This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Previous lumbar spinal surgery (PLSS) is not currently considered as a contraindication for regional anesthesia. However, there are still problems that make spinal anesthesia more difficult with a possibility of worsening the patient's back pain. Spinal anesthesia using combined spinal-epidural anesthesia (CSEA) in elderly patients with or without PLSS was investigated and the anesthetic characteristics, success rates, and possible complications were evaluated.
Materials and Methods
Fifty patients without PLSS (Control group) and 45 patients with PLSS (PLSS group) who were scheduled for total knee arthroplasty were studied prospectively. A CSEA was performed with patients in the left lateral position, and 10 mg of 0.5% isobaric tetracaine was injected through a 27 G spinal needle. An epidural catheter was then inserted for patient controlled analgesia. Successful spinal anesthesia was defined as adequate sensory block level more than T12. The number of skin punctures and the onset time were recorded, and maximal sensory block level (MSBL), time to 2-segment regression, success rate and complications were observed.
Results
The success rate of CSEA in Control group and PLSS group was 98.0%, and 93.3%, respectively. The median MSBL in PLSS group was higher than Control group [T4 (T2-L1) vs. T6 (T3-T12)] (p < 0.001). There was a significant difference in the number of patients who required ephedrine for the treatment of hypotension in PLSS group (p = 0.028).
Conclusion
The success rate of CSEA in patients with PLSS was 93.3%, and patients experienced no significant neurological complications. The MSBL can be higher in PLSS group than Control group.
Keywords: Anesthetics local, tetracaine, anesthetic techniques, subarachnoid, surgery, spinal
INTRODUCTION
Spinal anesthesia is not currently considered as a contraindication in patients with previous spinal surgery.
1,
2 However, the elderly population often have multiple comorbidities undergoing total knee arthroplasty or total hip arthroplasty. Thus, significant perioperative morbidity and mortality may occur.
3 The main benefits of regional anesthesia for the elderly are to lessen intraoperative blood loss, perioperative cardiac ischemic events, postoperative hypoxic episodes, and arterial and venous thrombosis, and to provide appropriate postoperative pain control.
4-
7
In spite of these advantages, anesthesiologists may prefer general anesthesia rather than spinal or epidural anesthesia in patients with previous lumbar spinal surgery (PLSS), even though some investigators reported that spinal and epidural anesthesia techniques can be performed successfully in patients with PLSS.
1,
2,
8,
9 Several problems may arise in these patients, including altered anatomy, which makes spinal or epidural injection more technically difficult, a possibility of worsening back pain and ineffective spread of local anesthetics in the subarachnoid space.
6 Lumbar spine surgery can cause postoperative epidural fibrosis, influencing the spread of spinal anesthetics if spinal stenosis which resulted from the postoperative epidural fibrosis exists immediately above the site of surgery.
10
The following prospective study was performed on elderly patients with or without PLSS undergoing spinal anesthesia using combined spinal-epidural anesthesia (CSEA) technique. The main purpose was to evaluate the difference of the maximal sensory block level (MSBL) of the spinal anesthesia. In addition, we evaluated the success rates, onset time to L1 dermatome, time to 2-segment regression and possible complications.
MATERIALS AND METHODS
The study was approved by the Hospital Ethics Committee (Severance Hospital IRB), and written informed consent was obtained from patients before surgery. Patients with infectious diseases, a history of neurological disease, drug allergies, and coagulopathies were excluded from the study. Ninety-five patients who were the American Society of Anesthesiologists physical status I-III, and scheduled to have elective total knee arthroplasty under CSEA, were enrolled. Fifty patients without PLSS (Control group) and forty-five with PLSS (PLSS group) were studied prospectively.
Patients fasted for 8 hours preoperatively and were not premedicated. All patients were questioned about pre-existing back pain before anesthesia. Patients were monitored with an electrocardiograph, non-invasive blood pressure monitor, and pulse-oximeter in the operating theater. Lactated Ringer's solution was injected intravenously in all patients via a 20-gauge i.v. catheter and external jugular vein was accessed for blood transfusion with an 18-gauge i.v. catheter. Patients received approximately 300 mL of lactated Ringer's solution rapidly before spinal anesthesia.
A CSEA was performed in all patients. Patients were placed in the left lateral position, using a midline approach at the L3-4 interspace in Control group. For patients in the PLSS group, the segmental level of previous laminectomy and/or fusion was established using lumbar anterior-posterior and lateral X-rays. Lumbar interspaces were determined by counting the spines of the vertebrae from both the cranial and caudal directions and palpating the iliac crest to confirm the position of the fourth lumbar vertebrae. A CSEA was performed using a midline approach at the upper level of previous operation. A CSEA in all patients was performed with a combined spinal-epidural kit (Espocan®, B. Braun, Melsungen, Germany). After local infiltration with 2 mL of 1% lidocaine, an 18-gauge epidural needle was placed first in the epidural space using loss of resistance technique with air. A 27-gauge spinal needle was then introduced through the epidural needle into the subarachnoid space, and free flow of cerebrospinal fluid (CSF) was observed. The spinal anesthetic solution was prepared as follows: 1 mL of 1% tetracaine was taken from a vial of mixing powder tetracaine (Pantocainsterile inj.®, Daihan Pharm., Seoul, Korea) that was dissolved in 2 mL of 0.9% NaCl. This was mixed with 1 mL of patient's CSF and 0.1 mL of 0.1% epinephrine to make 2 mL of 0.5% isobaric tetracaine. The 2 mL of 0.5% isobaric tetracaine was injected at a rate of 0.1 mL/sec with the upward orientation of the spinal needle bevel. Finally, 4 centimeters of the epidural catheter was threaded through the epidural needle remained in the epidural space for additional rescue anesthetics and patient controlled analgesia. Immediately after the epidural catheter was secured, the patient was gently returned to the supine position.
The level of lumbar puncture and number of skin punctures for detecting the epidural space during the CSEA were recorded. The onset time to the sensory block level L1 was defined as bilateral complete loss of pinprick sensation to a 22-gauge hypodermic needle. The patterns of block, including patchy blockade, and the evolution of sensory and motor blocks on both sides were checked every 5 minutes for the first 30 minutes after intrathecal injection, then every 10 minutes until the two pinprick block level regressed.
The MSBL and time to 2-segment regression from MSBL were checked throughout the surgery by another anesthesiologist blinded to the patient grouping. The successful spinal anesthesia was defined as adequate sensory block level more than T12. The success rate and complications were observed.
Mean arterial pressure and heart rate were recorded every 5 minutes for 30 minutes after intrathecal injection and monitored throughout the surgery. Atropine (0.5 mg) was administered intravenously when heart rate was lower than 45 beat/min. If the systolic arterial pressure decreased to less than 90 mmHg or a decrease of mean arterial pressure by more than 25% of the baseline value, 12 mg of ephedrine was administered intravenously.
Patients were also evaluated for the first 2 postoperative days by an investigator blinded on possible side effects; including headache (positional headache was considered to be a post-dural puncture headache), back pain, and transient neurologic symptoms, which are defined as pain radiating to the buttocks or legs and sensory disturbances on areas not related to the surgery. Final questionnaire survey about the back pain was performed by a blinded investigator via telephone 3 months after surgery.
For the purpose of statistical analyses, each dermatomal level was scored in sequence starting at S5 = 1, such that S1 = 5, L1 = 10, T8 = 15, and T3 = 20. Statistical analyses were performed using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA). Based on the primary results of a pilot study on the difference in MSBL between two groups, more than 36 patients in each group were required in order to detect a difference of 2 dermatome anesthesia levels to pinprick between Control and PLSS group with α error of 0.05 and β error of 0.2. Therefore, we studied 45 patients for PLSS group and 50 patients for Control group in this study. The puncture site and MSBL were analyzed using Mann-Whitney U-test. The number of skin puncture, onset time, and time to two-segment regression were analyzed using unpaired Student's t-test. The incidences of ephedrine or atropine requirements were analyzed by Pearson's Chi-square test, and the success rates of CSEA were analyzed by Fisher's exact test. Data are presented as mean (SD), median (range), or frequencies, as appropriate. A p-value < 0.05 was considered statistically significant.
RESULTS
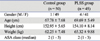
The 2 groups were not statistically different with respect to age, height, weight, and American Society of Anesthesidogists (ASA) class (
Table 1). The median level of lumbar puncture in PLSS group was significantly higher than that of Control group (
p < 0.001). No difference in the number of skin punctures for detecting the epidural space was observed between the two groups. The mean (SD) onset time to the sensory block level L1 in PLSS group was significantly faster than that of the Control group (
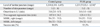
p < 0.01). The median MSBL was higher in PLSS group than Control group (
p < 0.001) (
Fig. 1,
Table 2). The success rates for spinal anesthesia were comparable between the 2 groups.
Patients with PLSS were divided into 2 categories: 1) those who underwent laminectomy (n = 26); and 2) those who underwent posterior lumbar interbody fusion (n = 19). The types of PLSS did not influence the onset time, MSBL, and time to two-segment regression.
We failed to detect the epidural space in two patients in PLSS group during CSEA, each of whom had extensive spinal fusions (L4-S1, and L2-S1, respectively). One patient who had history of 3 lumbar spinal laminectomies and fusions at L3-5 experienced patchy block following spinal anesthesia (MSBL only extended to L1). And these 3 patients were converted to general anesthesia for surgery. Eleven patients (22.0%) in Control group and nineteen patients (42.2%) in PLSS group required ephedrine for treatment of hypotension (p = 0.022). One patient in PLSS group required atropine for bradycardia.
After successful injection of spinal anesthetic solution in the 2 PLSS patients, the epidural catheter was incidentally inserted into the subarachnoid space during placement through the epidural needle. Immediately after epidural catheter insertion, the free flow of CSF was observed through the epidural catheter. After the epidural catheter was removed, another catheter was inserted in the space above for postoperative pain control. There was no postdural puncture headache or neurologic injury in these 2 patients.
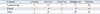
The questionnaire for worsening of back pain was assessed 3 months after spinal anesthesia. In Control group, 10 of 50 patients (20%) had pre-existing back pain with no newly developed back pain and 4 of 10 patients with pre-existing back pain (40%) complained of worsening of back pain. In PLSS group, 14 of 45 patients (31%) had pre-existing back pain. In addition, the 2 patients complained of newly developed back pain and 7 of the 14 patients with pre-existing back pain (50%) complained of worsening of the back pain. Nevertheless, none of these patients stated that their back pain interfered with daily activities (
Table 3).
DISCUSSION
The present study showed that MSBL in PLSS group was higher than in Control group at the same dose of spinal anesthetic solution. The success rate of spinal anesthesia in PLSS groups was comparable with that of Control group.
MSBL (range) was higher in patients with PLSS than that in patients without PLSS. This inconsistent result may be explained by the higher puncture site level of CSEA and the postoperative anatomical changes of intra- and extra-dural structure in patients with PLSS. Although the level of injection site is one of the well-known factors affecting the intrathecal spread of local anesthetics in spinal anesthesia,
11-
14 MSBL cannot be explained with the level of injection of anesthetics alone. Lumbar spine surgery can cause adhesive changes in the epidural space, and these postoperative epidural fibrosis may alter the anatomy of the subarachnoid space after spine surgery, including the narrowing of the spinal canal,
15-
17 influencing the spread of spinal anesthetics if spinal stenosis which resulted from the postoperative epidural fibrosis exists immediately above the site of surgery.
17 According to a report of a spinal anesthesia in a patient who had 4 myelograms, 3 lumbar spinal laminectomies and fusions at L4-5, MSBL of anesthesia extended only to L1 and the spinal anesthesia resulted in a patchy, failed block.
8 The relatively low level of sensory blockade and the presence of unblocked segments in this study could be explained by ineffective spread of local anesthetics in the subarachnoid space which was altered by postoperative scar tissue. In our study, CSEA was performed at the upper level of previous operation. Thus, the relatively high level of sensory blockade could be explained by the easy spread of local anesthetics more cephalad due to the postoperative stenotic change in the subarachnoid space. To evaluate the inter-relationship between level of spinal anesthesia and PLSS, magnetic resonance imaging studies should be performed to confirm anatomical changes of the intra- and extra-dural structures in these patients.
18 The onset time for sensory block to L1 was significantly faster in PLSS group. Postoperative structural changes in PLSS group might allow the drug to spread cephalad more rapidly than in Control group.
In our study, the PLSS group had a tendency towards higher incidence of hypotension and bradycardia, which can be explained by the higher spinal block level. This suggests that the dose of spinal anesthetics should be reduced when spinal anesthesia is planned in patients with PLSS at a higher level than the previous operative site. In addition, a reduced dose of anesthetics can help diminish the risk of hemodynamic problems resulting from high spinal block.
While there was only 1 case in which we failed to detect the epidural space during CSEA in Control group, there were 2 failed cases in PLSS group, each of whom received extensive spinal fusion operations. This was thought to be due to the anatomical changes following spinal surgery. One patient experienced patchy block requiring general anesthesia. This result could be explained by ineffective spread of local anesthetics in the subarachnoid space, altered by postoperative scar tissue. Also, incidental insertion of an epidural catheter into the subarachnoid space occurred in two PLSS patients, most likely due to tethering of the dura and surrounding tissue, and intra- and extra-dural scarring after spinal operations. Although there was no statistical significance, the PLSS group showed an 11% rate of procedural problems in the quality of anesthesia and potential of neurologic complications during CSEA.
Although there are no existing data to support the worsening of persistent back pain after CSEA in patients with PLSS, the possibility of back pain aggravation is usually one of the reasons why anesthesiologists prefer general anesthesia in patients with PLSS. We found that 7 of 14 patients (50%) with pre-existing back pain complained of worsening of the persistent back pain and 2 patients in PLSS group complained of newly developed back pain. Also, 4 of 10 patients (40%) with pre-existing back pain in Control group complained of worsening of the persistent back pain. Consequently, 9 patients (20%) in PLSS group and 4 patients (8%) in Control group complained of worsening or newly developed back pain. Although this data are statistically insignificant in itself and impossible to compare them directly with previous reports, the results are similar to those of Kock et al.
19 and Schwabe et al.
20 who reported the incidence of persistent back pain after spinal anesthesia as 12.3% and 11.5%, respectively. It is quite possible that the incidence of long term back pain following CSEA is likely to be associated with preexisting back pain, rather than the history of PLSS itself.
There are some limitations in this study. First, spinal anesthesia was performed above the L2/3 interspace in some patients because of their postoperative structural changes. Also, there was a potential risk of direct-needle trauma to the spinal cord due to the high puncture site level in PLSS group. Most anesthesiologists suggest that spinal anesthesia should be attempted below the level of L2/3.
21,
22 Second, the dose of tetracaine used in this study resulted in relatively high MSBL for knee arthroplasty. In spite of the benefit of CSEA technique that allows the intrathecal dose to be minimal, 10 mg of tetracaine was administered in order to evaluate the patterns of spinal anesthesia in patients with PLSS.
In summary, spinal anesthesia using CSEA technique can be performed in patients with PLSS. As MSBL may be higher in patients with PLSS, reduced dose of anesthetics can help diminish the risk of hemodynamic problems which resulted from high spinal block.
ACKNOWLEDGEMENTS
The study was approved by the Hospital Ethics Committee (Severance Hospital IRB), and written informed consent was obtained from patients before surgery. Presented in part at the European Society of Anaesthesiologists, Muchen Meeting, June 11, 2007.
References
1. Berkowitz S, Gold MI. Spinal anesthesia for surgery in patients with previous lumbar laminectomy. Anesth Analg. 1980. 59:881–882.

2. Jost U, Wolter E, Böhrer H. [Spinal anaesthesia in 50 patients with previous lumbar spinal surgery.]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2004. 39:78–80.
3. Gomersall CD, Ramsay SJ, Leung P. Hospital and 28-day mortality amongst 'high risk' surgical patients. A retrospective cohort study. Anaesth Intensive Care. 2008. 36:20–24.

4. Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ. 2000. 321:1493.

5. Urwin SC, Parker MJ, Griffiths R. General versus regional anaesthesia for hip fracture surgery: a meta-analysis of randomized trials. Br J Anaesth. 2000. 84:450–455.

6. Indelli PF, Grant SA, Nielsen K, Vail TP. Regional anesthesia in hip surgery. Clin Orthop Relat Res. 2005. 441:250–255.

7. Sakura S. [Epidural anesthesia and spinal anesthesia in the elderlyg.]. Masui. 2007. 56:130–138.
8. Sun KO. Spinal anaesthesia following previous spinal surgery. Eur J Anaesthesiol. 1994. 11:321–323.
9. Sharrock NE, Urquhart B, Mineo R. Extradural anaesthesia in patients with previous lumbar spine surgery. Br J Anaesth. 1990. 65:237–239.

10. Brodsky AE. Post-laminectomy and post-fusion stenosis of the lumbar spine. Clin Orthop Relat Res. 1976. 130–139.

11. Hocking G, Wildsmith JA. Intrathecal drug spread. Br J Anaesth. 2004. 93:568–578.

12. Lowson SM, Brown J, Wilkins CJ. Influence of the lumbar interspace chosen for injection on the spread of hyperbaric 0.5% bupivacaine. Br J Anaesth. 1991. 66:465–468.

13. Tuominen M, Taivainen T, Rosenberg PH. Spread of Spinal anaesthesia with plain 0.5% bupivacaine: influence of the vertebral interspace used for injection. Br J Anaesth. 1989. 62:358–361.

14. Sakura S, Sumi M, Morimoto N, Yamamori Y, Saito Y. Spinal anesthesia with tetracaine in 0.75% glucose: influence of the vertebral interspace used for injection. Reg Anesth Pain Med. 1998. 23:170–175.

15. Takahashi N, Konno S, Kikuchi S. A histologic and functional study on cauda equina adhesion induced by multiple level laminectomy. Spine. 2003. 28:4–8.

16. Carroll SE, Wiesel SW. Neurologic complications and lumbar laminectomy. A standardized approach to the multiply-operated lumbar spine. Clin Orthop Relat Res. 1992. 14–23.
17. O'Connor M, Brighouse D, Glynn CJ. Unusual complications of the treatment of chronic spinal arachnoiditis. Clin J Pain. 1990. 6:240–242.
18. Ross JS, Robertson JT, Frederickson RC, Petrie JL, Obuchowski N, Modic MT, et al. ADCON-L European Study Group. Association between peridural scar and recurrent radicular pain after lumbar discectomy: magnetic resonance evaluation. Neurosurgery. 1996. 38:855–861. discussion 861-3.
19. Kock S, Hopf HB. [Incidence and predisposing factors of persistent backache after lumbar catheter epidural anesthesia in a non-obstetrical setting.]. Anasthesiol Intensivmed Notfallmed Schmerzther. 1998. 33:648–652.

20. Schwabe K, Hopf HB. Persistent back pain after spinal anaesthesia in the non-obstetric setting: incidence and predisposing factors. Br J Anaesth. 2001. 86:535–539.

21. Saifuddin A, Burnett SJ, White J. The variation of position of the conus medullaris in an adult population. A magnetic resonance imaging study. Spine. 1998. 23:1452–1456.

22. Reynolds F. Damage to the conus medullaris following spinal anaesthesia. Anaesthesia. 2001. 56:238–247.






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download