Abstract
Purpose
This study was undertaken to investigate the outcomes associated with docetaxel treatment of Korean patients with hormone-refractory prostate cancer (HRPC) and to compare its clinical efficacies in 1st and 2nd-line settings.
Materials and Methods
This study was retrospectively performed and included 47 patients with HRPC. The 1st-line group consisted of 19 patients who had not undergone prior chemotherapy, and the 2nd-line group consisted of 28 patients who underwent prior chemotherapy. All patients were treated with 75 mg/m2 IV docetaxel every 3 weeks and 5 mg of prednisone twice daily with a continuous androgen blockade.
Results
Of 47 study subjects, 14 patients (29.8%) had ≥ 50% PSA decline from baseline. PSA response was more common in the 1st-line group, but this was not statistically different (42.1% vs. 21.4%, p = 0.114). After a median follow up of 11 months (range, 6 - 24 months), the 1st-line group showed a longer time to PSA progression (4 vs. 2 months, p = 0.015) and survival (17 vs. 10 months, p = 0.037) than the 2nd-line group. In terms of toxicities, no difference was apparent between the 2 groups.
Prostate cancer is the second most common cause of cancer-related deaths in men in the United States and its occurrence is rapidly increasing in Korea.1,2 Early-stage prostate cancer can be cured by radical surgery or radiation therapy, but many newly diagnosed patients have advanced stage prostate cancer.3 In 1941, Huggins and Hodges first reported the efficacy of androgen deprivation therapy in advanced prostate cancer.4 Subsequently, androgen deprivation treatment became the most effective systemic approach for patients with metastatic disease. Although 80 - 90% of patients initially respond favorably to this treatment, all patients, however, eventually develop "hormone-refractory prostate cancer (HRPC)", which is unresponsive to androgen deprivation.5,6 Unfortunately, treatment for HRPC is limited and some forms of chemotherapy have been shown to provide a palliative effect, but no survival gain.7-10
Two recent phase III trials showed that docetaxel plus estramustine or prednisone improved overall survival versus mitoxantrone plus prednisone.7,8 Subsequently, docetaxel was strongly advocated as a standard treatment for metastatic HRPC. Currently, docetaxel is administrated to HRPC patients in Korea, but no report on clinical outcomes of docetaxel therapy in our country has been published. We, therefore, undertook this study to investigate the outcomes of docetaxel for the treatment of HRPC in Korean patients, and to compare its clinical efficacies in 1st and 2nd-line settings.
From January 2005 through September 2007, 47 patients who had received docetaxel chemotherapy for the treatment of HRPC were enrolled in this study. Patient records were retrospectively reviewed to determine the base-line characteristics of patients and the clinical efficacy and tolerability of docetaxel. All patients had histologically confirmed adenocarcinoma of the prostate, evidence of metastasis, and progressive disease despite complete androgen blockade therapy, anti-androgen withdrawal, and an Eastern Cooperative Oncology Group (ECOG)-Performance Status of 0 to 2. Progressive disease was defined by an increase in PSA levels as determined by 2 consecutive measurements at least 2 weeks apart, an increase in the size of a measurable lesion by computed tomography (CT) or any newly developed bony metastasis with hot uptake by bone scan. Bone scan was considered stable if there were no new lesions in 2 scans at least two months apart. Androgen suppression was confirmed by serum testosterone measurements. Informed consent was obtained prior to each therapy. To investigate differences according to prior chemotherapy, patients were classified into 2 groups; the 1st-line group consisted of patients who had undergone no prior chemotherapy, whilst the 2nd-line group had undergone prior chemotherapy. The 1st-line therapy for each HRPC patient in this study was determined at physician's discretion, based on cancer-related symptoms, rising PSA, extent of metastasis and performance status.
Pretreatment evaluation included a complete medical history-taking, a physical examination, complete blood cell count, serum chemistry profile, serum PSA, bone scan, CT of the pelvis and abdomen, and chest X-ray. Patients were treated with 75 mg/m2 IV docetaxel every 3 weeks and 5 mg of prednisone twice daily, following premedication with 8 mg of dexamethasone. Patients who had not undergone orchiectomy were required to continue androgen blockade with a luteinizing hormone-releasing hormone (LHRH) analogue. Patients underwent physical examination, CBC, LFT and renal function test before docetaxel administration, and 7 days after each docetaxel administration. Patients were followed up by using 3 weekly PSA determinations before docetaxel administration. In patients with measurable disease, tumor assessments were performed every 3 cycles until progression or sooner, if possible. Visual analogue pain scale (VAS) was also routinely applied during each docetaxel cycle. Chemotherapy was continued until disease progression or unacceptable adverse events occurred. All patients received this docetaxel treatment as an in-patient each cycle.
All patients were evaluated for PSA response, objective measurable disease response, subjectivepain response, time to PSA progression, and survival. In particular, we investigated differences between the clinical outcomes of the 1st and 2nd-line groups.
The criteria used for determining response were based on the guidelines of the PSA working group.9 A PSA decline of ≥ 50%, confirmed by a second value at least 3 weeks later, was considered as a PSA response. Additionally, stable disease was defined as a PSA decrease, which did not satisfy PSA response criteria. Progression was defined as the increase of PSA on the contrary. Baseline PSA was defined as the PSA value obtained within a 2-week period prior to starting the study medication.
The start of the time to PSA progression was the day when treatment was initiated. If at least 50% decline of PSA has been achieved, end date was the time when PSA has increased of 50% above the nadir at a minimum of 5 ng/mL. For patients that did not experience a PSA decrease of this magnitude (or no decrease), the end point for progression was calculated as the time of 25% increase in baseline or nadir PSA. All end dates required a confirmatory PSA test. Overall survival was defined as the time between first docetaxel administration and death.
Objective response was documented using evaluable radiographs according to the Response Evaluation Criteria of Solid Tumors (RECIST).10 For bone metastasis, stable disease was defined if there were no new lesions in two bone scans taken at least 2 months apart. Subjective pain responses were measured using the VAS. Pain relief was defined as a decline of ≥ 2 points in VAS scores of at least 1-month duration versus baseline scores.
The National Cancer Institute Common Toxicity Criteria version 2.0 was used to evaluate patients for toxicity during each cycle. If Grade 3 or 4 hematologic or non-hematologic toxicities were observed during any cycle, the docetaxel dose was then temporarily deescalated to 75% of the original dose for following treatment cycles until recovery, and a reescalated dose was then recommended. If the same toxicity reappeared at any time, the reduced dose was maintained throughout.
The major statistical endpoints of this study consisted of PSA response, time to PSA progression, and overall survival. We also investigated differences between these endpoints in 1st and 2nd-line groups. Time to PSA progression and survival curves were produced using the Kaplan-Meier method and differences between the 1st and 2nd-line groups were compared using the log-rank test. The T test (or Mann-Whitney test for non-parametric variables) was used for continuous variables, and the Chi-square (or Fisher's exact test for non-parametric variables) was used for categorical variables. P values of < 0.05 (2-sided) were considered statistically significant, and confidence intervals were set at the 95% level. All analyses were performed using the Statistical Package for the Social Sciences for Windows Ver. 11 (SPSS Inc, Chicago, IL, USA).
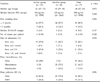
The baseline characteristics of the 47 patients are listed in Table 1. The median pretreatment PSA level was 180 ng/mL (range, 12 - 8788 ng/mL), and there was no significant difference between the baseline PSA levels of the 1st and 2nd-line groups. In terms of visceral metastases, 2 patients had lung lesions, 1 patient had a liver lesion and another patient had a brain lesion. Most patients had bone or LN metastasis. In terms of the subgroup analysis, 19 patients received docetaxel as the 1st-line chemotherapy, and 28 as the 2nd-line chemotherapy. Of these 28 patients, 21 had previously received mitoxantrone and 7 had received 280 mg estramustine. In addition, 8 of the 28 2nd-line chemotherapy patients (28.6%) had previously received palliative radiation. However, none of the 2nd-line chemotherapy patients had received any cytotoxic drug or radiotherapy during the month preceding the study period.
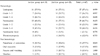
Of the 47 study subjects, 14 (29.8%) experienced a PSA decline of ≥ 50% from baseline that had lasted for ≥ 4 weeks, which constituted PSA response. PSA response was more frequently demonstrated in the 1st line group (42.1% vs. 21.4%), but this was not significant (p = 0.128). Stable disease and progression disease were presented by 18 (38.3%) and 15 (31.9%) of the study subjects, respectively (Table 2).
Twenty-nine study subjects had measurable metastasis, revealed by radiographic examinations, which included CT and MRI; i.e., lung in 2, liver in 1, brain in 1, and LN plus bone in 25 patients. Of evaluable these 29 patients, one patient with brain lesions achieved complete response (CR) and 2 patients with lung and 1 patient with LN lesions achieved partial response (PR). Objective response including CR and PR appeared in 3 (23.1%) in the 1st-line and only one patient (6.3%) in the 2nd-line, which did not show any significant difference (p = 0.299).
Of the 30 evaluable study subjects, 16 (53.3%) symptomatic patients showed an improvement in VAS pain scores of 2 points versus baseline pain scores, over a period of at least 2 months. Whereas 8 of 16 patients with symptomatic improvement had an accompanying decrease in PSA, the other 8 demonstrated only pain improvement without a PSA decline or objective response. No difference in subjective pain response was observed between the 2 groups (data not shown).
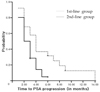
Given a median follow-up of 11 months (range, 6 - 24 months) for all study subjects, 42 patients ultimately experienced PSA progression despite therapy. Moreover, no difference in mean follow-up duration was observed between the two groups (11 months in the 1st-line group vs. 9 months in the 2nd-line group, p = 0.798). Only 1 patient showed a continuously decreasing serum PSA level over 9 months after docetaxel administration. He received docetaxel in a 1st-line setting and had bone metastasis; his baseline PSA level was 98 ng/mL. Median time to progression for study subjects was 3.0 months (range, 1 - 14 months). At the time of analysis, 23 were remained alive and 24 patients died of prostate cancer. Median survival was 12.0 months (range, 3 - 24 months). The 1st-line group showed the longer median time to PSA progression (4.0 vs. 2.0 months, p = 0.015) and survival (17 months vs 10 months, p = 0.037) than the 2nd-line group. Time to PSA progression and the overall survival curve are presented in Figs. 1 and 2, respectively.
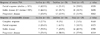
Toxicity findings are summarized in Table 3. In terms of hematologic toxicities, neutropenia and leukopenia were common, and were found in 27 (57.4%) and 28 (59.6%), respectively, but no difference was apparent between the 2 groups (57.9% vs 57.1% for leukopenia, p = 0.959; and 68.4% vs 53.6% for neutropenia, p = 0.309). Grade 3 - 4 neutropenia occurred in 19 patients (40.4%), which showed no difference between the two groups (47.4% vs 35.7%, p = 0.424). Dose reduction was required temporarily in 19 patients (40.4%) due to hematologic toxicities, and most recovered within 2 weeks. Of these, 12 patients required granulocyte-colony stimulating factor (GCSF) and 5 patients were maintained at 75% of the original dose because of repetitive hematologic toxicities. Grade 3 neutropenic fever occurred in 2 patients who recovered with supportive care that included hydration and antibiotics. In terms of non-hematologic toxicities, grade 1 to 2 sensory neuropathies, such as paresthesia of the extremities, were most frequently found in 13 patients (27.7%). However, no patient developed a grade 3 - 4 non-hematologic toxicity, and all patients who developed a non-hematologic toxicity recovered with conservative treatment.
Docetaxel is considered as a promising agent because of its excellent experimental results in vitro and its theoretical background. The studies to evaluate the ability of docetaxel to stabilize tubulin, found that it had a significant anti-tumor effect in androgen-dependent and androgen-independent prostate cancer cell lines.11,12 In addition, docetaxel caused apoptosis by inducing phosphorylation of bcl-2, which found to be overexpressed in androgen-resistant prostate cancer.13 Thus, these in vitro results encouraged the clinical use of docetaxel in HRPC patients. In 2004, 2 randomized trials, TAX 327 and the Southwest Oncology Group (SWOG) 99 - 16 trial, showed for the first time a survival benefit for docetaxel in men with metastatic HRPC.7,8 Specifically, median overall survival in the TAX 327 trial was improved by 2.4 months in the docetaxel (administered every 3 weeks) arm versus the mitoxantrone arm (also administered every 3 weeks) (18.9 vs. 16.5 months, resp., p = 0.009), which led the US FDA in 2005 to approve docetaxel as chemotherapeutic agent in HRPC patients.7
In the present study, the PSA response rate for all study subjects was 21%, which was lower than those found in two landmark studies (45% in TAX 327 and 50% in SWOG 99 - 16), which may have been due to different patient characteristics. Our patients had a median baseline PSA level of ca. 180ng/mL, which was substantially higher than those of previous studies; i.e., 114 ng/mL in TAX 327 and 90 ng/mL in SWOG 99 - 16. Moreover, our study included more patients who had received prior chemotherapy than previous studies. When subgroup analysis was performed in the 1st-line group, PSA response rate increased to 42.1%. Moreover, our median survival was 12 months (95% confidence interval, 9.75 - 16.25 months), which was somewhat lower than those of the 2 above-mentioned landmark trials. Because our study was limited by the small number patients enrolled and its retrospective nature, we were unable to identify the cause of poor response rate to docetaxel chemotherapy by comparing to previous trials. However, in these previous trials, patients received docetaxel as 1st-line chemotherapy, whereas most of our patients were heavily pretreated as mentioned above; i.e., 31.9% had received palliative radiation and 59.6% prior chemotherapy, such as, mitoxantrone or estramustine. Therefore, the start of docetaxel treatment was usually late in the present study, and these patient characteristics could well explain the differences between these previous studies and present study in terms of clinical outcomes, such as PSA response, time to PSA progression, and overall survival.
A few studies have examined outcomes of docetaxel chemotherapy in Asian countries, especially as a 2nd-line treatment.14,15 Thus, it is worth noting that the present study is the first to be conducted on the efficacy of docetaxel in Korean patients, and that it included patients with progressive disease despite prior chemotherapy; i.e., mitoxantrone-resistant and estramustine-resistant cases. A small number of studies conducted in the West have evaluated PSA response rates after cross over from mitoxantrone to docetaxel and vice versa. However, reported PSA response rates, palliation efficacies, and tolerabilities were variable and dependent on disease extent, treatment duration, and patient performance status.16-18
In the present study, docetaxel was generally tolerable, and no patient was lost due to toxicity. Leukopenia, neutropenia, and paresthesia of the extremities were the predominant side effects, and the hematologic toxicity was comparable to that reported previously.7,8 Furthermore, patients well tolerated 2nd-line docetaxel, and its toxicities were comparable to those of 1st-line treatment.
No standard chemotherapy has yet been established for Korean HRPC patients. The Korean FDA also approved docetaxel for the treatment of HRPC in 2005, and therefore, docetaxel is actively being administrated to many patients throughout Korea. However, no clinical report has yet been published on the clinical efficacy of docetaxel chemotherapy in Korean HRPC patients. Two docetaxel regimens could be suggested; i.e., docetaxel plus prednisone or estramustine. In the SWOG 99 - 16 trial, median overall survival was better for docetaxel plus estramustine than mitoxantrone plus prednisone. However, docetaxel plus estramustine was associated with more frequent incidents of cardiovascular and thromboembolic toxicities.8 In view of these side effects together with the fact that the estramustine combination has no survival benefit, we would recommend 75 mg/m2 docetaxel (3 weekly) plus prednisone, because of its effectiveness and acceptable toxicity in Korean HRPC patients.
The optimal timing of docetaxel chemotherapy is an issue that should be considered. However, no prospective clinical trial has indicated whether early treatment is more effective than delayed treatment. Some experts in the field recommended that mitoxantrone plus prednisone with palliative radiation therapy should be offered to the patients with a slow PSA doubling time and asymptomatic disease should be observed, that patients with a slow PSA doubling time and symptomatic bone-only disease, and that patients with a rapid PSA doubling time and/or symptomatic disease and/or visceral metastases should be treated with a docetaxel-based chemotherapy.19-21 Recently, docetaxel has strongly been recommended as a 1st-line treatment in our institution for HRPC patients with a rapidly increasing PSA or symptomatic metastasis.
Although our 2 study groups were comparable in terms of patient characteristics (including baseline PSA), our study is intrinsically limited by its retrospective nature. Furthermore, the fact that the 1st-line therapy for HRPC patients was determined at physician's discretion is an another limitation. Docetaxel was administrated to patients with symptomatic metastatic HRPC, which meant that time to docetaxel treatment was greater than in previous studies. Therefore, the selection bias could exist, thus making us to perform cross-study comparisons.
In conclusion, docetaxel in a 1st-line setting was found to be effective and tolerable in Korean HRPC patients. 2nd-line docetaxel was also found to have tolerable toxicity, but its efficacy was limited. Nevertheless, additional multi-institutional studies are required to obtain a meaningful result concerning the survival benefits of docetaxel in Korean HPRC patients.
Figures and Tables
Fig. 1
Times to PSA progression in the 1st and 2nd-line groups (p = 0.015). PSA, prostate-specific antigen.
References
1. Greenlee RT, Hill-Harmon MB, Murray T, Thun M. Cancer statistics, 2001. CA Cancer J Clin. 2001. 51:15–36.

2. Park SK, Sakoda LC, Kang D, Chokkalingam AP, Lee E, Shin HR, et al. Rising prostate cancer rates in South Korea. Prostate. 2006. 66:1285–1291.

3. McLeod DC. Hormonal therapy in the treatment of carcinoma of the prostate. Cancer. 1995. 75:Suppl 7. 1914–1919.

4. Huggins C, Hodges CV. Studies on prostatic cancer: I. the effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostate. CA Cancer J Clin. 1972. 22:232–240.

5. Crawford ED, Eisenberger MA, McLeod DG, Spaulding JT, Benson R, Dorr FA, et al. A controlled trial of leuprolide with and without flutamide in prostatic carcinoma. N Engl J Med. 1989. 321:419–424.

6. Eisenberger MA, Blumenstein BA, Crawford ED, Miller G, McLeod DG, Loehrer PJ, et al. Bilateral orchiectomy with or without flutamide for metastatic prostate cancer. N Engl J Med. 1998. 339:1036–1042.

7. Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et al. TAX 327 Investigators. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cacner. N Engl J Med. 2004. 351:1502–1512.

8. Petrylak DP, Tangen CM, Hussain MH, Lara PN Jr, Jones JA, Taplin ME, et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med. 2004. 351:1513–1520.

9. Scher HI, Eisenberger M, D'Amico AV, Halabi S, Small EJ, Morris M, et al. Eligibility and outcomes reporting guidelines for clinical trials for patients in the state of a rising prostate-specific antigen: recommendations from the Prostate-Specific Antigen Working Group. J Clin Oncol. 2004. 22:537–556.

10. Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000. 92:205–216.
11. Kreis W, Budman DR, Calabro A. Unique synergism or antagonism of combinations of chemotherapeutic and hormonal agents in human prostate cancer cell lines. Br J Urol. 1997. 79:196–202.

12. Díaz JF, Andreu JM. Assembly of purified GDP-tubulin into microtubules induced by taxol and taxotere: reversibility, ligand stoichiometry, and competition. Biochemistry. 1993. 32:2747–2755.

13. Haldar S, Basu A, Croce CM. Bcl2 is the guardian of microtubule integrity. Cancer Res. 1997. 57:229–233.
14. Miyoshi Y, Uemura H, Nakamura M, Hasumi H, Sugiura S, Makiyama K, et al. Treatment of androgen-independent, hormone-refractory prostate cancer with docetaxel in Japanese patients. Int J Clin Oncol. 2005. 10:182–186.

15. Akaza H, Moore MA, Chang SJ, Cheng C, Choi HY, Esuvaranathan K, et al. The 5th conference on Asian Trends in prostate cancer hormone therapy. Asian Pac J Cancer Prev. 2007. 8:3–12.
16. Joshua AM, Nordman I, Venkataswaran R, Clarke S, Stockler MR, Boyer MJ. Weekly docetaxel as second line treatment after mitozantrone for androgen-independent prostate cancer. Intern Med J. 2005. 35:468–472.

17. Michels J, Montermurro T, Murray N, Kollmannsberger C, Nguyen Chi K. First- and second line chemotherapy with docetaxel or mitoxantrone in patients with hormone-refractory prostate cancer: does sequence matter? Cancer. 2006. 106:1041–1046.
18. Berthold DR, Sternberg CN, Tannock IF. Management of advanced prostate cancer after first-line chemotherapy. J Clin Oncol. 2005. 23:8247–8252.

19. Calabrò F, Sternberg CN. Current indications for chemotherapy in prostate cancer patients. Eur Urol. 2007. 51:17–26.

20. Pienta KJ, Smith DC. Advances in prostate cancer chemotherapy: a new era begins. CA Cancer J Clin. 2005. 55:300–318. quiz 323-5.

21. Mendiratta P, Armstrong AJ, George DJ. Current standard and investigational approaches to the management of hormone-refractory prostate cancer. Rev Urol. 2007. 9:Suppl 1. S9–S19.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download