Abstract
Purpose
This single-institution retrospective review examines the management of uninfected para-anastomotic aneurysms of the abdominal aorta (PAAA), developed after infrarenal grafting.
Materials and Methods
From October 1979 to November 2005, 31 PAAA were observed in our Department. Twenty-six uninfected PAAA of degenerative etiology, including 24 false and 2 true aneurysms, were candidates for intervention and retrospectively included in our database for management and outcome evaluation. Six (23%) patients were treated as emergencies. Surgery included tube graft interposition (n = 12), new reconstruction (n = 8), and graft removal with extra-anatomic bypass (n = 3). Endovascular management (n = 3) consisted of free-flow tube endografts.
Results
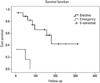
The mortality rate among the elective and emergency cases was 5% and 66.6%, respectively (p = 0.005). The morbidity rate in elective cases was 57.8%, whereas 75% in emergency cases (p = 0.99). The survival rate during the follow-up was significantly higher for elective cases than for emergency cases.
Conclusion
Uninfected PAAA is a late complication of aortic grafting, tends to evolve silently and is difficult to diagnose. The prevalence is underestimated and increases with time since surgery. The mortality rate is higher among patients treated as an emergency than among patients who undergo elective surgery, therefore, elective treatment and aggressive management in the case of pseudoaneurysm are the keys to obtain a good outcome. Endovascular treatment could reduce mortality. Patients who undergo infrarenal aortic grafting require life-long surveillance after surgery.
Para-anastomotic aneurysm of the abdominal aorta (PAAA) is a major complication of infrarenal grafting performed for occlusive disease or aneurysm,1,2 and involves the sutureline with disruption of the anastomosis. PAAA may be related to infection of the graft or caused by a sterile degenerative process involving the anastomosis. It is rare for a PAAA to be diagnosed within 5 years after aortic grafting (1-6%),3-11 and such cases are generally associated with an infection of the graft; the uninfected degenerative form of PAAA is usually observed 8-10 years after primary aortic surgery.
We focused our attention on uninfected PAAA because such aneurysms are secondary to a slow, degenerative process acting silently at the anastomosis, apparently not influenced by any external factors, and responsible for late failure of aortic reconstructions with life-threatening clinical consequences.11 A PAAA may present as a true aneurysm of the aortic remnant near the anastomosis, or as a false aneurysm (anastomotic aneurysm) of the suture-line,5,9-11 and both are potentially responsible for thrombosis, distal embolization, compression/erosion of adjacent organs, and inexorable growth to the point of rupture.4,6,10
Their deep location makes PAAA difficult to detect without imaging and, despite the high levels of sensitivity and specificity of diagnostic techniques now available, true and false PAAA often cannot clearly be distinguished. Furthermore, the follow-ups scheduled by most Departments of Vascular Surgery to check aortic grafts are not continued for long enough period, considering the time at which uninfected PAAA usually develops.7 For these reasons, the real frequency of uninfected PAAA is difficult to determine. Based on the limited data available in the literature, the overall incidence appears to range from 0.2% to 15%,9-12 however, this is probably an underestimate because of no long-term, standardized follow-ups that could reveal a higher frequency than that so far reported. One further problem is that many of the published epidemiological data have been derived from heterogeneous populations of patients with no distinctions concerning the etiology or site of the disrupted anastomoses.
Prospective analyses10,13,14 estimated that the incidence of late, uninfected anastomotic complications ranges from 22.8% to 35.8% at 15 years after infrarenal grafting. Such results can not certainly be neglible, and raise doubts about the long-term durability of what has always been considered the most successful and gratifying intervention by vascular surgeons.
Once diagnosed, the management of uninfected PAAA is extremely challenging both in elective and emergency conditions, and the outcome appears to be influenced more by technical surgical variables than by the patients' clinical background.6,9 The high morbidity and mortality rates reported in the literature, particularly following surgery performed as an emergency, bear witness to the clinical relevance of this complication and the importance of an early diagnosis in order to manage it in elective conditions.6
The aim of this single-institution study was to review the management of uninfected PAAA in our Department, focusing on perioperative outcomes and long-term survival.
All the infrarenal aortic prosthetic reconstructions performed in our Institution between October 1979 and November 2006 were identified from the prospective patients' registry, and a retrospective review of patients' clinical records was used to create a database containing information on all the cases of PAAA observed, including anatomical and etiopathogenetic details of the PAAA based on the results of clinical and imaging evaluations. Infected PAAA were excluded.
Pre-operative medical risk factors, intra-operative variables, and post-operative outcomes were analyzed for uninfected degenerative PAAA only. Pre-operative risk factors were recorded according to the American Society of Anesthesiologists (ASA) physical status classification after evaluation of cardiopulmonary and renal function. These data together with indications for the operation and type of treatment allowed to calculate the risk/benefit ratio and identification of patients unfit for an intervention. All complicated, life-threatening PAAA, were treated as emergencies without evaluation of pre-operative risk factors. Operative variables recorded included the form (elective or emergency) and type (surgical or endovascular) of the intervention, type of surgical reconstruction, and anatomical location of the aortic control. Post-operative outcomes included in-hospital morbidity and mortality: in-hospital mortality was defined as a peri-operative death occurring during the same admission regardless of the duration of the hospital stay; in-hospital morbidity included cardiac, pulmonary, neurological, gastrointestinal, visceral ischemic, peripheral ischemic, systemic, and wound complications occurring during the same hospital admission. Long-term survival of more recent cases was assessed by direct clinical evaluation, and by telephone contact for older ones.
The primary end-point for analysis was perioperative outcome, and the secondary end-point was long-term survival. Demographic data, pre-operative medical risk factors, and perioperative variables were analyzed descriptively. Mortality and morbidity rates were considered separately for the overall population of patients with uninfected PAAA, and the subgroups were treated electively or as an emergency and those managed surgically or with an endovascular intervention. Fisher's exact test was used to compare the results of patients treated electively or as an emergency and those undergoing surgery or endovascular treatment (two-tailed level of significance α = 0.05). The patients who were managed surgically underwent physical examination after 2 months and subsequently once yearly; data from these examinations were combined with those from ultrasonography when diagnostic echo-studies became widely available in clinical practice; angio-computed tomography (angio-CT) was performed only if abnormalities were suspected at ultrasonography and routinely after 5 years. Patients managed with an endovascular procedure underwent angio-CT after 2, 6, and 12 months and then yearly. The patients' survival was assessed using Kaplan-Meier product-limit estimates (SPSS 13.0, Chicago, IL, USA). p values < 0.05 were considered statistically significant.
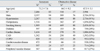
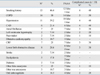
From October 1979 to November 2005, 2,996 infrarenal prosthetic reconstructions for aneurysmal and obstructive aortoiliac disease were performed in our Department. The demographics of the population who underwent these reconstructions are presented in Table 1.
During the same period, 31 patients with PAAA were observed. Seventeen patients (55%) had had their primary graft in our Department, whereas 14 patients (45%) were treated at another Institution. All patients underwent clinical, biochemical, and microbiological examinations along with imaging studies in order to obtain a precise diagnosis and define the etiology and morphology of the PAAA. The type of imaging study (thoraco-abdominal angio-CT, abdominal color Doppler ultrasound, aortography) varied over time because of technological evolutions that occurred during the 26-year period covered in this study.
Four of the 31 patients with an identified PAAA had graft infection combined with disruption of the proximal aortic anastomosis and formation of a pseudoaneurysm. The remaining 27 patients had uninfected PAAA, as determined by clinical evaluation, laboratory examinations, microbiological analyses and imaging, thereby excluding an infective etiology, and anastomotic failure was the result of a degenerative process.
All patients in whom an uninfected PAAA was detected in non-emergency conditions underwent preoperative assessment of cardiac, pulmonary, renal function (color Doppler echocardiography, coronarography, spirometry, and serum creatinine levels), and comorbid conditions in order to stratify the operative risk according to the ASA criteria. For patients presenting as an emergency, there was usually not enough time for a pre-operative assessment, except for that strictly related to the diagnosis of PAAA. Emergency cases underwent immediate treatment, whereas for patients whose PAAA was detected in non-emergency conditions the indication to treat was discussed considering the ASA score, the diameter of the PAAA and the risk related to technical-surgical variables, in order to define a benefit/risk ratio.
Our database of patients with uninfected PAAA included information on 25 (92.6%) men and 2 women. The mean age of these patients was 70 years (range, 47 to 87 years), whereas the mean age at the time of primary surgery was 58 years. The mean interval from primary surgery to the diagnosis of PAAA was 10.1 years (range, 0.25-21 years).
The indication for primary grafting was aneurysm in 18 patients and occlusive disease in 9 patients. The patients' comorbidities and risk factors are listed in Table 2.
After careful preoperative evaluation, 25 patients - with 26 uninfected PAAA - underwent intervention: 24 (92.3%) with pseudoaneurysms - 23 proximal, 1 distal - and 2 with true aneurysms. Two proximal false PAAAs were associated with Crawford's type 4 thoraco-abdominal aortic aneurysm (TAA), and no other thoracic aortic aneurysm recurrence was diagnosed in the population treated. In one patient, a false PAAA recurred twice at the same anastomotic line. Two asymptomatic patients were considered unfit for intervention: 1 was an 83-year-old man with a proximal pseudoaneurysm and type 3 TAA 90 mm in diameter, who had a ventriculoperitoneal drainage for a hydrocele. He was permanently confined to bed because of a spinal cord disease, and had severe chronic obstructive pulmonary disease and cardiac dysfunction. The other patient was an 87-year-old man with a proximal pseudoaneurysm of 42 mm in diameter who had severe chronic obstructive pulmonary disease, mild-to-severe renal impairment and extreme cardiac dysfunction (ejection fraction 18% at echocardiography).
Among the patients with a false PAAA, the disrupted anastomosis was end-to-side in 9 cases and end-to-end in the other 15 (62.5%) cases. In the 2 patients with true PAAA, the disrupted anastomosis was end-to-end in one and end-to-side in the other. The mean diameter of the true PAAA was 50 mm (range, 48-52 mm) whereas that of the false PAAA was 46.25 mm (range, 34-80 mm). The mean diameter of the PAAA treated as emergencies because of rupture or aorto-enteric fistula (AEF) was 45 mm (range, 34-53 mm).
On admission to the hospital, patients with true PAAA were asymptomatic and free of complications. Thirteen (50%) of the patients with false PAAA had acute or subacute non-specific symptoms, including abdominal pain, gastrointestinal bleeding, lower limb ischemia, asthenia and back pain with sciatica.
In the subgroup of false PAAA, 10 (41.6%) cases were complicated by thrombosis of the aneurysm and lower limb ischemia (n = 1), asymptomatic fissuration diagnosed intraoperatively (n = 2), asymptomatic tamponated rupture in mesocolon (n = 1), retroperitoneal rupture (n = 2) and secondary AEF with upper gastrointestinal bleeding (n = 4). True secondary AEF in the third part of the duodenum was observed in 2 cases of ruptured PAAA, whereas a paraprosthetic secondary AEF with duodeno-ileal perforation over an integral pulsating PAAA capsule was detected in another 2 cases.
Clinical examination was negative in 9 cases (35%), whereas a pulsating abdominal mass was palpable in 17 cases (65%).
Ultrasonography was diagnostic in 4 of the 9 false PAAA in which this examination was used and the aortic dilatation was detected without defining its extension. Angio-CT was diagnostic in all the cases in which it was applied and the extent of the PAAA and the involvement of visceral arteries were determined. Aortography was diagnostic in 16 (80%) of 20 cases (19 pseudoaneurysms and 1 true aneurysm). Esophagogastroduodenoscopy was performed in 3 cases of hematemesis of duodenal origin, but failed to detect fistulae. One false PAAA was diagnosed during an explorative laparotomy.
In the subgroup of patients treated surgically, no infective foci were found during intra-operative exploration. Samples of the grafts removed were microbiologically and histologically examined, which confirmed the lack of bacterial contamination and demonstrated the degenerative etiopathogenesis.
AEF is potentially responsible for suture-line infection from the bowel. The absence of infective features might be explained by the fact that the true AEF after PAAA rupture (n = 2) developed so acutely that there was no time for contamination of the anastomosis to occur, whereas the integrity of the false PAAA fibrous capsule probably protected the aortic suture-line from infection in paraprosthetic AEF (n = 2). Furthermore, the bacterial load of the duodenum is low compared to that of other parts of the intestine.
Twenty cases (77%) - 2 true and 18 false PAAA - were treated electively, whereas 6 symptomatic and life-threatening complicated false PAAA were treated in emergency. Table 3 summarizes the presentation and management of the cases of PAAA.
Surgery was performed in 23 cases (88%). The transabdominal approach allowed good exposure of the entire abdominal aorta in 21 cases (20 false and 1 true PAAA). Aortic control was safely obtained below or close to renal arteries, except in 6 cases which required suprarenal clamping below the mesenteric vessels because of difficulties in the surgical approach to the juxtarenal aorta and PAAA. The thoracoabdominal approach was required for 2 false PAAA associated with type 4 TAA.
Ten cases of false PAAA were treated by in situ Dacron reconstruction with tube graft interposition between the aorta and the distal portion of the old graft; 7 cases of false PAAA and 1 true PAAA were managed by complete removal of the old graft and new reconstruction; thoraco-abdominal endo-aneurysmectomy and tube graft interposition between the thoracic aorta and old graft with reimplantation of visceral arteries was performed in two cases of false PAAA with type 4 TAA. Extra-anatomic axillofemoral bypass with reinforced expanded PolyTetraFluorEthilene (ePTFE) combined with complete graft removal and closure of the aortic stump was the management chosen for 3 cases of PAAA, in order to avoid as much as possible technical risks related to in situ reconstruction in the site of a damaged, malacic aorta or when there was a suspicion of bacterial contamination from the duodenal lumen at the onset of AEF.
Endovascular treatment was performed electively in 3 uncomplicated cases (2 proximal false PAAA and 1 proximal true PAAA after end-to-end anastomosis) in the operating room, after surgical exposure of the femoral arteries under epidural anesthesia. Angio-CT scanning and complementary aortography documented proximal infrarenal necks shorter than 15 mm, so free-flow tube endografts (Endologix Powerlink Bard®) were required to achieve safe exclusion of the aneurysm without impairing renal vessels.
Five patients, all treated surgically, died in hospital giving an in-hospital mortality rate of 19.2% in the whole series and 21.7% in the surgical subgroup. No deaths occurred in the endovascular subgroup. The mortality rate was 5% among patients treated electively and 66.6% in emergency cases (p = 0.005, 2-tailed Fisher's exact test). The mortality rate among patients who underwent localized and extensive surgical interventions was 0% and 50%, respectively (p = 0.09, two-tailed Fisher's exact test). The mortality rate in cases of symptomatic PAAA was 30.7%, whereas it was 7.7% in asymptomatic cases (p = 0.32, two-tailed Fisher's exact test). One patient with a false PAAA and type 4 TAA died during an elective intervention from consumption coagulopathy after severe aortic bleeding. Four patients treated as emergencies died in the post-operative period: 2 from compromised hemodynamics and coagulopathy the first day after surgery for ruptured false PAAA; 1 patient died from massive bowel infarction 8 days after surgery for false PAAA and secondary AEF; and 1 died from acute massive duodenal bleeding and perforation 29 days after surgery for false PAAA complicated by gastrointestinal bleeding.
The overall morbidity rate was 66.5%; 57.8% in electively managed cases and 75% in emergency cases (p = 0.99, 2-tailed Fisher's exact test). The morbidity rate in symptomatic cases was 63.6%, whereas it was 50% in the asymptomatic group (p = 0.68, two-tailed Fisher's exact test). Major and minor complications observed are summarized in Table 4. Only minor complications were noted in the endovascular subgroup, and their relationship with the procedure appeared very weak.
Technical difficulties were recorded in 21 cases of redosurgery: omental and bowel adhesions to PAAA with or without AEF (n = 12); challenging preparation of the aorta, PAAA and renal arteries due to intense fibrosis (n = 5); ligature of the left renal vein to gain the aortic clamp-site (n = 2); iatrogenic duodeno-ileal damage (n = 3); retroperitoneal/ abdominal bleeding after PAAA rupture or consumption coagulopathy (n = 4); intra-operative rupture of the aneurysm during preparation of the aorta (n = 1).
A stay in the Intensive Care Unit (ICU) was required in 41.6% of cases for a mean period of 2.5 days (range, 1-8 days). None of the patients in the endovascular subgroup needed ICU management. Survivors were discharged from hospital after a mean period of 12.2 days (range, 4-27 days); 14.3 and 4.3 days for the surgical and endovascular subgroups, respectively.
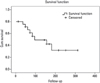
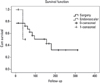
Follow-up data are available for all the patients. Kaplan-Meier product-limit survival estimates are depicted in Figs. 1, 2 and 3. With a median follow-up of 105.6 months (range, 12-312 months), the 10-year survival was 50% for the overall population of patients with uninfected PAAA who underwent an intervention (Fig. 1). There was a significant difference in mid- to long-term survival between elective and emergency cases, as depicted in Fig. 2. Eight patients died of causes unrelated to the PAAA treatment. There were no cases of graft infection or late lower limb amputations. No graft complications were observed in the surgical subgroup except for that of the patient who experienced recurrent false PAAA. Three patients underwent interventions for disease of other vascular districts. One pseudoaneurysm treated with an endograft developed a proximal type I endoleak, detected by angio-CT 2 months after the procedure: an aortic cuff with effective exclusion of the aneurysm was deployed in this patient. Exclusion of the aneurysm was maintained in the other 2 cases in which endovascular management was used without signs of stent-graft migration or failed fixation to the inner surface of the old grafts.
The 2 patients considered unfit for intervention died; one after rupture of a type 3 TAA and the other of cardiac failure and uremia.
Uninfected PAAA is a late major complication of infrarenal aortic grafting. Discontinuity of the anastomosis causes a false PAAA that usually occurs as a result of arterial wall disruption and mechanical stress4,7,9,13-20 rather than because of graft/suture material failure.21 Aorta versus graft compliance/diameter mismatch9,10,13,14 and extreme mechanical stress (greater in end-to-side rather than end-to-end anastomoses) at the suture-line play major pathogenetic roles.4,10,19-24 Hypertension,4,25 atherosclerosis, and previous aortic endarterectomy4 are important in suture-line failure.24 Major peri-operative complications, technical errors, recurrent aneurysm and α1-antitrypsin deficiency may be associated with an early onset of pseudoaneurysm.9-11
True PAAA usually occurs after surgery performed for an aneurysm rather than for occlusive disease, and is a progression of the aortic dilatation:5,10,25-28 it may affect the infrarenal aorta as a consequence of inadequate resection of the primary aneurysm, particularly when treated as an emergency for rupture,29,30 or it involves the pararenal and/or suprarenal aorta proximally to a graft placed just below the renal arteries as a consequence of progressive atherosclerosis.9,23,28 The incidence of false PAAA is 2 to 3 times higher than that of true PAAA.7,9,10,15
Uninfected PAAA is, however, an underestimated complication.7,9,18,31,32 Table 5 summarizes the reported incidences of PAAA in different series. There is a tendency to define PAAA as an infrequent event, but there is a clear lack of uniformity of data, therefore, a precise epidemiological evaluation of the phenomenon is not possible.11 The real dimensions of this complication are probably misunderstood7,9,18 because of the heterogeneous attention paid to PAAA by Departments of Vascular Surgery, the lack of long-term follow-ups after aortic grafting, diagnostic difficulties (PAAA evolves silently for a long time and manifests with non-specific symptoms and no signs because of its retroperitoneal location), and the different diagnostic methods used during follow-up.3,6,7,9,10 The significant number of PAAA (45% in our survey) observed in Institutions different from those in which the primary aortic reconstructions were performed confirms that it is difficult to achieve long-term follow-up after aortic grafting by many Vascular Departments.18,32 In our own experience, we diagnosed PAAA in 17 patients from a population of 2,996 who underwent infrarenal reconstructions, resulting in an incidence of 0.57% PAAA. We consider this an underestimate, because we were not able to follow-up all the patients over the 26-year period and we cannot be sure how many developed late anastomotic complications that were eventually diagnosed and treated at other Departments of Vascular Surgery.
Prospective analyses10,13,14 underline how the incidence of PAAA increases significantly with time elapsed since the primary graft, so that the patient's long life-expectancy is a risk factor for future development of sterile PAAA.3,4 Using life-table analysis, Edwards et al.10 estimated that the overall incidence of PAAA after 8 and 15 years was 5% and 27%, respectively, and that the incidence of false PAAA was 1% and 20%, respectively. They also estimated that the incidence of true/recurrent PAAA was 4% and 9% after 10 and 25 years, respectively. Van den Akker et al.,13 who also used life-table analysis, calculated that the chance of being free of an anastomotic aneurysm at any site was 77.2% at 15 years after the primary operation. By applying the Kaplan-Meier method, Mii et al.14 estimated overall incidences of PAAA of 0.8%, 6.2% and 35.8% after 5, 10 and 15 years, respectively.
PAAAs are challenging for surgeons because of the technical difficulties, which are caused by intense para-aortic fibrosis, encountered during surgical preparation of the aorta near the PAAA, which increase the risk of both iatrogenic damage to vessels and organs and peri-operative complications. Technical aspects and surgical variables are, therefore, crucial in determining a patient's operative risk.6 Moreover, patients with PAAA are 8-10 years older than at the time of the primary graft and their co-morbidities (particularly cardiac and pulmonary) are expected to be worse.6 These factors contribute to making the operative risk for PAAA higher than that for primary aortic surgery, which is strictly related to co-morbidities.
It is clear that a ruptured or seriously complicated PAAA increases the operative risk, therefore, emergency treatment is associated with a higher surgical risk than elective management. In agreement with reports in the literature (Table 6), there was a very high mortality rate (66.6%) in the subgroup of our patients treated as emergencies, whereas the mortality rate was only 5% in the electively treated subgroup (p = 0.005, two-tailed Fisher's exact test). On the other hand, we found no significant differences in early post-operative morbidity rates between elective and emergency cases. Furthermore, no significant differences were found in mortality rates between patients undergoing localized and extensive surgery (p = 0.09, 2-tailed Fisher's exact test). In conclusion, elective surgery of an uninfected PAAA carries a higher operative risk than that of primary grafting, however, it is acceptable in terms of mortality, when compared with the risk associated with emergency treatment.3,6,33
It is clear from the foregoing that early diagnosis is extremely important. An uninfected PAAA may evolve silently over a long period. Symptoms are absent or unusual. When present, they are non-specific and compatible with numerous differential diagnoses. Clinical signs are usually difficult to detect due to the retroperitoneal location of PAAA,4 therefore, imaging methods are necessary to make a diagnosis. The easiest, least invasive and most repeatable examination is color Doppler ultrasound, which reveals an abdominal aortic dilatation,34 although its nature and extension cannot always be defined. Angio-CT is always diagnostic and is the method of choice in order to define the extension and size of the aneurysm, the involvement of visceral arteries, relationships with adjacent organs and all the anatomical and morphological data necessary to plan the treatment strategy.9,35-37 In emergency cases, angio-CT is the method of choice to make the diagnosis and collect as much anatomical data as possible and also as quickly as possible. It is essential that esophagogastroduodenoscopy is performed prior to angio-CT in patients with acute or chronic gastrointestinal bleeding and a history of infrarenal aortic grafting in order to evaluate the origin of hematemesis or melena.4,9,38,39
All patients treated with abdominal aortic grafting must be followed-up with standardized, long-term evaluations, including clinical examination, color Doppler ultrasound6 and angio-CT. After a learning curve, we now perform clinical and abdominal ultrasound examinations 2 months after the intervention and then annually. Angio-CT should initially be reserved for patients whose ultrasound findings indicate the need for this investigation and then performed in all cases 5 years after the intervention, when the incidence of graft infection and PAAA begins to become significant.3,15,35,39 Such a periodic, life-long surveillance program should enable PAAA to be treated in elective conditions and with an acceptable interventional risk.6,9,27
Uninfected PAAA in symptomatic patients must always be treated. The indications to treat asymptomatic true PAAA are strictly related to the dimensions and the rate of growth of the aneurysm, as for generic abdominal aortic aneurysms: a sac diameter of 5 cm or more or twice the graft or normal aortic diameter11.
Many authors emphasize the importance of aggressive management of uninfected false PAAA:3,4,6,7,10,17,27,31-33,40 the reported incidence of rupture ranges from 8 to 55%, particularly when a surveillance program is not routinely performed.4,7,10,23 With regards to asymptomatic false PAAA, the diagnosis itself represents an indication to treat because of the fast, unpredictable evolution and higher incidence of rupture compared to that of true PAAA6,9-11,32,41 (in our population, all emergency cases were false PAAA). A pseudoaneurysm consists of a fibrotic capsule whose resistance to mechanical stress is lower than that of the native aortic wall, therefore, rupture is more frequent than rupture of a true PAAA and relatively independent of diameter. A watch-and-wait strategy seems to be justified only in electively manageable patients with a short life-expectancy and/or high surgical/anesthetic risk.9 However, careful evaluation of the risk/benefit ratio should be made when dealing with small false PAAA.4,9
Endovascular treatment of uninfected PAAA is based on the larger experience reported with infrarenal aortic aneurysms and has advantages that contribute significantly to reducing peri-operative morbidity and mortality.12,42-45 Our database includes information on only 3 patients who underwent endovascular treatment, but it is clear that this less invasive approach reduces complications and shortens time spent in the hospital by eliminating the above described technical/surgical risks. There were no peri-operative deaths in our subgroup of patients who were managed with an endovascular procedure and the complications described were minor events with a weak relationship with the procedure. The endovascular option for uninfected PAAA, however, has some limitations: the absence of an infrarenal neck long enough for an endoanastomosis (if considering a pararenal PAAA);12,42,43 the high risk of a type II endoleak from the patent caudal aorta or iliac arteries after proximal end-to-side reconstruction;42 the management of residual hypogastric vasculature;12 tortuosity and poor flexibility of iliac arteries/grafts due to periprosthetic fibrosis; persistent pressure of the PAAA on adjacent organs after effective exclusion of the aneurysm;12 graft infection;12,42,43 the absence of long-term results completely validating AAA endovascular treatment;42-45 and the failure of endograft/Dacron fixation.46 In particular, failed fixation of tube stent-grafts inside old Dacron, causing endotension and sac rupture has been documented, therefore, bifurcated endografts appear to be a more durable solution for exclusion of a PAAA.46 On the other hand, it has been suggested that tube aortic cuffs can sequentially be used in an overlapping configuration to create customized endografts and overcome the difficulties described above.47 The current use of fenestrated/branched endografts (which we have not yet experimented) has extended the indications for endovascular treatment to thoraco-abdominal48 and juxtarenal/pararenal aortic aneurysms.49,50 Such configurations which do not interfere with aortic side branches have been found useful in endovascular treatment of uninfected PAAA, resulting in significant reduction of major adverse events and death in the majority of cases lacking an infrarenal neck.51,52 Further trials are, however, necessary to validate the long-term efficacy of these newly available devices, which are associated with considerable incidences of early endoleak and in-stent stenosis in fenestration sites.49
In accordance with published data,7,9 our results confirmed the need for life-long clinical and imaging surveillance after aortic grafting; follow-up methods must be the cheapest and least invasive that enable early diagnosis of uninfected PAAA. This complication develops silently, and is difficult to repair and associated with a high mortality rate if treated as an emergency because of life-threatening complications. Elective surgical repair is advocated in order to minimize mortality and morbidity rates. Endovascular therapy with new generation devices is less invasive, bypasses surgical technical difficulties, and may represent an important option to combine safe treatment with a reduction of peri-operative adverse events.
Figures and Tables
Fig. 1
Kaplan-Meier product-limit survival estimates of the overall population of uninfected PAAA. PAAA, para-anastomotic aneurysm of the abdominal aorta.
ACKNOWLEDGEMENTS
The authors are grateful to Ilias Dalainas, (MD, PhD, A.F.I.C.A., F.I.C.S.), for support in the statistical analysis of the population's survival.
References
1. Biancari F, Ylönen K, Anttila V, Juvonen J, Romsi P, Satta J, et al. Durability of open repair of infrarenal abdominal aortic aneurysm: a 15-year follow-up study. J Vasc Surg. 2002. 35:87–93.

2. Crawford ES, Saleh SA, Babb JW 3rd, Glaeser DH, Vaccaro PS, Silvers A. Infrarenal abdominal aortic aneurysm: factors influencing survival after operation performed over a 25-year period. Ann Surg. 1981. 193:699–709.
3. Matsumura JS, Pearce WH, Cabellon A, McCarthy WJ 3rd, Yao JS. Reoperative aortic surgery. Cardiovasc Surg. 1999. 7:614–621.

4. Treiman GS, Weaver FA, Cossman DV, Foran RF, Cohen JL, Levin PM, et al. Anastomotic false aneurysms of the abdominal aorta and the iliac arteries. J Vasc Surg. 1988. 8:268–273.

5. Hagino RT, Taylor SM, Fujitani RM, Mills JL. Proximal anastomotic failure following infrarenal aortic reconstruction: late development of true aneurysms, pseudoaneurysms, and occlusive disease. Ann Vasc Surg. 1993. 7:8–13.

6. Mulder EJ, van Bockel JH, Maas J, van den Akker PJ, Hermans J. Morbidity and mortality of reconstructive surgery of noninfected false aneurysms detected long after aortic prosthetic reconstruction. Arch Surg. 1998. 133:45–49.

7. Curl GR, Faggioli GL, Stella A, D'Adato M, Ricotta JJ. Aneurysmal change at or above the proximal anastomosis after infrarenal aortic grafting. J Vasc Surg. 1992. 16:855–859. discussion 859-90.

8. Gautier C, Borie H, Lagneau P. Aortic false aneurysms after prosthetic reconstruction of the infrarenal aorta. Ann Vasc Surg. 1992. 6:413–417.

9. Allen RC, Schneider J, Longenecker L, Smith RB 3rd, Lumsden AB. Paraanastomotic aneurysms of the abdominal aorta. J Vasc Surg. 1993. 18:424–431. disussion 431-2.

10. Edwards JM, Teefey SA, Zierler RE, Kohler TR. Intraabdominal paraanastomotic aneurysms after aortic bypass grafting. J Vasc Surg. 1992. 15:344–350. disussion 351-3.

11. Odero A, Arici V, Canale S. [Proximal abdominal aortic aneurysms after infrarenal aortic reconstruction.]. Ann Ital Chir. 2004. 75:211–221.
12. Morrissey NJ, Yano OJ, Soundararajan K, Eisen L, McArthur C, Teodorescu V, et al. Endovascular repair of para-anastomotic aneurysms of the aorta and iliac arteries: preferred treatment for a complex problem. J Vasc Surg. 2001. 34:503–512.

13. van den Akker PJ, Brand R, van Schilfgaarde R, van Bockel JH, Terpstra JL. False aneurysms after prosthetic reconstructions for aortoiliac obsctructive disease. Ann Surg. 1989. 210:658–666.

14. Mii S, Mori A, Sakata H, Kawazoe N. Para-anastomotic aneurysms: incidence, risk factors, treatment and prognosis. J Cardiovasc Surg (Torino). 1998. 39:259–266.
15. In : Signorelli M, Gaeta A, De Nale A, Tosini S, Ranucci M, Tealdi DG, editors. Pseudoaneurismi anastomotici: una complicazione nella chirurgia vascolare ricostruttiva. 1988. Atti del XXVI World Congress of the International College of Surgeons; 03-09 July 1988; Milan. Bologna: Monduzzi Editore;561–565. Free papers printed in full.
16. Gaylis H. Pathogenesis of anastomotic aneurysms. Surgery. 1981. 90:509–515.
17. Gaylis H, Dewar G. Anastomotic aneurysms: facts and fancy. Surg Annu. 1990. 22:317–341.
18. Hallett JW Jr, Marshall DM, Petterson TM, Gray DT, Bower TC, Cherry KJ Jr, et al. Graft-related complications after abdominal aortic aneurysm repair: reassurance from a 36-year population-based experience. J Vasc Surg. 1997. 25:277–284. discussion 285-6.
19. Szilagyi DE, Smith RF, Elliott JP, Hageman JH, Dall'Olmo CA. Anastomotic aneurysms after vascular reconstruction: problems of incidence, etiology, and treatment. Surgery. 1975. 78:800–816.
20. Millili JJ, Lanes JS, Nemir P Jr. A study of anastomotic aneurysms following aortofemoral prosthetic bypass. Ann Surg. 1980. 192:69–73.

21. Starr DS, Weatherford SC, Lawrie GM, Morris GC Jr. Suture material as a factor in the occurrence of anastomotic false aneurysms. An analysis of 26 cases. Arch Surg. 1979. 114:412–415.

22. Mehigan DG, Fitzpatrick B, Browne HI, Bouchier-Hayes DJ. Is compliance mismatch the major cause of anastomotic arterial aneurysms? Analysis of 42 cases. J Cardiovasc Surg (Torino). 1985. 26:147–150.
23. Szilagyi DE, Elliott JP Jr, Smith RF, Reddy DJ, McPharlin M. A thirty-year survey of the reconstructive surgical treatment of aortoiliac occlusive disease. J Vasc Surg. 1986. 3:421–436.

24. Mikati A, Marache P, Watel A, Warembourg H Jr, Roux JP, Noblet D, et al. End-to-side aortoprosthetic anastomoses: long-term computed tomography assessment. Ann Vasc Surg. 1990. 4:584–591.

25. Plate G, Hollier LA, O'Brien P, Pairolero PC, Cherry KJ, Kazmier FJ. Recurrent aneurysms and late vascular complications following repair of abdominal aortic aneurysms. Arch Surg. 1985. 120:590–594.

26. Illig KA, Green RM, Ouriel K, Riggs P, Bartos S, DeWeese JA. Fate of the proximal aortic cuff: implications for endovascular aneurysm repair. J Vasc Surg. 1997. 26:492–490. discussion 499-501.

27. Lipski DA, Ernst CB. Natural history of the residual infrarenal aorta after infrarenal abdominal aortic aneurysm repair. J Vasc Surg. 1998. 27:805–811. discussion 811-2.

28. Coselli JS, LeMaire SA, Büket S, Berzin E. Subsequent proximal aortic operations in 123 patients with previous infrarenal abdominal aortic aneurysm surgery. J Vasc Surg. 1995. 22:59–67.

29. Cho JS, Gloviczki P, Martelli E, Harmsen WS, Landis ME, Cherry KJ Jr, et al. Long-term survival and late complications after repair of ruptured abdominal aortic aneurysms. J Vasc Surg. 1998. 27:813–829. discussion 819-20.

30. Baker DM, Hinchliffe RJ, Yusuf SW, Whitaker SC, Hopkinson BR. True juxta-anastomotic aneurysms in the residual infra-renal abdominal aorta. Eur J Vasc Endovasc Surg. 2003. 25:412–415.

31. Nevelsteen A, Suy R. Anastomotic false aneurysms of the abdominal aorta and the iliac arteries. J Vasc Surg. 1989. 10:595.

32. Locati P, Socrate AM, Costantini E. Paraanastomotic aneurysms of the abdominal aorta: a 15-year experience review. Cardiovasc Surg. 2000. 8:274–279.

33. Dennis JW, Littooy FN, Greisler HP, Baker WH. Anastomotic pseudoaneurysms. A continuing late complication of vascular reconstructive procedures. Arch Surg. 1986. 121:314–317.
34. Bastounis E, Georgopoulos S, Maltezos C, Balas P. The validity of current vascular imaging methods in the evaluation of aortic anastomotic aneurysms developing after abdominal aortic aneurysm repair. Ann Vasc Surg. 1996. 10:537–545.

35. Kalman PG, Rappaport DC, Merchant N, Clarke K, Johnston KW. The value of late computed tomographic scanning in identification of vascular abnormalities after abdominal aortic aneurysm repair. J Vasc Surg. 1999. 29:442–450.

36. Taylor LM Jr, Van Kolken RJ, Baur GM, Porter JM. Precise diagnosis of aortic anastomotic aneurysm by computed tomographic scan. Arch Surg. 1981. 116:1209–1211.

37. Guinet C, Buy JN, Ghossain MA, Mark AS, Jardin M, Fourmestraux J, et al. Aortic anastomotic pseudoaneurysms: US, CT, MR, and angiography. J Comput Assist Tomogr. 1992. 16:182–188.
38. Busuttil SJ, Goldstone J. Diagnosis and management of aortoenteric fistulas. Semin Vasc Surg. 2001. 14:302–311.

39. Bianchi P, Dalainas I, Ramponi F, Dell'Aglio D, Casana R, Nano G, et al. Late gastrointestinal bleeding after infrarenal aortic grafting: a 16-year experience. Surg Today. 2007. 37:1053–1059.

40. Kalman PG. What are the long-term results of conventional open surgical repair of abdominal aortic aneurysms? Acta Chir Belg. 2003. 103:197–202.

41. Melliere D, Berrahal D, Becquemin JP, Desgranges P, Cavillon A. [False anastomotic aneurysms after aorto-femoral prosthesis. Detection, prevention and treatment.]. J Mal Vasc. 1996. 21:158–164.
42. Yuan JG, Marin ML, Veith FJ, Ohki T, Sanchez LA, Suggs WD, et al. Endovascular grafts for noninfected aortoiliac anastomotic aneurysms. J Vasc Surg. 1997. 26:210–221.

43. Liewald F, Kapfer X, Görich J, Halter G, Tomczak R, Scharrer-Pamler R. Endograft treatment of anastomotic aneurysms following conventional open surgery for infrarenal aortic aneurysms. Eur J Vasc Endovasc Surg. 2001. 21:46–50.

44. Magnan PE, Albertini JN, Bartoli JM, Ede B, Valerio N, Moulin G, et al. Endovascular treatment of anastomotic false aneurysms of the abdominal aorta. Ann Vasc Surg. 2003. 17:365–374.

45. Faries PL, Won J, Morrissey NJ, Briggs VL, Cadot H, Carroccio A, et al. Endovascular treatment of failed prior abdominal aortic aneurysm repair. Ann Vasc Surg. 2003. 17:43–48.

46. van Herwaarden JA, Waasdorp EJ, Bendermacher BL, van den Berg JC, Teijink JA, Moll FL. Endovascular repair of paraanastomotic aneurysms after previous open aortic prosthetic reconstruction. Ann Vasc Surg. 2004. 18:280–286.

47. Zhou W, Bush RL, Bhama JK, Lin PH, Safaya R, Lumsden AB. Repair of anastomotic abdominal aortic pseudoaneurysm utilizing sequential AneuRx aortic cuffs in an overlapping configuration. Ann Vasc Surg. 2006. 20:17–22.

48. Anderson JL, Adam DJ, Berce M, Hartley DE. Repair of thoracoabdominal aortic aneurysms with fenestrated and branched endovascular stent grafts. J Vasc Surg. 2005. 42:600–607.

49. O'Neill S, Greenberg RK, Haddad F, Resch T, Sereika J, Katz E. A prospective analysis of fenestrated endovascular grafting: intermediate-term outcomes. Eur J Vasc Endovasc Surg. 2006. 32:115–123.
50. Greenberg RK, West K, Pfaff K, Foster J, Skender D, Haulon S, et al. Beyond the aortic bifurcation: branched endovascular grafts for thoracoabdominal and aortoiliac aneurysms. J Vasc Surg. 2006. 43:879–886. discussion 886-7.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download