Abstract
Purpose
The aim of the study was to assess perinatal outcome of pregnancy burdened with maternal addiction in comparison with an unselected population from a European transition country.
Materials and Methods
Data on pregnancies complicated by illicit drug abuse (n = 85) managed during a 10-year period (1997 - 2007) at Split University Hospital were analyzed. Data on the type of drug, course of gestation and labor, and on perinatal outcome were considered. Data on all non-dependence pregnancies recorded during the study period were used as a control group.
Results
During the study period, there were 85 dependence-complicated pregnancies (0.2%). Use of heroin alone during pregnancy was recorded in 51 women (50%), methadone alone in 6 (7%), and a combination of heroin and methadone in 9 (11%). Premature delivery was significantly more common in the group of pregnant addicts (21% vs. 6%); 49% of pregnant addicts were carriers of hepatitis C virus (HCV) and 14% of hepatitis B virus (HBV). Neonatal abstinence syndrome developed in 61 infants (7%) born to addicted mothers. There were 4 cases (4.6%) of early neonatal death; 7 neonates had 5-minute Apgar score ≤ 7 (8%); 29 neonates had low birth weight for age (33%); and 7 neonates had congenital anomalies (8%). The risk of various congenital anomalies was 3-fold in the group of children born to addicted mothers.
Substance abuse has crossed social, economic, and geographical borders, and remains one of the major problems that modern society is facing worldwide. The prevalence of substance abuse in young adults of both genders has increased markedly over the past 20 years. Nearly 90% of drug-abusing women are of childbearing age.1 However, the exact number of drug-dependent women is unknown because the statistics relies heavily on voluntary patient disclosure.2 Some women tend to keep the use of illicit drugs from gynecologists for fear of stigmatization and discrimination, therefore, the symptoms induced by maternal dependence cannot always be recognized.3 In addition, it is difficult to identify the proportion of pregnancies in addicts terminated by spontaneous or induced abortion.4 The number of heroin addicts of fertile age in Croatia has been estimated to be 4,500, of which some 250 give birth to 1 child per year.3 Heroin alone or in combination with methadone has been used during the past decade by approximately 80% of addicted mothers in Croatia and worldwide.3,5 In 80% of cases, opiate addicts take at least 1 more drug or psychoactive substance along with heroin and more than 50% suffer from psychiatric comorbidity.3 Major health problems associated with high-risk lifestyle observed in non-pregnant illicit opiate users are also observed in pregnant users. These include poor nutritional habits, increased incidence of infectious and sexually transmitted diseases, other substance abuse, and poor antenatal care.6 These factors are likely to contribute to an increased risk of obstetric complications including placental insufficiency, miscarriage and intrauterine death, and neonatal morbidity.6-8 In utero drug exposure can have a severe impact on not only the development of the fetus but also the child later in life.9 Perinatal death, prematurity, fetal growth retardation, neonatal abstinence syndrome (NAS), and a wide variety of other perinatal complications have been frequently observed in the offspring of heroin-addicted women but it is unclear how much these effects are due to fetal heroin exposure or to generally poor health and limited prenatal care in these women.6,10-13
We analyzed drug abuse during pregnancy in the Split-Dalmatia County, Croatia. The purpose of the study was to compare perinatal outcome between heroin-exposed and unexposed pregnancies in a European transition country where heroin alone or with methadone is a predominant illicit drug in not only the population of pregnant women but also society in general.
In this retrospective cohort study, data on heroin, methadone, and polydrug addicted pregnant women admitted for delivery to the university Department of Obstetrics and Gynecology, Split University Hospital, in Split, Croatia, during a 10-year period were analyzed. During the study period from January 1, 1997, to January 1, 2007, there were 43,181 deliveries with 43,529 newborns, including 371 twin pregnancies (0.860%) and 5 triplet pregnancies (0.0116%). Stillbirths were excluded because there was no such case in the study group of addiction pregnancies. Records of 85 pregnant women with 86 neonates (1 twin pregnancy) found to have usedillicit drugs during pregnancy were selected from the maternal and neonatal files kept at the department. In 62 subjects (73%), testing was performed after they admitted drug addiction during pregnancy, delivery, or after delivery. Data on the type of drug, course of gestation and labor, and overall perinatal outcome were considered. Gestational age was calculated from the onset of the last menstruation and corrected according to ultrasonography (US) finding when the difference exceeded 1 week. In children born to addicted mothers, urine toxicology (Abbott Laboratories Diagnostics Division, IL, USA) for dependence substances, 5-minute Apgar score, and NAS score according to Finnegan were performed.14 Our own standards were used to evaluate fetal growth from birth weight according to gestational age and maternal parity and by use of ponderal index (PI (g/cm3) = weight (g) × 100/length (cm3).15,16
The data obtained were compared with a control group that included all non-addicted women admitted for delivery during the study period (n = 43,096) and their newborns (n = 43,529).
Statistical data analysis was performed using SPSS 10 statistical software, t-test, Mann-Whitney test for quantitative data, and χ2-test and odds ratio for qualitative data. The level of statistical significance was set at p < 0.05.
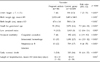
During the 10-year study period, there were 85 addiction pregnancies (0.2%) with 86 newborns (0.2%). General characteristics of both study and control groups of pregnant women and their pregnancies are shown in Table 1.
In the study group of 85 pregnant addicts, heroin was used by 51 (60%), methadone alone by 6 (7%), and a combination of heroin and methadone by 9 (11%). Of other dependence substances, benzodiazepines in combination with heroin and/or methadone were most commonly used, as reported by 15 women (19%) (Table 2).
Data obtained on the course of labor, labor complications, and sexually transmitted diseases in the study and control group of women showed statistically significant differences. Statistically significant between-group differences were observed in all parameters assessed except for the rate of premature rupture of membranes (PROM; p = 0.448), rate of cesarean section (p = 0.122), gestational age at delivery (p = 0.509), and gestational age at preterm delivery (p = 0.304). Preterm delivery was significantly more frequent in the group of addicted women (21% vs. 6%), yielding a relative risk of 3.45 (Table 3).
Neonatal outcome data showed that newborns of lower vitality were born more frequently to addicted mothers. In these newborns, the risk of Apgar score < 7 was 6-fold that of the control group.
Children born to addicted mothers generally had lower birth weight with a 7-fold risk of small for gestational age (SGA) newborns. The risk of various congenital anomalies was 4-fold in the group of children born to addicted mothers. Congenital cardiac defects were most common, including ventriculoseptal defect in 3 cases, and transposition of great vessels and hypoplastic left heart in 1 case each. Other anomalies included small intestine malrotation, polydactyly, and single umbilical artery in 1 case each. In the neonates born to addicted mothers, the risk of intracranial hemorrhage was 6-fold, of early neonatal sepsis caused by Streptococcus agalactiae 8-fold, and of early neonatal death 11-fold that of the control group (Table 4).
Five newborns died in the first week of life, 2 from asphyxia and prematurity, 2 from cardiac defect, and 1 from early neonatal sepsis (Table 5). In the children born to addicted mothers, the length of hospital stay was approximately 50% longer than in the control group children. NAS developed in 61 neonates (71%) born to addicted mothers with variation in manifestation according to the substance of abuse taken by the mother; i.e. heroin, methadone, heroin and methadone, or some other dependence substances (Table 5).
The results of the study indicated a 0.2% prevalence of addicted pregnant women in the area during the 10-year study period. The actual number of addicts is always several times greater than the number of those identified, however, detection of addicted women is additionally hampered by their tendency to conceal and deny the problem. It has been estimated that some 900 opiate addicts present for the first ever treatment per year in Croatia with a 1 : 1 ratio of treated to untreated addicts, yielding an incidence of 1,800 cases per year since 1997, 400 of them female.3
In the present study, drug addiction was demonstrated by positive urine toxicology for dependence substances. In 62 subjects (73%) study, testing was performed after they admitted drug addiction during pregnancy, delivery, or after delivery. In the remaining 23 women (27%), toxicology testing was indicated by the neonate behavior indicative of maternal drug addiction. According to the Republic of Croatia legislative, testing for dependence substances can be performed without the patient's consent, however, it may be limited in daily routine by the Act on Patient Rights, according to which the patient's informed consent should be obtained prior to any medical procedure including toxicological screening for dependence substances.17 We are fully aware that a certain proportion of neonates born to mothers concealing their drug addiction have thus been unrecognized, evading target pediatric surveillance. Croatia has a properly developed system of treatment of pregnant addicts.18,19 Within the frame of this Croatian model, methadone and buprenorphine therapy is easily available to pregnant addicts and they are encouraged to get regular general medical check-ups and prenatal gynecologic care in case of HCV infection in particular.18 Nevertheless, this model of treatment, now considered to be the gold standard for its favorable impact on perinatal outcome, was used by only 6 pregnant women on a voluntary basis in the present study.20-22
In our study, pregnant addicts mostly declared to be primiparae (n = 78) but the possibility of a number of addiction-burdened pregnancies having terminated prematurely by induced or spontaneous abortion should be taken in consideration, as also reported elsewhere.4 In spite of appropriate treatment modalities available during pregnancy, pregnant addicts failed to take due care of their health, so that 65% of them had a suboptimal number of gynecologic examinations, 41% underwent less than 3 US studies, and 20% had inadequate body weight gain as a direct consequence of poor nutritional status. Such a poor level of care for one's own health is characteristic of both heroin addicts and those continuing on heroin along with methadone therapy.20 In 1977, Connaughton et al. showed that pregnant addicts exclusively on methadone therapy had a mean of 8.2 antenatal examinations whereas those that continued using heroin along with methadone therapy had only 1.8 antenatal examinations, because of their uninterrupted high-risk lifestyle.23
In the present study, the rates of maternal HCV (49%) and HBV (16%) carriage were consistent with those found in Croatian injecting drug users, and comparable with those reported elsewhere.24,25 Although the rate of HCV vertical transmission is known to be very low as demonstrated by studies in an Australian population (3%), it eventually poses a risk of long-term morbidity and mortality.26 We found no case of human immunodeficiency virus (HIV) infection in our study population of pregnant addicts. Croatia still has a low level of HIV epidemic, with relatively stable epidemiological trends in recent years. Although there is a large having a high number of heroin injecting addicts, estimated to be more than 10,000, systematic HIV testing of injecting drug users seeking treatment shows a very low prevalence of HIV infection (< 1%) since 1991. The risk of HIV outbreak has been estimated as moderate, in part owing to the primary and secondary prevention actions launched for years.24
In spite of the fact that polydrug use in pregnancy contributes to the higher prevalence of perinatal complications such as placental hemorrhage, more than 90% of our pregnant addicts had vaginal delivery. It should be noted that there was no case of abruptio placentae, which may have been due to the relatively small sample of pregnant addicts (n = 85).27 There was no case of stillbirth either, which could be seen as an unexpected finding considering their high-risk lifestyle that they did not give up during pregnancy. However, there might have been stillbirths among pregnant addicts who kept their addictions to themselves, thus evading identification. Generally, children born to pregnant addicts had a high rate of perinatal morbidity.
Preterm delivery was more common in pregnant addicts, with drug abuse entailing a relative risk of 3.45. Inadequate numbers of clinical and US examinations due to poor care for one's own health and unawareness of the risks associated with their hazardous lifestyles may have contributed to the increased prevalence of premature deliveries. Premature deliveries and SGA are the most common antenatal complications of addiction pregnancies, which can threaten neonatal outcome irrespective of the drug effect.8,12,22,27,28 Although heroin is known to cross the transplacental barrier and is associated with low birth weight infants, we admit that this outcome may be only partly due to the effect of the drug itself and is also likely to be due to associated lifestyle factors such as poor maternal dietary habits, increased rate of maternal infection, and reduced antenatal care attendance.21,22 Furthermore, many investigators report that methadone therapy in pregnant heroin users significantly increases infant birth weight.20,21,29,30 The currently accepted protocol for pregnant heroin users includes methadone therapy which, in combination with antenatal care, results in considerable birth weight improvement.20,23,27 Our results pointed to rather poor acceptance of antenatal methadone therapy.
One-third of our pregnant addicts gave birth to SGA infants, suggesting that the addiction lifestyle is associated with a high risk of retarded fetal growth (RR = 5.103). Our results are consistent with the reports in the literature.13,21,22 Hulse et al. found concurrent use of heroin and methadone to reduce birth mass by 557g, similar to the effect of heroin alone.20 To our knowledge, the type of fetal growth disorders in pregnant addicts has not yet been specifically analyzed. It may seem surprising that the probability of delivering a newborn of low PI as a measure of symmetric growth is identical in pregnant addicts and the general population. Neonates born to pregnant addicts are smaller but not thinner than those born to non-addicts. The factors implicated in fetal growth retardation in pregnant addicts exert their influence throughout gestation and include infections and sexually transmitted diseases, maternal malnutrition and inadequate body weight gain, drug abuse, and overall addict's lifestyle.6,12,20,27 Thus, the early gestational period predominated by cell hyperplasia, medium gestational period with gradual inclusion of hypertrophy in growth determination, and the last trimester predominated by hypertrophy in fetal growth are equally affected.31 Therefore, symmetric growth retardation as seen in pregnant addicts is a logical result of these events.
In our study, children born to addicted mothers had a high prevalence of NAS (71%), mostly in those born to heroin and methadone addicts, which is consistent with literature data.13 This withdrawal syndrome is a constellation of behavioral and physiological signs and symptoms that are remarkably similar despite marked differences in the causative agent properties. The symptoms of NAS include high-pitched crying, irritability, vomiting, diarrhea, and tremor.2,13 Addiction or tolerance is due to passage of the drugs across the transplacental barrier, and this occurs in varying degrees depending on the pharmacokinetic properties of the particular drug. Therefore, disruption of this transplacental passage of drugs at birth results in the development of withdrawal syndrome.2 Based on thorough social and drug history including types of drugs used and data obtained from self-reporting addicted mothers, these newborns were admitted to the Neonatal Intensive Care Unit and observed by experienced staff to detect symptoms of withdrawal, initiate treatment before more severe encephalopathy supervened, and collect urine for toxicology screening. We used Finnegan's scoring system, and pharmacotherapy with phenobarbital was introduced when the average of 3 scores was 8 or more.32,33 Sarkar and Donn report that the management of NAS widely varies with inconsistent policies to determine its presence and treatment.34 There is only 1 randomized trial comparing different types of opioid-based medications for NAS treatment, and management of infants with NAS is still controversial and hampered by the lack of evidence from properly conducted trials.35,36 Phenobarbital is commonly used for the treatment of NAS. We used it at a loading dose followed by 5 mg/kg/day, with dosage increase/decrease according to response in each individual case. Kaltenbach and Finnegan found the loading dose of phenobarbital to reduce the length of treatment if administered as monotherapy.35
The results of our study revealed that children born to pregnant addicts had a higher rate of perinatal hypoxia and diseases unrelated to maternal addiction such as early sepsis caused by Streptococcus agalactiae, intracranial hemorrhage, and congenital anomalies. The high rate of early neonatal sepsis caused by beta-hemolytic streptococcus B (BHSB) is no surprise in neonates born to mothers from high-risk groups. BHSB infection is associated with maternal anorectal and urogenital colonization, chorioamnionitis, premature delivery, and prolonged rupture of fetal membranes.37 Our results showed that none of the pregnant addicts underwent prenatal testing for BHSB. Only 1 pregnant addict with her newborn's blood culture found to be positive for BHSB received intrapartum antibiotic prophylaxis with a single dose of ampicillin. Maternal risk factors for the development of early BHSB infection were present in 6 children (60%), and included intrapartum fever in 4 mothers and prolonged rupture of fetal membranes in 2 mothers. One infant died from early BHSB sepsis on the fourth day of life.
Although opiate abuse is not directly associated with an increased prevalence of cardiac defects, these congenital anomalies were most common in our study population.13,27 Congenital cardiac defects accounted for a significant proportion of neonatal mortality, which was very high in comparison with the control group.
The present study confirmed the problem of addiction in Croatia and pointed to a disturbingly low proportion of pregnant addicts being included in the system of institutional care and surveillance. The study period covered the early postwar period, but, it could only in part explain the low level of institutionalized care for pregnant addicts. The management of this high-risk group requires proper organization as it is time-consuming, uncertain, and expensive. Obviously, additional efforts should be invested in the care for this high-risk group of women because the problem of their addiction is transmitted to their offspring. Children born to addicted mothers are faced not only with withdrawal syndrome but also have a significantly higher risk of neonatal morbidity and mortality.6,13,27 Like other authors, we could not differentiate the direct consequences of drug abuse from a number of other unfavorable medical and social factors closely associated with poor lifestyle and habits of pregnant addicts.20,27 In our setting, methadone therapy as a currently accepted treatment modality for pregnant addicts has not yet taken hold since it was used by 6 women only. We are fully aware that methadone therapy is far from ideal due to the high likelihood of NAS development recorded in 63 - 85% newborns exposed to maternal methadone therapy yet it remains the predominant treatment modality that may improve perinatal outcome by careful drug titration and organized approach in the surveillance and control of addiction pregnancies.13,38 Addicted mothers are aware that the quality of their children's care upon discharge from the maternal ward is questionable, and this issue calls for active involvement of various services; first of all, social welfare institutions. These women tend to keep their addiction secret for fear of being deprived of custody of the child and of their addiction disclosure, which in turn has adverse effects on pregnancy outcome. During the 10-year study period, 5 children born to 3 mothers were placed at a social welfare institution. In these cases, maternal addiction was additionally burdened with psychiatric comorbidity.
An inherent weakness of this study was the self-reported nature of the data. It is difficult to elicit valid information on illicit drug abuse, and under-reporting is a common problem. We believe that patients included in the study were reasonably candid about their self-reported drug abuse because medical record information was confirmed by urine toxicology. Unfortunately, we do not have information on pregnancies delivered elsewhere, however, this is a county hospital and the majority of narcotics users probably gave birth here. We are aware that the real number of narcotics-dependent pregnant women having delivered during the study period must have been considerably higher.
The problem of opiate dependence poses a major problem in our area, and the results of the present study of pregnancy outcome and neonatal fate in this population during the 10-year period point to inadequate systematic organization of care for pregnant addicts with high-risk pregnancy while their newborns suffer from medical and social consequences of maternal addiction. Although there is no ideal treatment modality for pregnant addicts, this vulnerable population group obviously requires systematic and organized care. It is a relatively small but specific group of pregnant women who pose an intriguing perinatological problem due to the high incidence of complications, yet with a potentially successful active approach.
Figures and Tables
References
1. Kuczkowski KM. Anesthetic implications of drug abuse in pregnancy. J Clin Anesth. 2003. 15:382–394.
2. Oei J, Kei L. Management of the newborn infant affected by maternal opiates and other drugs of dependency. J Paediatr Child Health. 2007. 43:9–18.

3. Sakoman S. Care of pregnant women with opioid abuse and of their newborns. Gynaecol Perinatol Suppl. 2006. 15:93–101.
4. Coleman PK, Reardon DC, Rue VM, Cougle J. A history of induced abortion in relation to substance use during subsequent pregnancies carried to term. Am J Obstet Gynecol. 2002. 187:1673–1678.

5. Fabris C, Prandi G, Perathoner C, Soldi A. Neonatal drug addiction. Panminerva Med. 1998. 40:239–243.
6. Hulse GK, Milne E, English DR, Holman CD. Assessing the relationship between maternal opiate use and neonatal mortality. Addiction. 1998. 93:1033–1042.

7. Stone ML, Salerno LJ, Green M, Zelson C. Narcotic addiction in pregnancy. Am J Obstet Gynecol. 1971. 109:716–723.

8. Ostrea EM, Chavez CJ. Perinatal problems (excluding neonatal withdrawal) in maternal drug addiction: a study of 830 cases. J Pediatr. 1979. 94:292–295.

9. Huestis MA, Choo RE. Drug abuse's smallest victims: in utero drug exposure. Forensic Sci Int. 2002. 128:20–30.

10. Olofsson M, Buckley W, Anderson GE, Friis-Hansen B. Investigation of 89 children born by drug-dependent mothers. II. Follow-up 1-10 years after birth. Acta Paediatr Scand. 1983. 72:407–410.
11. Olofsson M, Buckley W, Andersen GE, Friis-Hansen B. Investigation of 89 children born by drug-dependent mothers. I. Neonatal course. Acta Paediatr Scand. 1983. 72:403–406.
12. Rosen TS, Johnson HL. Children of methadone-maintained mothers: follow-up to 18 months of age. J Pediatr. 1982. 101:192–196.

13. Bell GL, Lau K. Perinatal and neonatal issues of substance abuse. Pediatr Clin North Am. 1995. 42:261–281.

14. Finnegan LP, Connaughton JF Jr, Kron RE, Emich JP. Neonatal abstinence syndrome: assessment and management. Addict Dis. 1975. 2:141–158.
15. Roje D, Tadin I, Marušić J, Vulić N, Aračić M, Vučinović M, et al. Birth weights and birth lengths of newborns from the town of Split; the importance of developing own standards. Gynaecol Perinatol. 2005. 14:69.
16. Roje D, Banovic I, Tadin I, Vucinovic M, Capkun V, Barisic A, et al. Gestational age-the most important factor of neonatal ponderal index. Yonsei Med J. 2003. 45:273–280.

17. The patients rights law. 2004. Accessed May 19, 2007. Available from: URL:
http://www.nn.hr/clanci/sluzbeno/.
18. Sakoman S. National strategy on drug abuse control in Republic of Croatia. 1995. Zagreb: Croatian Government Comitee for drug abuse control.
19. Sakoman S. Substance abuse in the Republic of Croatia and National Program for Drug Control. Croat Med J. 2000. 41:270–286.
20. Hulse GK, Milne E, English DR, Holman CD. The relationship between maternal use of heroin and methadone and infant birth weight. Addiction. 1997. 92:1571–1579.

21. Kandall SR, Albin S, Dreyer E, Comstock M, Lowinson J. Differential effects of heroin and methadone on birth weights. Addict Dis. 1975. 2:347–355.
22. Lam SK, To WK, Duthie SJ, Ma HK. Narcotic addiction in pregnancy with adverse maternal and perinatal outcome. Aust N Z J Obstet Gynaecol. 1992. 32:216–221.

23. Connaughton JF, Reeser D, Schut J, Finnegan LP. Perinatal addiction: outcome and management. Am J Obstet Gynecol. 1997. 129:679–686.

24. Matic S, Lazarus JV, Donoghoe MC, editors. HIV/AIDS in Europe: moving from death sentence to chronic disease management. 2006. Copenhagen: WHO Regional Office for Europe.
25. Crofts N, Aitken CK, Kaldor JM. The force of numbers: why hepatitis C is spreading among Australian injecting drug users while HIV is not. Med J Aust. 1999. 170:220–221.

26. Garland SM, Tabrizi S, Robinson P, Hughes C, Markman L, Devenish W, et al. Hepatitis C-role of perinatal transmission. Aust N Z J Obstet Gynaecol. 1998. 38:424–427.
27. Little BB, Snell LM, Klein VR, Gilstrap LC 3rd, Knoll KA, Breckenridge JD. Maternal and fetal effects of heroin addiction during pregnancy. J Reprod Med. 1990. 35:159–162.
28. Thornton L, Clune M, Maguire R, Griffin E, O'Connor J. Narcotic addiction: the expectant mother and her baby. Ir Med J. 1990. 83:139–142.
29. Ellwood DA, Sutherland P, Kent C, O'Connor M. Maternal narcotic addiction: pregnancy outcome in patients managed by a specialized drug-dependency antenatal clinic. Aust N Z J Obstet Gynaecol. 1987. 27:92–98.

30. Stimmel B, Adamsons K. Narcotic dependency in pregnancy. Methadone maintenance compared to use of street drugs. JAMA. 1976. 235:1121–1124.

31. Carrera JM, Devesa R, Serra B. Kurjak A, editor. Classification of intrauterine growth retardation. A textbook of perinatal medicine. 1998. London: Parthenon Publishing;1192–1200.
32. Levy M, Spino M. Neonatal withdrawal syndrome: associated drugs and pharmacologic management. Pharmacotherapy. 1993. 13:202–211.
33. Carin I, Glass L, Parekh A, Solomon N, Steigman J, Wong S. Neonatal methadone withdrawal. Effect of two treatment regimens. Am J Dis Child. 1983. 137:1166–1169.
34. Sarkar S, Donn SM. Management of neonatal abstinence syndrome in neonatal intensive care units: a national survey. J Perinatol. 2006. 26:15–17.

35. Kaltenbach K, Finnegan LP. Neonatal abstinence syndrome, pharmacotherapy and developmental outcome. Neurobehav Toxicol Teratol. 1986. 8:353–355.
36. Langenfeld S, Birkenfeld L, Herkenrath P, Müller C, Hellmich M, Theisohn M. Therapy of the neonatal abstinence syndrome with tincture of opium or morphine drops. Drug Alcohol Depend. 2005. 77:31–36.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download