Abstract
Purpose
To provide a systematic review with meta-analysis for addressing the relationship between fecal bile acids (FBAs) and colorectal cancer.
Materials and Methods
Electronic databases were searched for all observational studies that examined the relationship between FBAs and colorectal cancer or adenoma, and calculated weighted mean difference (WMD) and 95% confidence interval (CI). Publication bias was assessed with funnel plot.
Results
Twenty case-control or cohort studies were identified. All studies were pooled to assess the relationship between total FBAs and cancer/adenoma of the large bowel, however, no association was seen (WMD 0.61 mg/g freeze-dried feces; 95% CI: - 0.35 - 1.57). Significantly increased concentration of chenodeoxycholic acid (CDCA) was seen while pooling to assess the relationship between CDCA and cancer/adenoma of the large bowel (WMD 0.13 mg/g freeze-dried feces; 95% CI: 0.01 - 0.25), especially for colorectal cancer (WMD 0.28 mg/g freeze-dried feces; 95% CI: 0.10 - 0.46). However, no significant differences in deoxycholic acid (DCA), lithocholic acid (LCA), and primary and secondary bile acids, were seen between patients with cancer and patients with matched controls regardless of fixed and random effects models.
Epidemiological and experimental studies both in vivo and in vitro suggest that fecal bile acids (FBAs) may play a role in the etiology of colorectal cancer.1-4 It has previously been shown by Hill et al,1 in England and Reddy and Wynder5 in the United States that the mean concentration of total FBAs in patients with colon cancer were higher than those in control subjects, however, further studies failed to demonstrate similar results, raising some doubts over the proposed implication of bile acids.6,7
Large bowel carcinogenesis is a multistage process involving the formation and growth of the adenoma, development of increasingly severe epithelial dysplasia, and finally the progression to malignancy; this process is referred to as the adenoma-carcinoma sequence.8 In other words, colorectal adenomas are well-established precursor lesions for colorectal cancer. Then, the value of individual bile acids as a potential risk marker for colorectal cancer can be further evaluated by study of FBA profiles in patients carrying colorectal adenoma. For bile acid metabolism, many studies reported that patients with colorectal adenoma also had an increased proportion of DCA in their feces.5,9 However, these studies have been limited by small sample size. A meta-analysis may provide a more precise understanding of the true effect. Here, we performed a meta-analysis of all eligible studies in order to address the relationship between FBAs and colorectal cancer or adenoma.
Electronic databases (Pubmed, Embase, Cochrane Controlled Trials Register, Science Citation Index, and Chinese Biomedical Database) were searched up to March 2007 for all observational studies that examined the relationship between bile acids and colorectal cancer or adenoma. For the search, we used both medical subject headings, textwords, and their abbreviations: "bile acid", "cholic acid", "chenodeoxycholic acid", "deoxycholic acid", "lithocholic acid" and "ursodeoxycholic acid" in combination with "colon cancer", "colonic cancer", "rectal cancer", "colorectal cancer", "adenoma", and "adenomatous polyps". Both literature searches were limited to "human" and "English language", except for Chinese in the Chinese Biomedical Database. We also performed a manual search of references cited by the original published studies and relevant review articles. Authors of some identified trials were asked whether they knew of additional studies including unpublished ones.
The contents of abstracts or full-text manuscripts identified through the literature search were reviewed independently by 2 investigators (Tong JL and Shen J) in duplicate to determine whether they met eligibility criteria for inclusion. When discrepancies between investigators occurred for inclusion or exclusion, a third investigator (Ran ZH) was involved to conduct additional evaluation of the study and discrepancies were resolved in conference.
For inclusion in the meta-analysis on the mean concentrations of bile acids and colorectal cancer, studies had to have an analytical design (case-control, cohort, or cross-sectional) and examine the relationship between bile acid concentrations and colorectal cancer or adenoma. Studies were included only if they were published as full-length articles or letters in peer-reviewed journals. All studies were required to have extractable data. Data expressed as medians were not included in the meta-analysis. For total or individual bile acids, data reporting concentrations of bile acids in fecal water were also not included. For duplicate publications, the smaller dataset was excluded. In all searches, we contacted the authors to obtain the required information when relevant information was not reported or there was doubt about duplicate publications.
All data were independently abstracted in duplicate by 2 investigators (Tong JL and Shen J) using a standardized data collection form. Discrepancies were resolved by discussing with a third investigator (Ran ZH). Study characteristics recorded were as follows: first author's name, year and source of publication, country of origin; inclusion, exclusion criteria, outcomes, number enrolled, mean age in each group, percentage of females, number of control case groups, mean levels of total bile acids, CDCA, DCA, LCA, and primary and secondary bile acids.
In the case of trials with more than 2 groups, and dichotomous outcomes, both the number of events and total number of patients would be halved; for continuous outcomes, only the total number of participants would be halved.
Some of the studies included in our meta-analysis differed in the unit used for reporting levels of total bile acids (µmol/g vs. mg/g). Therefore, we converted all units to mg/g using the conversion factor 1 µmol/g = 0.385 mg/g for total FBAs.
We calculated the WMD and 95% CI for all variables. The inverse variance method was used to weight the studies. A fixed-effects model approach was used but in case of heterogeneity, a random-effects model was used. We assessed heterogeneity with I2, which describes the percentage of total variation across studies because of heterogeneity rather than chance. Negative values of I2 are put equal to 0. I2 lies between 0% (no observed heterogeneity) and 100%. I2 values of 50% and more indicate a substantial level of heterogeneity. The heterogeneity between groups (cancer and adenoma) was also calculated using chi-squared test and significance was set at p < 0.10. For subanalysis, we calculated the WMD and 95% CI by geographical location (Europe, Asia, North America, and other continents) and lesions (cancer vs. adenoma). Publication bias was assessed with funnel plot. Begg and Egger tests were also performed. All analyses were performed with the statistical package Stata (ver. 9, Stata Corp., College Station, TX, USA) using the "metan" and "metabias" commands. For forest plots, the size of the box for each study represents the weight of the study in the meta-analysis. The lines around the point estimate represent the 95% CI for the individual studies. The diamonds represent summary estimates from the meta-analysis; the width of the diamond is the 95% CI.
The bibliographical search resulted in 941 hits. Of these studies, only 19 investigated the relationship between FBAs and colorectal cancer or adenoma. In addition to this, 1 study was identified in the Chinese Biomedical Database. Finally, 20 studies including a total of 1,226 individuals fulfilled our inclusion criteria. The flowchart of reviews showed the detailed process of selection (Fig. 1). Of the articles included, 18 were case-control1-3,10-24 and 2 cohort designed.25,26 Among the 20 studies, 7 were conducted primarily in the United Kingdom, 4 in Japan, 2 in France, 2 in Germany, 1 in the United States, 1 in Finland, 1 in Northern Ireland, 1 in Greece, and 1 in China. Table 1 summarizes the characteristics of the 20 trials included in the review. Table 2 shows the Q-statistics and I2 statistics for the overall analyses and compared the results of random effects to fixed effects models.
Nineteen studies reported extractable data about the relationship between total FBAs and cancer/adenoma of the large bowel. No association was seen (WMD 0.61 mg/g freeze-dried feces; 95% CI: - 0.35 - 1.57) in a random effects model (p < 0.01, χ2 test; I2 = 86.0%). When those studies were divided by lesion (cancer vs. adenoma) in order to explain the heterogeneity existed, the heterogeneity existed. In a random effects model, patients with large bowel cancer had a non significant higher concentration of total bile acids (WMD 0.43 mg/g freeze-dried feces; 95% CI: - 0.83 - 1.69) (p < 0.1, χ2 test; I2 = 88.5%) (Fig. 2). Under fixed effects model, the fecal excretion of total bile acids was significantly higher in patients with adenoma than in controls (WMD 0.66 mg/g freeze-dried feces; 95% CI: 0.08 - 1.24), but this difference was no longer significant when based on random effects models (WMD 1.13 mg/g freeze-dried feces; 95% CI: - 0.25 - 2.51).
Five studies reported the relationship between CDCA and cancer/adenoma of the large bowel. No heterogeneity existed about CDCA (p > 0.1, χ2 test; I2 = 33.7%). Significantly increased concentration of CDCA was seen by a fixed effects model when all studies were pooled to assess the relationship between CDCA and cancer/adenoma of the large bowel (WMD 0.13 mg/g freeze-dried feces; 95% CI: 0.01 - 0.25). The fecal excretion of CDCA was significantly higher in patients with large bowel cancer than in matched controls (WMD 0.28 mg/g freeze-dried feces, 95% CI: 0.10 - 0.46) in a fixed effects model (Fig. 3), and also with random effects models (WMD 0.28 mg/g freeze-dried feces; 95% CI: 0.09 - 0.48). However, no differences existed between patients with adenoma and controls (WMD 0.00 mg/g freeze-dried feces; 95% CI: - 0.17 - 0.17) by a fixed/random effects model.
All studies were pooled to assess the relationship between fecal DCA and cancer/adenoma of the large bowel. DCA excretion in patients with cancer/adenoma was not significantly different compared to corresponding controls (WMD 0.24 mg/g freeze-dried feces; 95% CI: - 0.43 - 0.91; random effects model). DCA excretion in patients with cancer was significantly different compared to corresponding controls under fixed effects models (WMD 0.33 mg/g freeze-dried feces; 95% CI: 0.10 - 0.57) (Fig. 4), but the significance was lost with random effects models (WMD 0.01 mg/g freeze-dried feces; 95% CI: - 0.86 - 0.88). However, statistical heterogeneity was present (p < 0.01, χ2 test; I2 = 89.2%). DCA excretion in patients with adenoma on admission was significantly higher than in patients with corresponding controls under fixed effects models (WMD 0.69 mg/g freeze-dried feces; 95% CI: 0.18 - 1.20). There was no heterogeneity existed (p > 0.01, χ2 test; I2 = 56.1%).
LCA excretion in patients with cancer was significantly higher than in patients with corresponding controls under fixed effects models (WMD 0.30 mg/g freeze-dried feces; 95% CI: 0.07 - 0.52) (Fig. 5), and no significance exists between patients with adenoma and patients with corresponding controls. All studies were pooled to assess the relationship between fecal LCA and cancer/adenoma of the large bowel. LCA excretion in patients with cancer/adenoma was nonsignificantly higher than in patients with corresponding controls (WMD 0.61 mg/g freeze-dried feces; 95% CI: - 0.03 - 1.24) under random effects model.
Primary bile acids in patients with cancer/adenoma were slightly higher than in patients with matched controls, but little differences were seen (WMD 0.20 mg/g freeze-dried feces; 95% CI: - 0.10 - 0.51) (random effects model) (Fig. 6). For secondary bile acids, no significance was seen between patients with cancer and patients with matched controls regardless of fixed and random effects models (Fig. 7).
For sub analysis, we calculated the WMD and 95% CI by geographical location. In Europe, there was no difference between patients with cancer/adenoma and patients with matched controls. However, total bile acids excretion in patients with cancer/adenoma was slightly higher than in patients with matched controls in Asia, although no significance was seen. There was only 1 study investigating the relationship in North America that showed significantly higher level of total bile acids in patients with cancer/adenoma compared to matched controls. In the sensitivity analysis, we excluded the studies conducted by Meance et al.,17 which contained probiotics in the diet. The concentration of total bile acids had no significant changes.
For total bile acids excretion, no evidence of publication bias was observed as indicated by a symmetric funnel plot and a non-significant Begg test (p = 0.47) and Egger test (p = 0.23) (Fig. 8).
Colorectal cancer is the third most common cancer in both men and women, and is the second leading cause of cancer deaths.27 Investigators have identified several risk factors that increase a person's chance of developing colorectal cancer, such as age, diet, large intestinal polyps, family history of colon cancer, medical conditions, lack of exercise, obesity, diabetes, smoking, familial adenomatous polyposis, Gardner's syndrome, etc.28 Among these risk factors, observational evidence to relate fecal bile acids and risk of colorectal cancer/adenoma is abundant, however, these studies reported contradictory conclusions.
Therefore, we performed a meta-analysis of all eligible studies in order to address the relationship between FBAs and colorectal cancer or adenoma. The time-related analysis also suggested that FBA concentrations are not an important risk factor for carcinoma unless they are greater than 9 mg/g of feces.21 The finding of this analysis suggests no association between total FBAs and cancer/adenoma of the large bowel, regardless of being based on fixed (WMD 0.14 mg/g freeze-dried feces; 95% CI: - 0.19 - 0.47) and random effects models (WMD 0.61 mg/g freeze-dried feces; 95% CI: - 0.35 - 1.57). However, there was significant heterogeneity (p < 0.01, χ2 test; I2 = 86.0%). Adjustment for clinically relevant confounders in these studies makes this possibility less likely but does not completely eliminate it. Our meta-analysis also showed that the fecal excretion of CDCA was significantly higher in patients with cancer/adenoma than in controls (WMD 0.13 mg/g freeze-dried feces; 95% CI: 0.01 - 0.25), especially for colorectal cancer (WMD 0.28 mg/g freeze-dried feces; 95% CI: 0.10 - 0.46). However, no differences existed between patients with adenoma and controls (WMD 0.00 mg/g freeze-dried feces; 95% CI: - 0.17 - 0.17). In vivo, CDCA markedly enhanced tumor growth and increased vascularization via the COX-2 pathway.29
Animal model experiments indicate that DCA and LCA act as colon tumor promoters of an established large bowel animal carcinogen.30,31 For fecal excretion of DCA and LCA, significantly increased concentrations of DCA and LCA were seen under fixed effects models [(WMD 0.40 mg/g freeze-dried feces; 95% CI: 0.18 - 0.61) and (WMD 0.32 mg/g freeze-dried feces; 95% CI: 0.12 - 0.53), respectively]. However, the significance was lost with random effects models [(WMD 0.24 mg/g freeze-dried feces; 95% CI: - 0.43 - 0.91) and (WMD 0.61 mg/g freeze-dried feces; 95% CI: - 0.03 - 1.24), respectively]. There was also significant heterogeneity. For the sum of primary and secondary bile acids, no significances were seen although there was no heterogeneity. Secondary bile acids have been found to be mutagenic and promote tumor growth in animal models, and the feces of populations with a low risk of colonic cancer contain relatively low proportions of secondary bile acids.32 Furthermore, it has been shown that the proportion of secondary bile acids, namely LCA and DCA, is a far better marker for colorectal cancer.
LCAs and DCAs are the product of 7α-dehydroxylation of CDCA and cholic acids. Cholic acid is mainly derived from endogenous cholesterol whereas CDCA is synthesized mainly from dietary cholesterol.33,34 Some studies demonstrated that Americans who consume a mixed Western diet are, a high risk population and excreted high levels of bile acids compared to Japanese, Chinese, and American Seventh-Day Adventists, who are at low risk.35,36 We purposed that diet patterns have a definite influence upon bile acids metabolism.
Furthermore, many studies also reported the ratio of LCA/DCA, and suggested that the ratio of LCA/DCA may be an important discriminant marker for susceptibility to colorectal cancer.37 The LCA/DCA ratio was significantly higher in the colorectal cancer group compared to the control group.14 Another interesting feature has emerged from some studies that relate the LCA/DCA ratio to the excretion of total FBAs, LCA/DCA×FBA index showing a positive correlation with colorectal cancer.12
Many factors may contribute to the discrepancy in results of observational studies. Firstly, wide variations in the excretion of bile acids in feces have been reported between individuals and from day-to-day within the same individual. Variations in bile acid metabolism might mainly be influenced by age, transmit time, hepatic function, liver metastases, use of medication, gall bladder function, and undergoing previous cholecystectomy and bowel surgery. Secondly, methodological aspects including selection of subjects, period of feces collection, and chemical analysis of either total feces are of great influence. Thirdly, FBA profiles are complex because of bacterial deconjugation, dehydroxylation, oxidoreduction, and desulphation of bile acids in the intestine.
This meta-analysis has several strengths and limitations. Although funnel plot and formal testing did not indicate publication bias, bias cannot definitely be ruled out because of the small number of studies and the low power of any test to detect publication bias. There was evidence of heterogeneity concerning the outcomes of total bile acids, DCA, and LCA. Adjustment for clinically relevant confounders in these studies makes this possibility less likely but does not completely eliminate it. One limitation of our study is the lack of data from multiple large trials. Furthermore, to some extent, the techniques used for FBA determination, which represent little advance since their development in the mid 1960s, can be criticized for lacking in specificity and being incapable of detecting trace quantities of the types of compounds proposed as carcinogens or cocarcinogens. Furthermore, the definition of the sum of secondary bile acids is different; some studies included DCA and LCA which others included DCA, LCA, and ursodeoxycholic acid. Nevertheless, the detailed composition of the sum of primary bile acids in each study is consistent.
In conclusion, by showing differences between the bile acid profiles of patients with colorectal adenomas or carcinomas and matched controls, we provided further support for the concept that bile acids have a role to play in the development of large bowel tumors. The present findings also raise possibility that the biochemical analysis of fecal CDCA might be useful in screening populations for high and low risk in developing carcinoma of the colon.
Figures and Tables
Fig. 2
Summary estimates of the WMD for total bile acids concentration in individuals with colorectal cancer/adenoma vs. matched controls under random effects model. CI, confidence interval; WMD, weighted mean difference.

Fig. 3
Summary estimates of the WMD for CDCA concentration in individuals with colorectal cancer/adenoma vs. matched controls under fixed effects model. CI, confidence interval; WMD, weighted mean difference; CDCA, chenodeoxycholic acid.

Fig. 4
Summary estimates of the WMD for DCA concentration in individuals with colorectal cancer/adenoma vs. matched controls under random effects model. CI, confidence interval; WMD, weighted mean difference; DCA, deoxycholic acid.
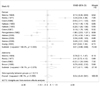
Fig. 5
Summary estimates of the WMD for LCA concentration in individuals with colorectal cancer/adenoma vs. matched controls under random effects model. CI, confidence interval; WMD, weighted mean difference; LCA, lithocholic acid.

Fig. 6
Summary estimates of the WMD for primary bile acids concentration in individuals with colorectal cancer/adenoma vs. matched controls under fixed effects model. CI, confidence interval; WMD, weighted mean difference.

Fig. 7
Summary estimates of the WMD for secondary bile acids concentration in individuals with colorectal cancer/adenoma vs. matched controls under fixed effects model. CI, confidence interval; WMD, weighted mean difference.
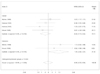
Fig. 8
Begg's funnel plot with pseudo 95% confidence limits showing WMD in total bile acids by standard error of WMD. WMD, weighted mean difference.
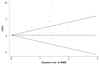
Table 1
General Characteristics of Included Studies which Assessed the Relationship between Fecal Bile Acids and Colorectal Cancer or Adenoma
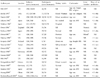
CRC, colorectal cancer; HS, healthy subjects; BW, body weight; NI, Northern Ireland; CC, colon cancer; CRA, colorectal adenoma; PU, peptic ulcer; NGD, non-gastrointestinal disease; AP, adenomatous polyps; NR, not reported.
*Containing a diet with probiotics.
†Including patients with liver metastases.
ACKNOWLEDGMENTS
We thank Drs ZY Zhang and X Chen for their helpful suggestions and critical reading.
References
1. Hill MJ, Drasar BS, Williams RE, Meade TW, Cox AG, Simpson JE, et al. Faecal bile-acids and clostridia in patients with cancer of the large bowel. Lancet. 1975. 1:535–539.
2. Bayerdörffer E, Mannes GA, Richter WO, Ochsenkühn T, Wiebecke B, Köpcke W, et al. Increased serum deoxycholic acid levels in men with colorectal adenomas. Gastroenterology. 1993. 104:145–151.

3. Debruyne PR, Bruyneel EA, Karaguni IM, Li X, Flatau G, Müller O, et al. Bile acids stimulate invasion and haptotaxis in human colorectal cancer cells through activation of multiple oncogenic signaling pathways. Oncogene. 2002. 21:6740–6750.

5. Reddy BS, Wynder EL. Metabolic epidemiology of colon cancer. Fecal bile acids and neutral sterols in colon cancer patients and patients with adenomatous polyps. Cancer. 1977. 39:2533–2539.

6. Mudd DG, McKelvey ST, Norwood W, Elmore DT. Carcinoma of the large bowel and faecal bile acids. Br J Surg. 1979. 66:355.
7. Murray WR, Backwood A, Trotter JM, Calman KC, MacKay C. Faecal bile acids and clostridia in the aetiology of colorectal cancer. Br J Cancer. 1980. 41:923–928.

8. Morson B. President's address. The polyp-cancer sequence in the large bowel. Proc R Soc Med. 1974. 67:451–457.
9. Mudd DG, McKelvey ST, Norwood W, Elmore DT, Roy AD. Faecal bile acid concentration of patients with carcinoma or increased risk of carcinoma in the large bowel. Gut. 1980. 21:587–590.

10. Hikasa Y, Tanida N, Ohno T, Shimoyama T. Faecal bile acid profiles in patients with large bowel cancer in Japan. Gut. 1984. 25:833–838.

11. Makino T. Fecal bile acid excretion in patients with colon cancer, colon polyp and peptic ulcer. Tokai J Exp Clin Med. 1984. 9:297–305.
12. Owen RW, Henly PJ, Thompson MH, Hill MJ. Steroids and cancer: faecal bile acid screening for early detection of cancer risk. J Steroid Biochem. 1986. 24:391–394.

13. Kaibara N, Sasaki T, Ikeguchi M, Koga S, Ikawa S. Fecal bile acids and neutral sterols in Japanese with large bowel carcinoma. Oncology. 1983. 40:255–258.

14. Owen RW, Dodo M, Thompson MH, Hill MJ. Fecal steroids and colorectal cancer. Nutr Cancer. 1987. 9:73–80.
15. Murray WR, Backwood A, Trotter JM, Calman KC, MacKay C. Faecal bile acids and clostridia in the aetiology of colorectal cancer. Br J Cancer. 1980. 41:923–928.
16. Korpela JT, Adlercreutz H, Turunen MJ. Fecal free and conjugated bile acids and neutral sterols in vegetarians, omnivores, and patients with colorectal cancer. Scand J Gastroenterol. 1988. 23:277–283.

17. Meance S, Boutron-Ruault MC, Myara A, Gerhardt MF, Marteau P, Lavergne A, et al. Fecal primary bile acids and serum cholesterol are associated with colorectal adenomas. Dig Dis Sci. 2003. 48:1751–1757.
18. Owen RW, Day DW, Thompson MH. Faecal steroids and colorectal cancer: steroid profiles in subjects with adenomatous polyps of the large bowel. Eur J Cancer Prev. 1992. 1:105–112.
19. Breuer NF, Jaekel S, Dommes P, Goebell H. Fecal bile acids in patients with adenomatous polyps of the colon. Case-control study. Digestion. 1986. 34:87–92.

20. Haines A, Hill MJ, Thompson MH, Owen RW, Williams RE, Meade TW, et al. A prospective study of faecal bile acids and colorectal cancer. Eur J Cancer Prev. 2000. 9:317–323.

21. Hill MJ, Melville DM, Lennard-Jones JE, Neale K, Ritchie JK. Faecal bile acids, dysplasia, and carcinoma in ulcerative colitis. Lancet. 1987. 2:185–186.
22. Perogambros A, Legakis NJ. Faecal bile acids in patients with colon cancer. Zentralbl Bakteriol Mikrobiol Hyg [B]. 1982. 176:346–348.
23. Breuer NF, Dommes P, Jaekel S, Goebell H. Fecal bile acid excretion pattern in colonic cancer patients. Dig Dis Sci. 1985. 30:852–859.

24. Tanida N, Hikasa Y, Shimoyama T, Setchell KD. Comparison of faecal bile acid profiles between patients with adenomatous polyps of the large bowel and healthy subjects in Japan. Gut. 1984. 25:824–832.
25. Huang JG, Yu JP, Shen ZX. The metabolism feature of fecal bile acids in patients with colorectal cancer. Anthology Med. 2000. 19:429–431.
26. Boutron-Ruault MC, Marteau P, Lavergne-Slove A, Myara A, Gerhardt MF, Franchisseur C, et al. Effects of a 3-mo consumption of short-chain fructo-oligosaccharides on parameters of colorectal carcinogenesis in patients with or without small or large colorectal adenomas. Nutr Cancer. 2005. 53:160–168.

27. American Cancer Society. Colorectal Cancer Facts & Figures. Statistics for 2005. Accessed June 14, 2005. Available at:
http://www.cancer.org/downloads/STT/CAFF2005CR4PWSecured.pdf.
28. Sandler RS. Epidemiology and risk factors for colorectal cancer. Gastroenterol Clin North Am. 1996. 25:717–735.

29. Soma T, Kaganoi J, Kawabe A, Kondo K, Tsunoda S, Imamura M, et al. Chenodeoxycholic acid stimulates the progression of human esophageal cancer cells: A possible mechanism of angiogenesis in patients with esophageal cancer. Int J Cancer. 2006. 119:771–782.
30. Reddy BS, Mastromarino A, Wynder EL. Further leads on metabolic epidemiology of large bowel cancer. Cancer Res. 1975. 35:3403–3406.
31. Narisawa T, Magadia NE, Weisburger JH, Wynder EL. Promoting effect of bile acids on colon carcinogenesis after intrarectal instillation of N-methyl-N'-nitro-N-nitrosoguanidine in rats. J Natl Cancer Inst. 1974. 53:1093–1097.
32. Kishida T, Taguchi F, Feng L, Tatsuguchi A, Sato J, Fujimori S, et al. Analysis of bile acids in colon residual liquid or fecal material in patients with colorectal neoplasia and control subjects. J Gastroenterol. 1997. 32:306–311.

33. Ayaki Y, Tsuma-Date T, Endo S, Ogura M. Role of endogenous and exogenous cholesterol in liver as the precursor for bile acids in rats. Steroids. 1981. 38:495–509.
34. Gustafsson BE, Angelin B, Einarsson K, Gustafsson JA. Effects of cholesterol feeding on synthesis and metabolism of cholesterol and bile acids in germfree rats. J Lipid Res. 1977. 18:717–721.
35. Reddy BS, Weisburger JH, Wynder EL. Effects of high risk and low risk diets for colon carcinogenesis on fecal microflora and steroids in man. J Nutr. 1975. 105:878–884.

36. Reddy BS, Wynder EL. Large-bowel carcinogenesis: fecal constituents of populations with diverse incidence rates of colon cancer. J Natl Cancer Inst. 1973. 50:1437–1442.

37. Kamano T, Mikami Y, Kurasawa T, Tsurumaru M, Matsumoto M, Kano M, et al. Ratio of primary and secondary bile acids in feces: possible marker for colorectal cancer? Dis Colon Rectum. 1999. 42:668–672.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download