Abstract
Purpose
Aortic dissection (AoD) is one of the most common catastrophes involving the aorta. Nevertheless, early diagnosis remains to be a challenge in the Emergency Department (ED), particularly in young individuals. In this study, we attempted to identify the characteristics of acute AoD among young individuals, particular in patients with Marfan syndrome.
Materials and Methods
This was an retrospective chart-review study conducted in a tertiary referring hospital. The hospital database was queried for the combination of AoD and patients under age of 40 years. The medical charts were reviewed to obtain demographic data, clinical data and laboratory characteristics by using a standardized data collection sheet. A comparison between Marfan syndrome and non-Marfan syndrome patients was performed.
Results
During the 10-years period, 18 of 344 patients with acute AoD were younger than 40 years-old. Patients with Marfan syndrome developed acute AoD at a younger age than patients without Marfan syndrome. The mean diastolic blood pressure was significantly lower in patients with Marfan syndrome upon presenting to the ED than those without. Patients with Marfan syndrome had trends toward higher risk of development of type A AoD, increased recurrence rate and higher mortality rate than those without. However, statistical significance was not present.
Conclusion
ED physicians should have high alert to acute AoD in young patients presenting with severe unexplained chest and back pain, particularly in those patients with a history of heart diseases, hypertension, and Marfan syndrome or featuring Marfanoid habitus. Acute coronary syndrome, unexplained abdominal symptoms, and sudden cardiac arrest could be the initial manifestation of AoD in young patients. A low threshold to perform enhanced computed tomography may facilitate early diagnosis and timely treatment in this patient population.
Aortic dissection (AoD) is one of the most common catastrophes involving the aorta. It requires a timely diagnosis and, if the condition is unrecognized and untreated, the related mortality is particularly high during the first 48 hours.1 The time elapsed between onset of a type A dissection and intervention is directly correlated with survival, with mortality increasing by 1% per hour.2 Early diagnosis of acute AoD before development of cardiac tamponade and renal impairment is critical to improve the operative salvage rate of AoD.3 The peak age of the occurrence of proximal dissection is between 50 and 55 years, and that of distal dissection is between 60 and 70 years. Twenty-one percent of patients with AoD die prior to hospital admission.4 Chronic systemic hypertension is the most common factor precipitating the AoD and is present in 62% to 78% of patients with AoD. Nevertheless, the most common predisposing conditions for AoD in children and young adults are cardiovascular abnormalities, and other frequent predisposing factors include disorders of connective tissue such as Marfan syndrome, Ehlers-Danlos syndrome type IV, and Tuner syndrome.5 Typical risk factors, symptoms/signs and outcomes of AoD have been delineated in previous studies, nevertheless, the usefulness of these presentations may be limited, particularly in the emergency department (ED) setting and in young patients.
Due to the rarity and atypical presentations of AoD, particularly in young individuals, early diagnosis remains a challenge in the ED. We believe that, to identify these characteristics, a contrast-enhanced computed tomography (CECT) should be applied with a low threshold to facilitate an early diagnosis and timely treatment. In this study, we attempted to identify the characteristics of acute AoD among young individuals as well as the difference between Marfan syndrome and non-Marfan syndrome patients.
This was a retrospective study at a 1,600-bed tertiary teaching hospital with an average annual ED volume of 84,000 patients. The hospital database was queried for the combination of a discharge diagnosis of AoD and age less than 40 years between January 1995 and December 2004. Acute type A AoD was defined as any dissection that involved the ascending aorta with presentation within 14 days of symptom onset. Type B AoD was defined as any in which the dissection did not involve the ascending aorta.6 Traumatic AoD was excluded from this study. The medical charts were reviewed to obtain demographic data, clinical data and laboratory characteristics. Each chart was reviewed by 1 of the 5 authors, and the data were abstracted using a standardized data collection sheet. Because the study involved only the review of records obtained as a part of routine medical care, no patient consent was required. The presence of typical risk factors for acute AoD, including hypertension, hyperlipidemia, smoking, connective tissue diseases, congenital heart diseases, and previous cardiac surgery were determined. Variables including presenting symptoms, blood pressure (BP) upon arrival of ED, presumed risk factors for AD, triggering events, hemoglobin level, in-hospital diagnosis, types of AoD, organ involvement, diagnostic modalities, treatment modalities (emergent surgical reconstruction or conservative treatment) and outcomes were collected.
The diagnosis of Marfan syndrome involves 6 organ systems, including skeletal, ocular, cardiovascular, dura, pulmonary and skin/integument system, as well as family/genetic history with corresponding major and minor criteria. For the index case, in the absence of significant family history, at least 2 major criteria in different organ systems and involvement of a third organ system, or 1 major criterion in an organ system and involvement of a second organ system, if an fibrillin (FBN) 1 gene mutation was previously confirmed to cause Marfan syndrome, were required to diagnose Marfan syndrome. For a relative of an index case, only the presence of a major criterion in the family/genetic history category and 1 major criterion in an organ system and involvement of a second organ were required.7,8 The clinical impression or suspicion of Marfan syndrome (Marfanoid habitus) was determined by the referral primary care physicians, ED physicians, consulting cardiovascular surgeons or internists who cared for these patients according to the family history or physical findings and documented their concern in their preliminary diagnosis. The diagnosis of Marfan syndrome was confirmed after formally consulting with a sub-specialist or medical geneticist who was experienced in making the diagnosis of Marfan syndrome. The diagnosis of other congenital cardiac abnormalities was confirmed by cardiologists through appropriate diagnostic modalities, including 2-dimentional echocardiography or cardiac catheterizations. A comparison between Marfan syndrome and non-Marfan syndrome patients was performed.
All continuous variables are presented as means ± standard deviation (SD). Categorical variables were compared by using the Chi-square test or Fisher's exact test. Statistical significance was defined as a p value of less than 0.05.
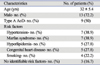
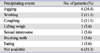
Three hundred and forty-four consecutive patients were found to have acute AoD as the primary discharge diagnosis during the study period. Eighteen (5.2%) of them presented acute AoD under the age of 40 years. The associated clinical presentations, risk factors and outcomes of these 18 patients are presented in Table 1. Nine patients had type A and another 9 patients had type B AoD. Seven patients (38.9%) had chest pain and/or tightness, 5 (27.8%) had chest-back pain, 2 (11.1%) had epigastric pain, 2 (11.1%) had back pain, 2 (11.1%) had lower limbs weakness or numbness, 1 (5.6%) had abdominal pain and 1 (5.6%) presented with sudden cardiac arrest. Previous or congenital heart disease included mitral valve prolapse (MVP), atrial septal defect (ASD), aortic regurgitation, aortic dissection and dilated aortic root. Pulse or BP differentials were present in 6 patients (33.3%). Suggestive signs of AoD in the initial chest radiography were present in only 6 patients (33.3%). Nearly all patients (94.4%) ultimately required more than 2 diagnostic modalities for appropriate diagnosis. The demographic data of these 18 patients are shown in Table 2. The mean age of these 18 patients was 32 ± 5.4 years. The mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) upon arrival at the ED was 153 ± 54.8 and 84 ± 39.5 mmHg, respectively (median SBP: 166; median DBP: 85 mmHg). Ten patients had a SBP greater than 160 mmHg and 3 featured a SBP less than 100 mmHg. Seven patients (38.9%) had history of hypertension. Seven patients (38.9%) were found to have Marfan syndrome. Five patients (27.8%) had history of hyperlipidemia. Three patients demonstrated no relevant risk factors for the development of AoD. The triggering events are shown in Table 3. The precipitating events could not be obtained in 6 patients (33.3%). Twelve patients (66.7%), including all patients with type A AoD (9) and 3 patients with type B AoD who had end organ involvement underwent emergent surgical reconstruction. The mean follow-up time was 4.78 ± 2.98 years, and 6 patients (33.3%) suffered recurrences of AoD. The mortality rate was 24.4%.
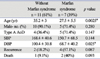
Comparison between patients with and without Marfan syndrome is shown in Table 4. Patients with Marfan syndrome developed acute AoD at younger age than patients without Marfan syndrome (27.5 ± 5.5 vs. 35.2 ± 3 years, p = 0.0025). The mean DBP upon presenting to the ED was significantly lower in patients with Marfan syndrome than those without (68.7 ± 40.2 vs. 100.4 ± 30.8 mmHg, p = 0.025), while SBP in these 2 groups had no statistical difference (150.7 ± 68.52 vs. 168.4 ± 40.6 mmHg, p = 0.144). Patients with Marfan syndrome had higher trends toward type A AoD (36.4% vs. 71.4%, p = 0.147), increased recurrence rate (18.2 % vs. 57.1%, p = 0.087) and higher mortality rate (9% vs. 40%, p = 0.093) than those without. However, the statistical significance was not attained for all such comparisons.
Fourteen individuals (77.8%) were diagnosed with AoD in the ED, while the remaining 4 were diagnosed subsequently. The clinical scenarios for these 4 patients (patients No. 1, 9, 15 and 16) are discussed in brief. Patient No. 15 presented with acute coronary syndrome (ACS). A 12-lead electrocardiogram (ECG) revealed ST elevation in Lead II, III, and aVF and reciprocal changes in I and aVL, as well ST elevation in the rV4 (arrow) and high degree atrioventricular (AV) block (Fig. 1), consistent with acute inferio-posterior wall myocardial infarction. The diagnosis was not made until a coronary angiogram and aortogram revealed AoD involving the right coronary artery. Patient No. 16 presented with sudden cardiac arrest following several bouts of forceful coughing. She recovered spontaneous circulation after 10 minutes of resuscitation. A bedside transthoracic echocardiography (TTE) demonstrated moderate pericardial effusion, aortic regurgitation and presence of false lumen with spontaneous contrast enhancement. She received a successful emergent aorta reconstruction. However, she developed hypoxic encephalopathy and multiple organ dysfunction, and died on the 21st hospital day. Patients No. 1 and No. 9 were admitted due to abdominal and epigastric pain, respectively. The combination of Marfanoid features, unresolved pain and pulse/blood pressure (BP) differentials led to further diagnostic procedures including CECT and/or transesophageal echocardiography (TEE), and the diagnosis of AoD was eventually established.
Our study demonstrated that young population (less than 40 years) constituted only a minor proportion (5.2%) of patients suffering from AoD. In a sub-study of International Registry of Aortic Dissection (IRAD) study that involved 951 acute AoD patients in 18 institutions between January 1996 and November 2001, only 68 patients (7%) were found to be younger than 40 years of age.5 The mortality rate (24.4%) of young patients who acquired AoD in our study was comparable to the corresponding results of IRAD studies (22%).9 The prevalence of Marfan syndrome in our study (38.9%) was lower than the corresponding prevalence of IRAD study (50%). Contrary to previous report, none of our 18 patients had bicuspid aortic valve which has been thought to be one of the most common congenital abnormalities associated with the occurrence of AoD.9 Pulse or BP differentials were present in 33% of young patients in our study, whereas von Kodolitsch et al.10 reported 38% of patients with AoD and considered to be specific signs of AoD.
Our finding is comparable with previous study that patients with Marfan syndrome tended to present with AoD at younger age and were not more hypertensive than those patients who had AoD but not Marfan syndrome.10 In addition, we found that acute AoD was developed at lower BP in patients with Marfan syndrome. The exact mechanisms are not obvious, however, we speculate that such a finding could be attributed to lower BP being required to initiate dissecting flap in patients with Marfan syndrome and once dissecting flap is developed, the propagation is more rapid, which causes more significant hemodynamic instability due to inherent collagen deficient in patients with Marfan syndrome than normal human subjects. Hypertension, either historical or at presentation, was less common in the young than in older AoD patients.5 Although most patients with AoD have hypertension at the time of presentation, an initial SBP < 100 mmHg has been reported in about 25% of AoD patients. Hypotension and shock in AoD patients can be caused by acute aortic regurgitation, aortic rupture, cardiac tamponade and left ventricular systolic dysfunction.11 Hypotension/shock, absence of chest/back pain on presentation and branch involvement have previously been identified to be associated with increased risk of in-hospital mortality in patients with type B AoD.12 Hypertension is more common in patients with distal dissection, whereas hypotension occurs mostly in proximal dissection.13,14 Although previous reports on the surgical management of AoD showed higher risk of developing type A AoD and a fatal outcome in patients with Marfan syndrome,15 our study failed to demonstrate statistical significance regarding the higher rate of type A AoD, increased recurrence and mortality rate in young patients with Marfan syndrome. A definitive diagnosis of Marfan syndrome may not be possible in the acute care setting when individuals are presenting with severe chest pain and shock. ED physicians should promptly recognize some physical features related to Marfan syndrome, including an upwardly displaced ocular lens, an "asthenic" body habitus due to general muscular underdevelopment and decreased subcutaneous fat, tall stature, unusually long arm span, arachnodactyly and pes planus, and pectus excavatum orcarinatum.16 The surveillance of aneurysm formation and timely surgical intervention might prevent the eventual occurrence of AoD in patients with Marfan syndrome. It is worth noting that 5 of the 7 patients with Marfan syndrome had known histories of a variety of previous heart diseases (sometimes leaving a surgical scar in their anterior chest wall, if the detailed histories were not readily available). Therefore, a screening diagnostic modalities such as CECT should be applied with lower threshold in such high-risk patients to facilitate an early diagnosis in the emergent setting.
Physical and mental activities can be triggers for many catastrophic diseases, including acute myocardial infarction or myocardial ischemia,18 and subarachnoid and intracerebral hemorrhage.17 Most AoD episodes are related to physical or mental stress, particularly for those episodes that occur during the day. AoD has been reported to be triggered by working, eating, drinking, defecation, urination, sports, housework, driving, walking, taking a bath, getting up from bed, dressing or undressing, brushing teeth, and numerous other examples of emotional stress.18 Anecdotal observations revealed weight lifting to be a triggering event of AoD.19-21 In addition, the use of cocaine or "crack" is an another association with AoD in young individuals.22 Hypertension and tachycardia induced by the pharmacologic effects of cocaine are speculated to be the causes of development and propagation of AoD.23 Our study identified that sexual intercourse and forceful coughing were two additional triggers for the onset of acute AoD in young patients. On reviewing medical literatures, we had found only one report regarding several forceful coughs due to choking as the trigger of acute AoD in a 65 year-old man.24 Intermittent forced respiratory maneuvers against airway resistance could be an afterload challenge to the left ventricle.25 Acute reduction in intrathoracic pressure distends the aorta, decreases the aortic strain, and increases the stiffness and shear stress of the aorta.26 We found no report regarding the association between sexual intercourse and the onset of acute AoD.
The classic suggestive signs in chest radiography of AoD have been reported to be present in up to 50 % of cases,27 nevertheless, only 33% of young patients had such findings. More than two thirds of patients required more than 2 imaging tests.28 Compared with using the older-model single-detector row helical CT scanners, the use of multi-detector row CT (MDCT) has led to dramatically increased speed and spatial resolution in aortic imaging. The sensitivity, specificity, positive and negative predictive value as well the accuracy for diagnosing aortic diseases were nearly 100%.29,30 Thus, MDCT is now considered the primary imaging modality when aortic dissection and/or other aortic disorders are suspected in the emergency setting. Exceptions to this standard arise when patient's instability, poor renal function, and/or allergy to iodinated contrast material prohibit the use of CT. We suggest the use of CECT with low threshold in young patients with a history of heart disease, hypertension, Marfan syndrome (Marfanoid habitus) to facilitate an early diagnosis. In addition, a CECT may also be beneficial in young patients presenting with acute coronary syndrome, unexplained abdominal symptoms, and sudden cardiac arrest, if the clinical situation is suitable.
Our study had several limitations. As it was retrospective, some clinical manifestations could not be traced, such as the triggering events. The sample size was too small to conclude whether Marfan syndrome was associated with an increased adverse outcome in young patients suffering from AoD. A prospective study is required to validate the difference between these 2 groups. The presence of undiagnosed patients might reasonably be expected in patients with out-of-hospital cardiac arrest. The evaluations of pathologic findings such as the presence of cystic medial necrosis or atherosclerotic plaque were not included in our study. The usefulness of serologic collagen turnover markers, such as matrix metalloproteinases and their tissue inhibitors as well as d-dimer assay in early diagnosis or exclusion of AoD in the ED setting can be incorporated in future studies.31
In conclusion, despite advances in the accuracy of diagnostic imaging modalities, a high clinical suspicion remains the most important factor in recognizing AoD and it holds to be true in young patients. Although AoD is rare in individuals younger than 40 years of age, ED physicians should have high alert to acute AoD in young patients presenting with severe unexplained chest and back pain, particularly in those patients with a history of heart diseases, hypertension, and Marfan syndrome or featuring Marfanoid habitus. even if BP is not markedly high. In susceptible young individuals, forceful coughing and sexual intercourse could be triggers of AoD. Acute coronary syndrome, unexplained abdominal symptoms, and sudden cardiac arrest could be the initial manifestation of AoD in young patients. A low threshold for CECT may be appropriate in young patients in order to facilitate an early diagnosis and timely treatment.
Figures and Tables
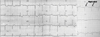 | Fig. 1Twelve-lead electrocardiography of patient No. 12 obtained in the emergency department. Note ST elevation in Lead II, III, aVF, reciprocal changes in I and aVL, and ST elevation in the rV4 (arrow) as well as high degree of AV block, findings consistent with acute inferio-posterior wall myocardial infarction. |
Table 1
Patients' Characteristics, Laboratory Findings, Diagnostic Modalities and Outcomes (n = 18)

Abdo pain, abdominal pain; HTN, hypertension; Hyperlipid, hyperlipidemia; S, smoking; MVP, mitral valve prolapse; AoD, aortic dissection; N/A, not available; C×R, chest radiography; CT, computed tomography; MRI, magnetic resonance imaging; TEE, transesophageal echocardiography; TTE, transthoracic echocardiography; MR, magnetic resonance imaging; MODS, multiple organ dysfunction syndrome; AR, aortic regurgitation, AMI, acute myocardial infarction; R, recurrence; D, death.
ACKNOWLEDGEMENTS
This study was supported by a grant from the Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan.
References
1. Blanchard DG, Kimura BJ, Dittrich HC, DeMaria AN. Transesophageal echocardiography of the aorta. JAMA. 1994. 272:546–551.

3. Fann JI, Smith JA, Miller DC, Mitchell RS, Moore KA, Grunkemeier G, et al. Surgical management of aortic dissection during a 30-year period. Circulation. 1995. 92(9):Suppl. II113–II121.

4. Meszaros I, Mórocz J, Szlávi J, Schmidt J, Tornóci L, Nagy L, et al. Epidemiology and clinicopathology of aortic dissection. Chest. 2000. 117:1271–1278.

5. Fikar CR, Koch S. Etiologic factors of acute aortic dissection in children and young adults. Clin Pediatr (Phila). 2000. 39:71–80.

6. Daily PO, Trueblood HW, Stinson EB, Wuerflein RD, Shumway NE. Management of acute aortic dissections. Ann Thorac Surg. 1970. 10:237–247.

7. De Paepe A, Devereux RB, Dietz HC, Hennekam RC, Pyeritz RE. Revised diagnostic criteria for the Marfan syndrome. Am J Med Genet. 1996. 62:417–426.

8. Summers KM, West JA, Peterson MM, Stark D, McGill JJ, West MJ. Challenges in the diagnosis of Marfan syndrome. Med J Aust. 2006. 184:627–631.

9. Januzzi JL, Isselbacher EM, Fattori R, Cooper JV, Smith DE, Fang J, et al. Characterizing the young patients with aortic dissection: results from the International Registry of Aortic Dissection (IRAD). J Am Coll Cardiol. 2004. 43:665–669.

10. Januzzi JL, Marayati F, Mehta RH, Cooper JV, O'Gara PT, Sechtem U, et al. Comparison of aortic dissection in patients with and without Marfan's syndrome (results from the International Registry of Aortic Dissection). Am J Cardiol. 2004. 94:400–402.

11. Khan IA, Nair CK. Clinical, diagnostic, and management perspectives of aortic dissection. Chest. 2002. 122:311–328.

12. Suzuki T, Mehta RH, Ince H, Nagai R, Sakomura Y, Weber F, et al. Clinical profiles and outcomes of acute type B aortic dissection in the current era: lessons from the International Registry of Aortic Dissection (IRAD). Circulation. 2003. 108:suppl 1. II312–II317.

14. Spittell PC, Spittell JA Jr, Joyce JW, Tajik AJ, Edwards WD, Schaff HV, et al. Clinical features and differential diagnosis of aortic dissection: experience with 236 cases (1980 through 1990). Mayo Clin Proc. 1993. 68:642–651.

15. Smith JA, Fann JI, Miller DC, Moore KA, DeAnda A Jr, Mitchell RS, et al. Surgical management of aortic dissection in patients with the Marfan syndrome. Circulation. 1994. 90:II235–II242.
16. Ramires F, Godfrey M, Lee B, Tsipouras P. Scriver CR, Beaudet AI, Sly WS, Valle D, editors. Marfan syndrome and related disorders. The metabolic and molecular bases of inherited disease. 1995. Volume 3:7th ed. New York: McGraw Hill;4079–4094.
17. Tsementzis SA, Gill JS, Hitchcock ER, Gill SK, Beevers DG. Diurnal variation of and activity during the onset of stroke. Neurosurgery. 1985. 17:901–904.

18. Kojima S, Sumiyoshi M, Nakata Y, Daida H. Triggers and circadian distribution of the onset of acute aortic dissection. Circ J. 2002. 66:232–235.

19. Gwan-Nulla DN, Davidson WR Jr, Grenko RT, Damiano RJ Jr. Aortic dissection in a weight lifter with nodular fasciitis of the aorta. Ann Thorac Surg. 2000. 69:1931–1932.

20. de Virgilio C, Nelson RJ, Milliken J, Snyder R, Chiang F, MacDonald WD, et al. Ascending aortic dissection in weight lifters with cystic medial degeneration. Ann Thorac Surg. 1990. 49:638–642.

21. Baumgartner FJ, Omari BO, Robertson JM. Weight lifting, Marfan's syndrome, and acute aortic dissection. Ann Thorac Surg. 1997. 64:1871–1872.
22. Rashid J, Eisenberg MJ, Topol EJ. Cocaine-induced aortic dissection. Am Heart J. 1996. 132:1301–1304.

23. Li W, Su J, Sehgal S, Altura BT, Altura BM. Cocaine-induced relaxation of isolated rat aortic rings and mechanisms of action: possible relation to cocaine-induced aortic dissection and hypotension. Eur J Pharmacol. 2004. 496:151–158.

24. Papadimos TJ, Hofmann JP. Aortic dissection after forceful coughing. Anaesthesia. 2006. 61:71–72.

25. Buda AJ, Pinsky MR, Ingels NB Jr, Daughters GT 2nd, Stinson EB, Alderman EL. Effect of intrathoracic pressure on left ventricular performance. N Engl J Med. 1979. 301:453–459.

26. Virolainen J, Kupari M. Age-dependent increase in aortic stiffness during negative intrathoracic pressure in healthy subjects. Am J Cardiol. 1993. 71:878–882.

27. Jagannath AS, Sos TA, Lockhart SH, Saddekni S, Sniderman KW. Aortic dissection: a statistical analysis of the usefulness of plain chest radiographic findings. AJR Am J Roentgenol. 1986. 147:1123–1126.

28. Moore AG, Eagle KA, Bruckman D, Moon BS, Malouf JF, Fattori R, et al. Choice of computed tomography, transesophageal echocardiography, magnetic resonance imaging, and aortography in acute aortic dissection: International Registry of Acute Aortic Dissection (IRAD). Am J Cardiol. 2002. 89:1235–1238.

29. Hayter RG, Rhea JT, Small A, Tafazoli FS, Novelline RA. Suspected aortic dissection and other aortic disorders: multi-detector row CT in 373 cases in the emergency setting. Radiology. 2006. 238:841–852.

30. Yoshida S, Akiba H, Tamakawa M, Yama N, Hareyama M, Morishita K, et al. Thoracic involvement of type A aortic dissection and intramural hematoma: diagnostic accuracy--comparison of emergency helical CT and surgical findings. Radiology. 2003. 228:430–435.

31. Akutsu K, Sato N, Yamamoto T, Morita N, Takagi H, Fujita N, et al. A rapid bedside D-dimer assay (cardiac D-dimer) for screening of clinically suspected acute aortic dissection. Circ J. 2005. 69:397–403.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download