Abstract
Purpose
To investigate the reliability of intra-atrial electrocardiogram (ECG) use for external jugular vein (EJV) catheterization.
Materials and Methods
Patients undergoing open heart surgery in Suleyman Demirel University Hospital between February and June 2006 were included in the study. Using a sterile Seldinger technique, a triple lumen polyurethane central venous catheter was introduced (Certofix® Trio V 720, length 20 cm, 7 French) under intra-atrial ECG guidance. The presence of an increase in P-wave size was recorded. Just after the surgery, a portable chest X-ray was taken. The method was considered to be successful when a change in P-wave could be seen and the catheter was in the superior vena cava, as well as when there was no change in P-wave and the catheter was not in the superior vena cava.
Results
In six patients (12%), we were not able to advance the guidewire. In the remaining 44 patients, the catheter was inserted without problem. Eight of these 44 catheters were positioned in the innominate vein, with a malposition ratio of 18%. The success rate of external jugular vein cannulation with intra-atrial ECG was 95%. No complications occured related to the EJV cannulation.
Central venous access plays an increasingly important role in the delivery of modern care. Many studies on the venous access sites for central venous catheterization have been conducted.1-5 The preferred access site for central venous catheter placement continues to be the right internal jugular vein (IJV).
When the right IJV is not available for central venous access, the second access site remains variable. Although the left IJV and the subclavian veins (SCV) have been used for second access, several studies suggest that both SCVs and the left IJV should be avoided because of a high incidence of procedural complications (pneumothorax, arterial puncture) as well as central venous stenosis and thrombosis.2-6 The left IJV is also related with a high incidence of catheter malfunction.6 Some authors believe that the second venous access after the right IJV should be the right external jugular vein (EJV).3,7 One reason for use of the right EJV is its relatively straightforward course and short length, which are very similar to those of right IJV. A second reason is that the EJV is easily accessed, given its superficial location on the neck.7 However, it is suggested that the incidence of malpositioned catheters via the EJV approach makes this route unreliable.8 To decrease the incidence of catheter dislodgement, vessel wall erosion, thromboembolism and catheter malfunction, accurate positioning of the catheter tip near or at the junction of the superior vena cava (SVC) and right atrium (RA) is necessary.9 It is possible to decrease the incidence of malposition with the use of additional techniques. Various techniques have been determined to ensure the correct placement of central venous catheters. An alternative technique to roentgenography has been developed to reduce radiation exposure and cost: atrial electrocardiogram (ECG).10 Right atrial electrocardiography is a technique that assures tip position outside the heart.
We aimed to investigate the reliability of intra-atrial ECG use for EJV catheterization.
The study protocol was approved by the local ethics committee. This prospective, randomized, single-centre study was performed in the section for cardiothoracic and vascular anaesthesia of a Suleyman Demirel University Hospital between February and June 2006. Patients undergoing open heart surgery were included in the study. Written informed consent was obtained from each patient. Following the induction of general anesthesia, patients were placed in a 200 Trendelenburg position and the right side of the neck and upper chest of the patient were prepared according to sterile technique. The right EJV was identified by visual inspection and palpation and then punctured high in the neck. The vein was entered using a sterile Seldinger technique, the guide wire was advanced and a triple lumen polyurethane central venous catheter was introduced (Certofix® Trio V 720, length 20 cm, 7 French). The kit includes a connection cable with a crocodile clip for connecting the guide wire to a Certodyn® universal adaptor (both B. Braun Melsungen AG, Melsungen, Germany). The guide wire was used as a bipolar electrode. A black marking on the proximal end of the guide wire indicates the point at which the tip of the wire levels with the port of the distal catheter lumen. The sterile connection cable was clamped to the guide wire at the marked position in order to connect it to the adaptor that allows the operator to switch from a surface to an intravascular ECG. The catheter was then advanced together with the guide wire, until an increase in P-wave size was detected. The presence of an increase in P-wave size was recorded. Both catheter and guide wire were then withdrawn until the P-wave returned to a normal size. Markings on the catheter allowed for the measurement of its depth of insertion. Then all three lumina of the catheter were tested for free back flow of venous blood. If there was any difficulty in aspirating the venous blood, the catheter was rotated by up to 3600. If problems persisted, the catheter was advanced by 1 cm. The whole procedure of aspiration, and turning and advancing the catheter was repeated until no difficulty in aspirating the lumina was detected. At this position, the catheter was sutured to the skin and final insertion depth was recorded.
Just after the surgery, a portable chest X-ray was taken. The radiographic SVC-RA junction was defined as the apex of the concave shadow formed by the superimposition of the distal superior vena cava on the right atrium.11 The catheter position was determined by a radiologist who was blinded to the presence of increases in the P-wave during insertion of the catheter. When a P-wave increase was not detected during insertion of the catheter, the position of the catheter was immediately controlled with fluoroscopy. The malpositioned catheters were removed and internal jugular catheterization was performed. One anaesthesist placed all the central venous catheters.
Patient characteristics that were recorded include age, sex, weight and height. A Chi-square test was used to assess the differences related to sex and a Mann-Whitney-U test was used to assess the differences associated with age, weight and height between patients with well positioned and malpositioned catheters and between patients in whom the method was successful and unsuccessful. p < 0.05 was considered statistically significant.
In six patients (12%), we were not able to advance the guidewire. The major reason for failure was an inability to pass the guidewire below the clavicle. In the remaining 44 patients, the catheter was inserted without any problems (Fig. 1). Eight of these 44 catheters were positioned in the left innominate vein (Fig. 2), with a malposition ratio of 18%. P-wave increases were not detected in any of the malposition cases. When the malposition was detected with fluoroscopy, the EJV catheter was replaced with an IJV catheter. An increase in the P-wave was detected in 34 out of the 36 patients with well-positioned catheters (Fig. 3). With the use of radionuclid angiography (Tc99 m pertecnetat), we tried to reveal any anatomic variation which could cause the catheter to follow a transverse course into the left innominate vein instead of going directly down into the superior vena cava. However, we detected no variation which could explain these malpositions.
The method was considered to be successful when a change in P-wave could be seen and the catheter was in the superior vena cava, and also when there was no change in the P-wave and the catheter was not in the superior vena cava. According to this determination, the success rate of external jugular vein cannulation with intra-atrial ECG was 95%. In two patients in whom the catheter was well positioned on chest X-ray and the P-wave increase was absent, we did not detect any manifestions of cardiac pathologies nor arrhythmias.
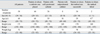
There was no significant difference between patients with well positioned and malpositioned catheters regarding sex, age, weight or height. There was no significant difference between patients in whom the method was successful and unsuccessful regarding sex, weight or height. Patients in whom the method was unsuccessful were primarily younger than patients in whom the method was successful (p < 0.05) (Table 1).
In all of the cases without malposition, the tip of the catheter was 1-3 cm beyond the pericardial reflection (atrio-caval junction) on chest X-ray. None of the central venous catheter tips were in the right atrium. The depth of the successfully positioned catheters was 12.5 cm (range 10-15 cm). No EJV cannulation related complications occured.
The right IJV runs straight down to the superior vena cava, which obviously reduces the risk of malposition and possibly also of central venous obstruction.12 The EJV is formed just below and behind the angle of the mandible by union of the posterior auricular and retromandibular veins. It lies under the platysma muscle in the neck and obliquely crosses the superficial surface of the sternocleidomastoid muscle. Approximately 2 cm above the middle of the clavicle, it passes through the cervical fascia to enter the SCV. Of anatomic importance for catheterization is the fact that the EJV forms an acute angle at its insertion into the SCV, which may explain the higher rate of malposition.13 It has been suggested that there is an inverse correlation between EJV and IJV diameters.14 If the right IJV is occluded, the diameter of the right EJV must be greater and therefore catheterization would favor the right EJV.7 Although performance results of central venous catheter access through the right EJV are expected to be similar to those through the right IJV,3 some authors suggest that the incidence of malpositioned catheters via the EJV approach makes this route unreliable.8
Cho et al.7 summarized the recent studies where the technical success rate for right EJV catheterization is between 88% and 96%. The unsuccessful punctures are generally related to the thrombosis of EJV and SCV and congenital absence of the EJV.14 In the present study, the technical success rate was 88%. The major reason for a failure was an inability to pass the guidewire below the clavicle.
In children, the success in IJV catheterization is 86% while the success in EJV catheterization is 65%.8 The incidence of catheter malposition following EJV catheterization is reported as 14%. In the study conducted by Belani et al.,15 IJV cannulation was successful in 91% of the patients, and an intrathoracic location was achieved in 100% of the cases; complications occured in 12.8% of the patients while external jugular vein cannulation using a 'J' wire technique yielded a 76% success rate with 93.7% of catheter tips reaching an intrathoracic location with no complications. Jobes et al.16 combined a retrospective study with 1,021 patients and a prospective study with 1,284 patients. In the restrospective study, the success rate and incidence of arterial puncture were respectively 95.3% and 4.2% for IJV. The prospective study revealed a success rate of 93.2% for IJC catheterization while the success rate was 74% with any arterial puncture complication for EJV. Malatinsky et al.17 reported that the malposition incidence was 30% and 5.7% for EJV and IJV respectively. The malposition incidence was 18% in the present study. What is interesting in the present study is that all the malpositioned catheters were placed in the left innominate vein. In recent studies, the malpositioned catheters showed extrathoracic placement, predominantly in the neck and arm veins.8,15,18 The external jugular veins are known to be so variable that it is not possible to determine a 'normal pattern'.19 But with the use of radionuclid angiography (Tc99m pertecnetat), we detected no variation which could explain these malpositions.
The literature suggests that serious mechanical complications of central venous catheterization, although uncommon, are associated with a high mortality rate. Death is associated with an intracardiac placement.20 Positioning a catheter tip in the right atrium is thought to increase the likelihood of cardiac arrhythmias. Despite this persistent corcern, there is minimal evidence to suggest that this is a significant problem.21
It is also important to understand that in the majority of patients, a catheter tip will exhibit a range of movement extending 2-3 cm.21 Since tip movement is well documented, it seems reasonable to recommend that the tip be maintained proximal to the right atrium.20
To decrease the incidence of catheter dislodgement, vessel wall erosion, thromboembolism and catheter malfunction, accurate positioning of the catheter tip near or at the junction of the superior vena cava and right atrium is necessary.9 The catheter tip should be placed in as large a vein as possible, ideally outside the heart and parallel with the long axis of the vein such that the tip does not abut the vein or heart wall.22
A major problem in correctly placing central venous catheters is the lack of reliable surface landmarks. In the study conducted by Peres,23 where the anesthesiologists attempted to place central venous catheters above the right atrium using conventional techniques, 24% of central venous catheter tips terminated within the right atrium. Several studies have reported that 10-30% of catheters placed without imaging guidance have a malpositioned catheter tip or a catheter tip in the right atrium.23,24
Although most of the authors recommend a chest X-ray as the only practical, reliable test, a frontal chest radiograph does not exclude a catheter position in smaller vessels (e.g. azygos vein) or extravascular site adjacent to the correct site. Determining the border between the SVC and RA on chest radiograph can be challenging. The lower radiographic quality of the bedside chest radiograph makes it more difficult. In addition, Hsu et al.25 showed that the radiographic SVC-RA junction ranged from 2.8 cm above to 0.6 cm below the echocardiographic SVC-RA junction indicated by catheter tip. As a limitation of the present study, we have to mention that a chest radiograph does not precisely determine the SVC-RA junction.
In many hospitals, ECG guidance for central venous catheter placement has replaced a post-insertion chest X-ray to check its position. In some countries, from a legal point of view, ECG guidance is equivalent to a chest X-ray.11 ECG-guided central venous catheter placement claims to detect the intra-atrial position of the tip of central venous catheters by detecting an intra-atrial P-wave (P-atriale) with the exploring electrode. The adjacent atrial wall tissue is thought to be responsible for the increase in the voltage of the P-atriale.20,22
Lack of an increase in P-wave size indicates an aberrant catheter placement in vessels other than the superior vena cava.11
Salmela and Aromaa18 installed 321 central venous catheters from different venous access points that were accompanied by an intra-atrial ECG and obtained a 92% success rate. The method was considered to be successful when a change in the P-wave could be seen and the catheter was in the superior vena cava, and also when there was no change in P-wave and the catheter was not in the superior vena cava, similar to the present study. The authors indicated that the failure of the intra-atrial ECG was related to manifestions of myocardial pathology, arrhythmias, or insufficient catheter length to reach the right atrium. In the present study, a similar success rate (95%) was obtained. In two patients, although a P-wave increase was absent, the catheter was well positioned on the chest X-ray. We did not detect any manifestions of cardiac pathologies nor arrhythmias in these patients. The patients in whom the method failed were younger than the patients in whom the method was successful, which seems to have no clinical significance. When the catheter malposition was detected on chest X-ray, the EJV was replaced with an IJV catheter. On the other hand, Fletcher and Bodenham22 indicated that positioning in the mid-point of the left innominate vein is a suitable site when the catheter is introduced from the left IJV or SCV.
Some authors suggested that an increase in the P-wave amplitude already starts at the pericardial reflection outside the heart and ECG guidance cannot distinguish whether a catheter is placed intraarterially or intravenously.11,26 Fluoroscopy or transesophageal echocardiography may be more reliable methods to detect the position of central venous catheters.
There were no procedural complications to report in the present study. However it should be noted that the superficial location of the EJV and the small amount of subcutaneous tissue over the EJV may lead to an oozing of blood. Because this oozing is easily controlled, we did not regard it as a complication.
In conclusion, considering that it is easily accessed without any complications, and the malposition is successfully detected by intra-atrial ECG, EJV is a suitable access vector for central venous cannulation when IJV is not usable.
Figures and Tables
Fig. 1
Appropriate localization of the external jugular vein catheter on chest X-ray. Catheter tip marked with an arrow.
ACKNOWLEDGEMENTS
The study was carried out in Suleyman Demirel University, School of Medicine, Department of Anesthesiology and Reanimation.
References
2. Trerotola SO, Kuhn-Fulton J, Johnson MS, Shah H, Ambrosius WT, Kneebone PH. Tunneled infusion catheters: increased incidence of symptomatic venous thrombosis after subclavian versus internal jugular venous access. Radiology. 2000. 217:89–93.

3. Trerotola SO. You are asked to place a dialysis access catheter in a patient. What is your preferred access site, and why? J Vasc Interv Radiol. 1997. 8:75–76.
4. Macdonald S, Watt AJ, McNally D, Edwards RD, Moss JG. Comparison of technical success and outcome of tunneled catheters inserted via the jugular and subclavian approaches. J Vasc Interv Radiol. 2000. 11:225–231.

5. Schillinger F, Schillinger D, Montagnac R, Milcent T. Post catheterisation vein stenosis in haemodialysis: comparative angiographic study of 50 subclavian and 50 internal jugular accesses. Nephrol Dial Transplant. 1991. 6:722–724.

6. Moss AH, McLaughlin MM, Lempert KD, Holley JL. Use of a silicone catheter with a Dacron cuff for dialysis short-term vascular access. Am J Kidney Dis. 1988. 12:492–498.

7. Cho SK, Shin SW, Do YS, Park KB, Choo SW, Choo IW. Use of the right external jugular vein as the preferred access site when the right internal jugular vein is not usable. J Vasc Interv Radiol. 2006. 17:823–829.

8. Nicolson SC, Sweeney MF, Moore RA, Jobes DR. Comparison of internal and external jugular cannulation of central circulation in the pediatric patient. Crit Care Med. 1985. 13:747–749.

9. Chu KS, Hsu JH, Wang SS, Tang CS, Cheng KI, Wang CK, et al. Accurate central venous port-A catheter placement: intravenous electrocardiography and surface landmark techniques compared by using transesophageal echocardiography. Anesth Analg. 2004. 98:910–914.

10. Watters VA, Grant JP. Use of electrocardiogram to position right atrial catheters during surgery. Ann Surg. 1997. 225:165–171.

11. Schummer W, Herrmann S, Schummer C, Funke F, Steenbeck J, Fuchs J, et al. Intra-atrial ECG is not a reliable method for positioning left internal jugular vein catheters. Br J Anaesth. 2003. 91:481–486.

12. Mickley V. Central venous catheters: many questions, few answers. Nephrol Dial Transplant. 2002. 17:1368–1373.

13. McCowan TC, Ferris EJ, Carver DK, Harshfield DL. Use of external jugular vein as a route for percutaneous inferior vena caval filter placement. Radiology. 1990. 176:527–530.

14. Stickle BR, McFarlane H. Prediction of a small internal jugular vein by external jugular vein diameter. Anaesthesia. 1997. 52:220–222.

15. Belani KG, Buckley JJ, Gordon JR, Castaneda W. Percutaneous cervical central venous line placement: a comparison of the internal and external jugular vein routes. Anesth Analg. 1980. 59:40–44.
16. Jobes DR, Schwartz AJ, Greenhow DE, Stephenson LW, Ellison N. Safer jugular vein cannulation: recognition of arterial puncture and preferential use of the external jugular route. Anesthesiology. 1983. 59:353–355.
17. Malatinsky J, Kadlic T, Májek M, Sámel M. Misplacement and loop formation of central venous catheters. Acta Anaesthesiol Scand. 1976. 20:237–247.

18. Salmela L, Aromaa U. Verification of the position of a central venous catheter by intra-atrial ECG. When does this method fail? Acta Anaesthesiol Scand. 1993. 37:26–28.

19. Illustrated encyclopedia of human anatomic variation [www document]. accessed on 25 May 2007. URL http://www.anatomyatlases.org/AnatomicVariants/AnatomyHP.shtml.
20. McGee WT, Ackerman BL, Rouben LR, Prasad VM, Bandi V, Mallory DL. Accurate placement of central venous catheters: a prospective, randomized, multicenter trial. Crit Care Med. 1993. 21:1118–1123.
21. Vesely TM. Central venous catheter tip position: a continuing controversy. J Vasc Interv Radiol. 2003. 14:527–534.

22. Fletcher SJ, Bodenham AR. Safe placement of central venous catheters: where should the tip of the catheter lie? Br J Anaesth. 2000. 85:188–191.
23. Peres PW. Positioning central venous catheters-a prospective survey. Anaesth Intensive Care. 1990. 18:536–539.
24. Aslamy Z, Dewald CL, Heffner JE. MRI of central venous anatomy: implications for central venous catheter insertion. Chest. 1998. 114:820–826.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download