Abstract
Purpose
This study examined the rate of degeneration of acetabular cartilage by the bipolar head according to time, and also which clinical factors are related to the degeneration of acetabular cartilage.
Materials and Methods
Among 192 patients (226 hip joints) who received bipolar hemiarthroplasty from August 1996 to August 2002, 61 patients (65 hip joints) were enrolled in this study, who were followed up for more than 2 years and showed no signs of dislocation, infection, or functional problems. A modified form of a computer assisted vector wear analysis program was used to measure the rate of degeneration of the acetabular cartilage. The factors that appeared to affect the rate of acetabular degeneration in the two groups was evaluated.
Results
The average linear degenerative change in the acetabular cartilage and the volumetric degenerative change were 0.23 ± 0.107 mm/year and 114 ± 47.2 mm3/year, respectively. The result showed significant differences in activity and HHS between the 2 groups. The HHS showed a reverse relationship with the linear degeneration and volumetric degeneration, and the activity showed a correlation with the linear and volumetric degeneration.
Conclusion
The acetabular cartilage degenerates faster as the patient' activity increases, and slower with a higher HHS. When surgeons perform hip joint arthroplasty, it is strongly recommended that the life expectancy and the level of activity should be considered when deciding between a hemiarthroplasty and total hip arthroplasty.
One of major mechanisms of failure after bipolar hemiarthroplasty is the migration of the metal head to the inside of pelvis as the acetabular articular cartilage degenerates. Generally, such complications have been reported to be caused by excessive pressure delivered on cartilage and abrasion caused by the friction of the bipolar metal cup and the acetabular cartilage.1-4 Degeneration of the acetabular articular cartilage by such mechanism has been reported in animal experiments or histologically during revision arthroplasty.5 However, studies radiologically measuring the degeneration rate of the acetabular articular cartilage in patients who underwent bipolar hemiarthroplasty and maintained the function well have not yet been reported. The purpose of this study was to examine the degeneration rate of the acetabular articular cartilage caused by the artificial bipolar metal cup with time, and to characterize clinical factors mediating an effect on the degeneration of the acetabular articular cartilage.
Of 192 patients who underwent bipolar hemiarthroplasty at our department from August 1996 to August 2002 (226 hip joints), the study was performed on 61 patients (65 hip joints) who were available for the minimum 2 years follow up, without showing dislocation, infection and functional problems. The male to female ratio of patients was 26 to 35, average age at the time of surgery was 68.7 years (53 - 88 years), and weight average was 55.4 kg. The follow-up period was average of 51.2 months (24 - 96 months). The causality of surgery was femoral neck or intertrochanteric fracture in 57 cases, and avascular necrosis of femoral head in 8 cases. In the cases of avascular necrosis of femoral head, only those cases that the disease level was early (Ficat stage I) and thus considered to be almost without change of the acetabular articular cartilage were included. Surgery was performed by the first author employing posterolateral approach. In all patients, extensively porous coated Anatomic Medullary Locking femoral stem (AML, DePuy, Warsaw, IN, USA) and the Self-centering bipolar head with an outer diameter of 39 - 53 mm and inner diameter of 28 mm (DePuy, Warsaw, IN, USA) were used. As the artificial femoral head, ceramic femoral heads (DePuy) 28 mm in diameter were used. In determining the size of the outer diameter of Bipolar cup, a size corresponding to patient`s femoral head was used, if it concurred to the measured value, and the next smaller size bipolar cup was used for the cases when corresponding size patient's femoral heads were absent.
Clinical as well as radiological evaluation was performed on all subjects immediately after surgery and annually afterward. The Harris Hip Score (HHS) was examined as clinical evaluation, and the presence or absence of loosening was assessed by examining and analyzing radiographs taken during the follow ups as radiological test. To accurately measure the acetabular cartilage degeneration, the anteroposterior images of the bilateral hip joint taken immediately and during annual follow ups were scanned onto a computer using the Powerlook 2001XL flat bed imaging scanner (Umax Data Systems, Inc., Taipei, Taiwan), and rendered using a computer assisted vector wear analysis program developed by Martell et al. at the University of Chicago (University of Chicago, Orthopedic Surgery, Hip analysis program version 4.0).6 From immediately after surgery, the degeneration of the acetabular articular cartilage was measured annually. The measurement methods were based on the border of the acetabular bone instead of the acetabular cup of hip arthroplasty, however, the acetabular bony margin was used instead of the acetabular cup of total hip arthroplasty since the acetabular cup is not a perfect circle on the anteroposterior radiographs. Because the shape of the acetabulum is not spherical, three points that could be observed through the AP x-ray findings were selected: the acetabular superior-outer margin, inferior-inner margin, and the point where the line that vertically bisects the line that connects the acetabular superior-outer and inferior-inner margin meets the acetabular bony margin. The Hip analysis program calculated the circle that passes through these 3 points, and the artificial femoral head was measured by the corresponding lateral aspect of the bipolar cup (Fig. 1). To prevent interobserver variation, each case was measured by a single investigator 3 times, and the mean values were used (Fig. 2). In each individual, there was a difference between estimated volumetric wear and true volumetric wear, depending on the size of acetabular fossa, however, it was impossible to measure each estimated volumetric wear. Therefore, we tried to consider the tendency of wear.
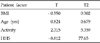
Based on the measured results, the subjects were divided into the group whose degeneration was higher than the average value and the group lower than the average value, and Body mass index (BMI), which was thought to influence degeneration, age, activity, and HHS were compared and analyzed by Student T-test. In addition, the contribution level of each factor influencing degenerative changes was analyzed by linear regression analysis. The correlation of pain and HHS was examined by correlation analysis. In the case of activity, it was divided into 5 levels according to the hip sheet of the Anderson Clinic6 (Table 1). Statistical analysis was performed by SPSS (Ver. 9.1).
The average level of the linear degeneration of all patients was measured to be 0.23 ± 0.107 mm/year, and the average volumetric degeneration level was measured to be 114 ± 47.2 mm3/year. Regarding the direction showing degeneration, the average acute angle formed by the line connecting both ischial tuberosity was found to be 74.91 ± 17.66 degrees. There was no significant intraobserver variation (p < 0.05). The subjects were divided into groups whose degeneration was higher than the average value and the group lower than the average value, and the values were compared and analyzed statistically. It was found that p value of body mass index was 0.694 and 0.611 in linear and volumetric degeneration, respectively, and a statistically significant difference was not detected. Similarly, age was 0.169 and 0.436, respectively, and a statistically significant difference was not detected.
On the other hand, activity was 0.005 and 0.598, respectively, and a statistically significant difference in linear degeneration was detected. Nevertheless, a statistically significant difference was not detected in volumetric degeneration. HHS was 0.009 and 0.008, respectively, and a statistically significant difference in the linear and volumetric wear and degeneration was detected (Tables 2 and 3). In analysis of contribution level of each factor to degeneration of the acetabular articular cartilage, the T-score of activity was 2.315 and a correlation was detected, in linear degeneration, and the T-score of HHS was - 8.812, and a statistically significant reverse correlation was detected. In addition, the T-score of HHS in volumetric degeneration was - 7.177, and a statistically significant correlation was detected. Finally, the T-score of activity was 3.301, and their correlation was confirmed (Tables 4 and 5).
The degeneration of the acetabular articular cartilage after bipolar hemiarthroplasty could be diverse, depending on the material of artificial joints, lubrication level, friction coefficient, direction and strength of the delivered force, activity pattern, sliding distance, etc.8 In addition, it is influenced by various clinical factors of patients, and it is accurately difficult to distinguish and measure the contribution level of each factor. Degenerative change of acetabular articular cartilage after hemiarthroplasty in numerous animal studies has already been reported.9-11 According to these animal studies, the hard bipolar cup in the histological degeneration process of the acetabular articular cartilage delivers abnormal stress to the articular cartilages, resulting in the increase of secretion of degenerative enzymes. These enzymes hydrolyse converted to lysosomal enzymes,5,12 which induces the loss of initial glucosaminoglycan, thus changing the biomechanical property of articular cartilages, softening them, and causing them to lose elasticity.13
This process destroys surface collagen fibers within the lamina splender and induces the initial loss of the surface intergrity.14 It has been shown that such changes of biomechanical strength of cartilage continues to gradually destroy cartilages. McGibbon et al. concluded that acetabular cartilage degeneration explained, in part, by repetitive stress after hemiarthroplasty,15 and Dalldorf et al. found that the progression in the severity of the degeneration after hemiarthroplasty correlated directly with the duration of articulation of the implant with the acetabulum.16 Such degeneration of articular cartilages becomes the cause of migration of the artificial metal bipolar cup through the acetabular articular cartilages that is a major cause of the failure of bipolar hemiarthroplasty. Since the measured degeneration rate of the acetabular cartilage in approximately 0.23 mm/year, and the mean thickness of the acetabular articular cartilage is 1.0 - 3.3 mm according to the study by Kurrat et al.,17 1.1 - 1.8 mm according to Athanasiou et al.,18 and 1.0 - 3.6 mm according to Eckstein et al.,19 it is thought that all acetabular cartilages would show degeneration approximately 7 - 8 years after surgery, and the abrasion of the acetabular bone would be initiated and the risk of protrusion would be increased. Nonetheless, such estimated outcomes vary, depending on many factors that influence the degeneration of articular cartilages, and thus it could not be considered accurate. Furthermore, in regard to factors involved in the degeneration of acetabular cartilages, the fact that the higher the HHS, the slower the degeneration was found. Therefore, the high score of HHS was associated with pain (89.7% correlation within 1% error range), and thus, more degeneration of cartilage. As pain was increased more actively, the degeneration of the acetabular cartilage occurred more rapidly. Hence, it is thought that total arthroplasty may be preferable in active patients, instead of hemiarthroplasty. In other words, it is thought that, considering the life expectancy and activity of patients who require hip arthroplasty, it could be determined whether to perform total arthroplasty or hemiarthroplasty, and the time to convert to total arthroplasty after bipolar hemiarthroplasty could be predicted by radiologically measuring the degeneration rate of the acetabular articular cartilage.
After bipolar hemiarthroplasty, the average linear degeneration change of the acetabular articular cartilage was measured to be 0.23 ± 0.107 mm/year, and the average volumetric degeneration change was 114 ± 47.2 mm3/year. The degeneration of the acetabular articular cartilage was faster in active patients and slower in patients with high HHS. In hip arthroplasty, it is thought to be preferable to choose bipolar hemiarthroplasty or total hip arthroplasty by considering the above results and the life expectancy as well as activity of patients. Studies with more cases and approaches from diverse angles are needed in future.
Figures and Tables
Fig. 1
The image shows how to calculate the acetabular cartilage degeneration. The acetabular bony margin was used instead of the acetabular cup of total hip arthroplasty. Because the shape of the acetabulum is not spherical, three points that could be observed through the AP x-ray findings were selected: the acetabular superior-outer margin, inferior-inner margin and the point where the line that vertically bisects the line that connects the acetabular superior-outer and inferior-inner margin meets the acetabular bony margin. The wear program calculated the circle that passes through these three points.

Fig. 2
Image showing the wear analysis procedure, known as the 'Hip 32' (Computer assisted vector wear analysis system, University of Chicago Ortho. Ver. 4.0).7

References
1. D'Arcy J, Devas M. Treatment of fractures of the femoral neck by replacement with the Thompson prosthesis. J Bone Joint Surg Br. 1976. 58:279–286.
2. Harris WH, Rushfeldt PD, Carlson CE, Scholler JM, Mann RW. The hip Society. Pressure distribution in the hip and selection of hemi-arthroplasty. The Hip: Proceedings of the Third Open Scientific Meeting of the Hip Society. 1975. St. Louis: CV Mosby;93–98.
3. Hinchey JJ, Day PL. Primary prosthetic replacement in fresh femoral-neck fractures. A review of 294 consecutive cases. J Bone Joint Surg Am. 1964. 46:223–240.
4. Jensen JS, Holstein P. A long term follow-up of Moore arthroplasty in femoral neck fractures. Acta Orthop Scand. 1975. 46:764–774.

5. Ehrlich MG, Mankin HJ, Jones H, Grossman A, Crispen C, Ancona D. Biochemical confirmation of an experimental osteoarthritis model. J Bone Joint Surg Am. 1975. 57:392–396.

6. von Knoch M, Sychterz CJ, Engh CA Jr, Engh CA Sr. Incidence of late bead shedding from uncemented porous coated cups. A radiographic evaluation. Clin Orthop Relat Res. 1997. 342:99–105.
7. Ebramzadeh E, Sangiorgio SN, Lattuada F, Kang JS, Chiesa R, Mckellop HA, et al. Accuracy of measurement of polyethylene wear with use of radiographs of total hip replacements. J Bone Joint Surg Am. 2003. 85A:2378–2384.

8. Schmalzried TP, Shepherd EF, Dorey FJ, Jackson WO, dela Rosa M, Fa'vae F, et al. The John Charnley Award. Wear is a function of use, not time. Clin Orthop Relat Res. 2000. 381:36–46.
9. Cruess RL, Kwok DC, Duc PN, Lecavalier MA, Dang GT. The response of articular cartilage to weight-bearing against metal. A study of hemiarthroplasty of the hip in the dog. J Bone Joint Surg Br. 1984. 66:592–597.

10. Minihane KP, Turner TM, Urban RM, Williams JM, Thonar EJ, Sumner DR. Effect of hip hemiarthroplasty on articular cartilage and bone in a canine model. Clin Orthop Relat Res. 2005. 437:157–163.

11. van der Meulen MC, Beaupré GS, Smith RL, Giddings VL, Allen WA, Athanasiou KA, et al. Factors influencing changes in articular cartilage following hemiarthroplasty in sheep. J Orthop Res. 2002. 20:669–675.

12. Ehrlich MG, Mankin HJ, Jones H, Wright R, Crispen C, Vigliani C. Collagenase and collagenase inhibitors in osteoarthritic and normal cartilage. J Clin Invest. 1977. 59:226–233.

13. Kempson GE, Muir H, Pollard C, Tuke M. The tensile properties of the cartilage of human femoral condyles related to the content of collagen and glycosaminoglycans. Biochim Biophys Acta. 1973. 297:456–472.

14. Freeman MA. The pathogenesis of primary osteoarthrosis: An hypothesis. Mod Trends Orthop. 1972. 6:40–94.
15. McGibbon CA, Krebs DE, Trahan CA, Trippel SB, Mann RW. Cartilage degeneration in relation to repetitive pressure: case study of a unilateral hip hemiarthroplasty patient. J Arthroplasty. 1999. 14:52–58.
16. Dalldorf PG, Banas MP, Hicks DG, Pellegrini VD Jr. Rate of degeneration of human acetabular cartilage after hemiarthroplasty. J Bone Joint Surg Am. 1995. 77:877–882.

17. Kurrat HJ, Oberländer W. The thickness of the cartilage in the hip joint. J Anat. 1978. 126:145–155.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download