Abstract
During drug treatment of tuberculous lymphadenitis, paradoxical response (PR) may occasionally occur. Continued treatment or lymph node aspiration improves PR without severe sequelae. However, we report a case of severe PR in a patient with cervical lymph node tuberculosis causing airway obstruction due to retropharyngeal lymph node swelling during antituberculous treatment. Tracheostomy and drainage of the node were performed to secure the airway. Possible airway obstruction due to PR must be suspected when cervical lymph node tuberculosis involves the retropharyngeal lymph node.
Paradoxical response (PR) during antituberculous treatment has well been documented, particularly in human immunodeficiency virus (HIV)-positive patients. PR poses a problem because it is difficult to differentiate from other conditions such as drug resistance, poor compliance to drug therapy, concomitant diseases, poor drug absorption, and side effects of antituberculous therapy. Furthermore, PR may require surgical exploration or result in other morbidities.
PRs occur in approximately 20% of patients during the course of lymph node tuberculosis treatment; however, most of them improve without severe sequelae.1 Continuance of the drug regimen and, if necessary, lymph node aspiration are usually sufficient to treat this condition, and aggressive surgical procedures are generally not required. Here, we report the first case of severe PR in an HIV-negative patient who experienced airway obstruction due to PR during treatment for cervical lymph node tuberculosis. In this case, tracheostomy and drainage of the lymph node were performed in order to secure the airway.
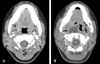
A 19-year-old woman visited our clinic, presenting with swelling of the neck for past few days. A physical examination revealed many enlarged lymph nodes on both sides of her neck. Complete blood count (CBC) revealed a leukocyte count of 7.5 × 109/L, of which neutrophils and lymphocytes accounted for 63.2% and 28.9%, respectively; a hemoglobin count of 13.1 g/dL, and a platelet count of 239 × 109/L. Computed tomography (CT) revealed multiple enlarged lymph nodes with central necrosis at the neck levels II, III, and V, and in the retropharyngeal space (Fig. 1A). Fine needle aspiration of the right cervical lymph node revealed chronic granulomatous inflammation with necrosis, which was consistent with that observed in tuberculosis. Acid-fast bacilli (AFB) staining revealed numerous acid-fast bacilli, and tuberculosis polymerase chain reaction (PCR) was positive. AFB culture of lymph node tissue was not performed. The patient tested seronegative for HIV, and her chest X-ray indicated no abnormalities. She was diagnosed with tuberculous lymphadenitis and treated with a drug regimen of isoniazid, rifampin, pyrazinamide, and ethambutol.
At 5 weeks, the patient was admitted to the hospital because of enlarged cervical lymph nodes and breathing difficulty. She complained of dyspnea and appeared tachypneic. Her respiration rate was 25/min. A physical examination revealed an enlarged lymph node on the right side of her neck and protrusion of the retropharyngeal wall blocking the pharyngeal space. A neck CT obtained at time of admission revealed the enlarged retropharyngeal lymph node with central necrosis, which had also been observed previously. This lymph node protruded into the pharyngeal space, blocking the airway (Fig. 1B). Her dyspnea did not improve despite oxygen therapy. Therefore, tracheostomy was performed as an emergency measure to resolve the narrowing of the airway and to prevent its imminent obstruction, following which the retropharyngeal lymph node was incised and drained. At the time of surgery, tissue culture was negative. AFB smear examination and culture also yielded negative results. The patient's antituberculous medications were continued, and the same regimen used previously was followed. In addition, ceftizoxime 2.0 g/day was administered for 2 weeks. The tracheostomy site was sealed at 2 weeks. The enlarged cervical lymph nodes decreased in size with continued antituberculous therapy. At 2 months, the drug regimen was altered to isoniazid, rifampin, and ethambutol. At 5 months, the left supraclavicular lymph node was enlarged and fluctuant, necessitating lymph node aspiration. The results of AFB stain and AFB culture were negative. The enlarged lymph nodes decreased further in size and resolved without any modification in the medication. At 11 months, the right supraclavicular lymph node was enlarged, and the AFB stain and culture of fine needle aspirates were also negative. The lymph node enlargement improved with the continuation of the same antituberculous regimen administered previously. Antituberculous treatment was continued for 1 year and 2 months.
Tuberculosis can worsen despite aggressive antimycobacterial treatment. This troublesome condition is termed PR and defined as clinical or radiological worsening of preexisting tuberculous lesions or the development of new lesions following the initiation of active antituberculous treatment.2 It includes the development of intracranial tuberculomas, worsening of existing lesions or development of new lesions in the lymph nodes, and various other manifestations.3,4 In patients coinfected with HIV and TB, paradoxical reactions occur more frequently when highly active antiretroviral treatment (HAART) is initiated and constitutes the immune reconstitution inflammatory syndrome (IRIS).5 PR is well described in HIV-positive patients; however, relatively few cases have been reported in HIV-negative patients. PR occurs more frequently in HIV-positive patients than in HIV-negative patients. It was reported among 20 - 30% of HIV-positive patients receiving antituberculous treatment and up to 40% of HIV-positive patients with lymph node tuberculosis.6,7
Hawkey et al. reported PR in approximately 1/4 of HIV-negative patients receiving treatment for lymph node tuberculosis4. The onset of the disease was at 10 - 405 days (median: 46 days) and the duration of 28 - 231 days (median: 67.5 days). PR symptoms are swelling of the existing lymph node lesion, formation of new lymph node lesions, and discharging sinus, etc. Cheng et al. determined that HIV-negative patients experiencing PR were more likely to have extrapulmonary tuberculosis at initial diagnosis and exhibited lower baseline lymphocyte count and greater increases in absolute lymphocyte count.8 The mechanism of PR has not clearly been defined to date, although it is believed that, the immune response against mycobacterial proteins may be enhanced and cause a local hypersensitive reaction when active antituberculous therapy is initiated and immunosuppression declines.9 It is also believed thats onset of PR may depend on the host immune response, virulence of tubercle bacilli, antigen load, site of infection, and effects of chemotherapy.7
The mainstay of PR management is the continuation of antituberculous treatment without any modification of drug regimen. However, duration of treatment may be prolonged to 9 - 12 months or more, depending on the site of infection or clinical condition6. In the present case, repeated PR and treatment without steroid might have contributed to the prolonged duration of treatment. Some reports suggest the use of systemic steroids as an adjuvant treatment modality for PR.6,10 The benefit of corticosteroid therapy for PR is apparent in intracranial tuberculomas, however, is somewhat controversial in other situations such as lymph node tuberculosis.9,11 In the case of lymph node compression of the intrapulmonary airway, adjunctive steroid therapy may be helpful in improving PR.12 In some situations, surgical exploration is necessary to ameliorate PR. In case of intracranial lesions, craniotomy or shunt operations are performed to decompress the increased intracranial pressure (IICP).
PR occurring during treatment of cervical lymph node tuberculosis can improve with continued antituberculous treatment or, if necessary, with lymph node aspiration or surgical drainage without severe sequelae. In the literature, there are no reports of PR occurring in a case of cervical lymphadenopathy causing difficulty in breathing due to airway obstruction. To our knowledge, this is the first case that required a tracheostomy to relieve the extrathoracic airway obstruction caused by PR in cervical lymphadenopathy. In general, cervical lymphadenopathy has a mild course; however, as in this case, severe PR might occur due to swelling of the lymph node in the retropharyngeal space and may cause airway obstruction. In such cases, a surgical approach such as tracheostomy or administration of steroids should be considered. Hence, when treating patients with tuberculous lymphadenitis involving the retropharyngeal lymph nodes, we should be cautious about the possibility of the development of severe PRs such as airway obstruction.
In summary, PR is not uncommon during treatment of cervical lymph node tuberculosis, and it frequently improves without severe sequelae. However, when it occurs in the retropharyngeal space, severe complications, such as airway obstruction, might occur and require surgical interventions such as tracheostomy.
Figures and Tables
References
1. Polesky A, Grove W, Bhatia G. Peripheral tuberculous lymphadenitis: epidemiology, diagnosis, treatment, and outcome. Medicine (Baltimore). 2005. 84:350–362.
3. Chambers ST, Hendrickse WA, Record C, Rudge P, Smith H. Paradoxical expansion of intracranial tuberculomas during chemotherapy. Lancet. 1984. 2:181–184.
4. Hawkey CR, Yap T, Pereira J, Moore DA, Davidson RN, Pasvol G, et al. Characterization and management of paradoxical upgrading reactions in HIV-uninfected patients with lymph node tuberculosis. Clin Infect Dis. 2005. 40:1368–1371.
5. McIlleron H, Meintjes G, Burman WJ, Maartens G. Complications of antiretroviral therapy in patients with tuberculosis: drug interactions, toxicity, and immune reconstitution inflammatory syndrome. J Infect Dis. 2007. 196:suppl 1. S63–S75.

6. Cheng VC, Ho PL, Lee RA, Chan KS, Chan KK, Woo PC, et al. Clinical spectrum of paradoxical deterioration during antituberculosis therapy in non-HIV-infected patients. Eur J Clin Microbiol Infect Dis. 2002. 21:803–809.

7. Orlovic D, Smego RA Jr. Paradoxical tuberculous reactions in HIV-infected patients. Int J Tuberc Lung Dis. 2001. 5:370–375.
8. Cheng VC, Yam WC, Woo PC, Lau SK, Hung IF, Wong SP, et al. Risk factors for development of paradoxical response during antituberculosis therapy in HIV-negative patients. Eur J Clin Microbiol Infect Dis. 2003. 22:597–602.

9. Nicolls DJ, King M, Holland D, Bala J, del Rio C. Intracranial tuberculomas developing while on therapy for pulmonary tuberculosis. Lancet Infect Dis. 2005. 5:795–801.

10. Safdar A, Brown AE, Kraus DH, Malkin M. Paradoxical reaction syndrome complicating aural infection due to Mycobacterium tuberculosis during therapy. Clin Infect Dis. 2000. 30:625–627.

11. Hejazi N, Hassler W. Multiple intracranial tuberculomas with atypical response to tuberculostatic chemotherapy: literature review and a case report. Infection. 1997. 25:233–239.

12. Marais BJ, Gie RP, Schaaf HS, Beyers N, Donald PR, Starke JR. Childhood pulmonary tuberculosis: old wisdom and new challenges. Am J Respir Crit Care Med. 2006. 173:1078–1090.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download