diet and lifestyle factor associations with CpG island methylator phenotype and BRAF mutations in colon cancer. Int J Cancer. 2007. 120:656–663.

45. Samowitz WS, Albertsen H, Sweeney C, Herrick J, Caan BJ, Anderson KE, et al. Association of smoking, CpG island methylator phenotype, and V600E BRAF mutations in colon cancer. J Natl Cancer Inst. 2006. 98:1731–1738.

46. Kaneko Y, Sakurai S, Hironaka M, Sato S, Oguni S, Sakuma Y, et al. Distinct methylated profiles in Helicobacter pylori dependent and independent gastric MALT lymphomas. Gut. 2003. 52:641–646.
47. Maekita T, Nakazawa K, Mihara M, Nakajima T, Yanaoka K, Iguchi M, et al. High levels of aberrant DNA methylation in Helicobacter pylori-infected gastric mucosae and its possible association with gastric cancer risk. Clin Cancer Res. 2006. 12:989–995.

48. Chan AO, Peng JZ, Lam SK, Lai KC, Yuen MF, Cheung HK, et al. Eradication of Helicobacter pylori infection reverses E-cadherin promoter hypermethylation. Gut. 2006. 55:463–468.

49. Perri F, Cotugno R, Piepoli A, Merla A, Quitadamo M, Gentile A, et al. Aberrant DNA methylation in non-neoplastic gastric mucosa of H. Pylori infected patients and effect of eradication. Am J Gastroenterol. 2007. 102:1361–1371.

50. Goel A, Li MS, Nagasaka T, Shin SK, Fuerst F, Ricciardiello L, et al. Association of JC virus T-antigen expression with the methylator phenotype in sporadic colorectal cancers. Gastroenterology. 2006. 130:1950–1961.

51. Herath NI, Leggett BA, MacDonald GA. Review of genetic and epigenetic alterations in hepatocarcinogenesis. J Gastroenterol Hepatol. 2006. 21:15–21.

52. Kang GH, Lee S, Kim WH, Lee HW, Kim JC, Rhyu MG, et al. Epstein-barr virus-positive gastric carcinoma demonstrates frequent aberrant methylation of multiple genes and constitutes CpG island methylator phenotype-positive gastric carcinoma. Am J Pathol. 2002. 160:787–794.

53. Ohm JE, McGarvey KM, Yu X, Cheng L, Schuebel KE, Cope L, et al. A stem cell-like chromatin pattern may predispose tumor suppressor genes to DNA hypermethylation and heritable silencing. Nat Genet. 2007. 39:237–242.

54. Ohm JE, Baylin SB. Stem cell chromatin patterns: an instructive mechanism for DNA hypermethylation? Cell Cycle. 2007. 6:1040–1043.

55. Rashid A, Shen L, Morris JS, Issa JP, Hamilton SR. CpG island methylation in colorectal adenomas. Am J Pathol. 2001. 159:1129–1135.

56. Chan AO, Broaddus RR, Houlihan PS, Issa JP, Hamilton SR, Rashid A. CpG island methylation in aberrant crypt foci of the colorectum. Am J Pathol. 2002. 160:1823–1830.

57. Shin SK, Nagasaka T, Jung BH, Matsubara N, Kim WH, Carethers JM, et al. Epigenetic and genetic alterations in Netrin-1 receptors UNC5C and DCC in human colon cancer. Gastroenterology. 2007. 133:1849–1857.

58. Ahlquist DA, Skoletsky JE, Boynton KA, Harrington JJ, Mahoney DW, Pierceall WE, et al. Colorectal cancer screening by detection of altered human DNA in stool: feasibility of a multitarget assay panel. Gastroenterology. 2000. 119:1219–1227.

59. Müller HM, Oberwalder M, Fiegl H, Morandell M, Goebel G, Zitt M, et al. Methylation changes in faecal DNA: a marker for colorectal cancer screening? Lancet. 2004. 363:1283–1285.

60. Nagasaka T, Goel A, Matsubara N, Tanaka N. Detection of fecal DNA methylation for colorectal neoplasia: does it lead to an optimal screening test? Acta Med Okayama. 2006. 60:249–256.
61. Chen WD, Han ZJ, Skoletsky J, Olson J, Sah J, Myeroff L, et al. Detection in fecal DNA of colon cancer-specific methylation of the nonexpressed vimentin gene. J Natl Cancer Inst. 2005. 97:1124–1132.

62. Zou H, Taylor WR, Harrington JJ, Hussain FT, Cao X, Loprinzi CL, et al. High detection rates of colorectal neoplasia by stool DNA testing with a novel digital melt curve assay. Gastroenterology. 2009. 136:459–470.

64. Mitsuno M, Kitajima Y, Ide T, Ohtaka K, Tanaka M, Satoh S, et al. Aberrant methylation of p16 predicts candidates for 5-fluorouracil-based adjuvant therapy in gastric cancer patients. J Gastroenterol. 2007. 42:866–873.

65. Stresemann C, Lyko F. Modes of action of the DNA methyltransferase inhibitors azacytidine and decitabine. Int J Cancer. 2008. 123:8–13.
66. Arnold CN, Goel A, Boland CR. Role of hMLH1 promoter hypermethylation in drug resistance to 5-fluorouracil in colorectal cancer cell lines. Int J Cancer. 2003. 106:66–73.

67. Oki Y, Issa JP. Review: recent clinical trials in epigenetic therapy. Rev Recent Clin Trials. 2006. 1:169–182.

68. Kaminskas E, Farrell A, Abraham S, Baird A, Hsieh LS, Lee SL, et al. Approval summary: azacitidine for treatment of myelodysplastic syndrome subtypes. Clin Cancer Res. 2005. 11:3604–3608.

69. Hellebrekers DM, Griffioen AW, van Engeland M. Dual targeting of epigenetic therapy in cancer. Biochim Biophys Acta. 2007. 1775:76–91.
70. Walker DL, Padgett BL, ZuRhein GM, Albert AE, Marsh RF. Human papovavirus (JC): induction of brain tumors in hamsters. Science. 1973. 181:674–676.
71. Gordon J, Khalili K. The human polyomavirus, JCV, and neurological diseases (review). Int J Mol Med. 1998. 1:647–655.

72. Boland CR, Luciani MG, Gasche C, Goel A. Infection, inflammation, and gastrointestinal cancer. Gut. 2005. 54:1321–1331.

73. Laghi L, Randolph AE, Chauhan DP, Marra G, Major EO, Neel JV, et al. JC virus DNA is present in the mucosa of the human colon and in colorectal cancers. Proc Natl Acad Sci U S A. 1999. 96:7484–7489.

74. Ricciardiello L, Laghi L, Ramamirtham P, Chang CL, Chang DK, Randolph AE, et al. JC virus DNA sequences are frequently present in the human upper and lower gastrointestinal tract. Gastroenterology. 2000. 119:1228–1235.

75. Jung WT, Li MS, Goel A, Boland CR. JC virus T-antigen expression in sporadic adenomatous polyps of the colon. Cancer. 2008. 112:1028–1036.

76. Enam S, Del Valle L, Lara C, Gan DD, Ortiz-Hidalgo C, Palazzo JP, et al. Association of human polyomavirus JCV with colon cancer: evidence for interaction of viral T-antigen and beta-catenin. Cancer Res. 2002. 62:7093–7101.
77. Casini B, Borgese L, Del Nonno F, Galati G, Izzo L, Caputo M, et al. Presence and incidence of DNA sequences of human polyomaviruses BKV and JCV in colorectal tumor tissues. Anticancer Res. 2005. 25:1079–1085.
78. Theodoropoulos G, Panoussopoulos D, Papaconstantinou I, Gazouli M, Perdiki M, Bramis J, et al. Assessment of JC polyoma virus in colon neoplasms. Dis Colon Rectum. 2005. 48:86–91.

79. Ricciardiello L, Baglioni M, Giovannini C, Pariali M, Cenacchi G, Ripalti A, et al. Induction of chromosomal instability in colonic cells by the human polyomavirus JC virus. Cancer Res. 2003. 63:7256–7262.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download