Abstract
We report a 65 year-old man with a large cystic phyllodes tumor of the prostate. The patient complained of abdominal discomfort and had a soft palpable mass. Computer tomography showed a solid and cystic mass in the pelvic fossa; the mass was adjacent only to the prostate. We excised the mass. Microscopic findings of the mass showed hyperplastic epithelium lined cysts with leaf-like intraluminal epithelia lined stromal projections, less than 2 mitotic counts/10 HPF, low-to-moderated cellularity, and mild-to-moderate cytoplasm atypia. The pathological findings were consistent with a phyllodes tumor of the prostate, a low-grade tumor. Twenty-eight months after the operation, the patient was well with no recurrence or metastases.
Phyllodes tumors of the prostate are rare neoplasms; histologically, they resemble breast tumors. They are characterized by a distinctive biphasic pattern of a leaf-like intraluminal epithelia lined stromal projections compressed by a hyperplastic stromal component and variable cellular spindle cell stroma.1-3 Most phyllodes tumors have been reported after transurethral resection of the prostate specimen.4 Some cases have been reported after open surgery where benign and malignant changes are not clearly defined.5 Diagnosis by needle biopsy is difficult because architectural features are not well defined. In this report, we describe a patient with a large cystic phyllodes tumor of the prostate.
A 65-year-old man was admitted to our hospital with an abdominal mass. The mass was noted 1 month prior to admission. The patient's history was negative for diabetes, hepatitis, hypertension, and pulmonary tuberculosis. The patient complained of abdominal discomfort, and a large mass could be palpated on the physical examination. The abdominal mass was about 6 × 7 cm, soft, non tender, and easily moved. The digital rectal examination revealed a firm, not enlarged, not tender, and smooth margined prostate. The other physical findings and the laboratory studies were within normal limits.
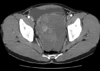
Computer tomography (CT) was performed and showed about a 13.7 cm solid and cystic mass in the pelvic fossa. The mass had solid and cystic portions as well as central enhancement and hemorrhagic portions. The mass had an enhancing thin capsule. Infiltration into adjacent solid organs, such as the urinary bladder, rectum and left ureter were not visualized. However, the margin with the prostate was uncertain (Fig. 1).
Aspiration of the cystic mass was performed. The pathological findings were consistent with a fibroma, however, a malignancy could not be ruled out, because of increased cellularity and pleomorphism.
At surgery, there was a very large cystic mass about 7 cm on the upper portion of the bladder, and the ureter coursed over the mass. The cystic mass was in the retroperitoneal space. The base of the mass mildly adhered to the prostatic capsule, but was easily dissected. The specimen consisted of a pink-white solid mass, measuring 9 × 8 × 7 cm and weighing 300 gm. The external surface was smooth. On the sections, the cut surface was semisolid (4 cm in diameter) with semicystic changes (5 cm in diameter) and had multifocal hemorrhagic foci. The microscopic findings showed hyperplastic epithelium lined cysts with leaf-like intraluminal epithelia lined stromal projections. Compressed and elongated slit-like epithelial lined spaces had less than 2 mitotic counts/10 HPF, low-to-moderated cellularity and mild-to-moderate cytoplasm atypia. The immunohistochemical stains were positive for CD34 and actin, focally positive for desmin and negative for NSE, S-100, and CD 56 (Fig. 2). The final pathological results were consistent with a phyllodes tumor of the prostate, a low-grade tumor. Twenty-eight months after surgery, the patient was well without recurrence or metastases.
Phyllodes tumors of the prostate are very rare. These tumors are pathologically similar to mammary gland tumors. It can have both benign and malignant components and is found in patients from 22 to 86 years of age (mean age 55).3 Patients with phyllodes tumor of the prostate present with urinary obstructive symptoms such as hesitancy and straining at voiding. Some patients have hematuria. Many patients are pathologically diagnosed after transurethral resection of the prostate. Our patient complained of abdominal pain and had a palpable mass, radiologically identified with cystic characteristics. When the tumor was removed, the pathological findings showed a phyllodes tumor of the prostate. The tumor had hyperplastic epithelium lined cysts with leaf-like intraluminal epithelia lined stromal projections, similar to tumors of the breast. Phyllodes tumors are pathologically divided into low-grade (benign), intermediate and high-grade (malignant) tumors, depending on their mitotic activity, stromal cellularity, and the stromal/epithelial ratio.
Benign phyllodes tumors have a low stromal/epithelial ratio, less cellular atypia and minimal mitotic activity. However, phyllodes tumors of the prostate, even when benign, frequently recur and spread to contiguous organs and occasionally metastasize.6,7 Sauder8 reported a local recurrence of a benign phyllodes tumor after simple resection and radical prostatectomy, and Bostwick et al.3 reported that about 50% of patients with a low grade phyllodes tumor had a recurrence within 2 years of surgery. However, recurrence and overall survival rates are more favorable for benign phyllodes tumors than the malignant forms. The treatment of phyllodes tumors of the prostate is radical surgery. Negative surgical margins are important for a patient's outcome. The treatment for metastatic and recurrent cases of phyllodes tumor has not yet been established, due to its rarity. Lam and Yeo9 reported the efficacy of chemotherapy with ifosfamide and doxorubicin for lung metastasis after radical prostatectomy, in addition to adjuvant irradiation. Yamamoto10 reported that radiation therapy is limited to patients with metastatic tumors, and Mizuaki11 reported the effects of VIP chemotherapy as induction therapy.
For the case presented in this report, simple excision of a very large tumor was performed. We recommended a radical prostatectomy, but the patient refused. The patient is being with radiological evaluation followed closely every 3 months. Twenty-eight months after surgery, the patient is well with no tumor recurrence or metastasis.
Figures and Tables
References
1. Gaudin PB, Rosai J, Epstein JI. Sarcomas and related proliferative lesions of specialized prostatic stroma: a clinicopathologic study of 22 cases. Am J Surg Pathol. 1998. 22:148–162.

2. Wu YS, Lee SH, Shen BY, Chang PL, Tsui KH, Ng KF. Malignant phyllodes tumor of the prostate. Arch Androl. 2005. 51:295–298.

3. Bostwick DG, Hossain D, Qian J, Neumann RM, Yang P, Young RH, et al. Phyllodes tumor of the prostate: long-term followup study of 23 cases. J Urol. 2004. 172:894–899.
4. Watanabe M, Yamada Y, Kato H, Imai H, Nakano H, Araki T, et al. Malignant phyllodes tumor of the prostate: retrospective review of specimens obtained by sequential transurethral resection. Pathol Int. 2002. 52:777–783.

5. Chen TA, Chou JM, Sun GH, Lee HS. Malignant phyllodes tumor of the prostate. Int J Urol. 2005. 12:1007–1009.

6. Kim HS, Lee JH, Nam JH, Lee MC, Park CS, Juhng SW, et al. Malignant phyllodes tumor of the prostate. Pathol Int. 1999. 49:1105–1108.

7. Latif Z, Clark D, Nairn ER, Gurun M. Phyllodes tumor of the prostate: a rare condition requiring careful surveillance. J Urol. 2003. 170:1944.

9. Lam KC, Yeo W. Chemotherapy induced complete remission in malignant phyllodes tumor of the prostate metastasizing to the lung. J Urol. 2002. 168:1104–1105.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download