Abstract
To report a patient who presented with epithelial ingrowth caused by viral keratoconjunctivitis 3 months after LASIK surgery. A 41-year-old man presented with decreased visual acuity in the right eye, which had developed about 3 weeks before. He had undergone LASIK surgery 3 months prior without complications. Two months after the surgery, he was treated for viral conjunctivitis. During the treatment period, filamentary keratitis developed, and a therapeutic bandage contact lens was applied for 2 weeks. Upon presentation, examination revealed a corrected visual acuity of 20/100 and irregular epithelial sheets under the edematous flap. The flap was lifted, and the in-grown epithelium was removed. The flap was repositioned with double continuous 10 - 0 nylon sutures. Post-operatively, the patient developed a mild diffuse lamellar keratitis that resolved rapidly with topical corticosteroid treatment. At 2 months, the corrected visual acuity was 20/20 without interface opacities. As the patient showed no complications prior to viral conjunctivitis, we suspect that the viral infection caused edema of the corneal flap, which caused epithelial ingrowth under the flap. Patients who have viral conjunctivitis after LASIK surgery should be examined carefully and managed with consideration of flap complications.
Laser in situ keratomileusis is the most frequently performed refractive surgical procedure worldwide. It involves the creation of an anterior corneal flap that adheres back into place after laser ablation. Although the flap heals to the posterior stromal bed, histological studies demonstrate a lack of wound repair at the interface 6 months after surgery, which may explain the possibility of late complications involving the flap and interface.1
Epithelial ingrowth is one of the most significant complications of LASIK at the edge of the flap. Reports of the incidence of epithelial ingrowth have ranged from 0 - 20%.2-5 It usually presents in the early post-operative period and is known to be associated with loose epithelium, epithelial defects at the time of surgery, hyperopic LASIK correction, enhancement surgeries, flap instability, and corneal epithelial basement membrane dystrophy.2,4-6 While not always serious, it can progress to induce irregular astigmatism or melting of the overlying flap and threaten the central vision.
Adenoviral keratoconjunctivitis is a common infection responsible for numerous worldwide ocular epidemics. It presents as acute catarrheal conjunctivitis with pseudomembrane formation of varying severity. In about 80% of the cases, keratitis causes groups of swollen epithelium with or without subsequent subepithelial infiltrates.7 We report the case of a patient who presented, 3 months after LASIK surgery, with epithelial ingrowth associated with viral keratoconjunctivitis. As far as we know, this is the first case of delayed epithelial ingrowth associated with viral keratoconjunctivitis.
A 41-year-old man presented with decreased visual acuity in the right eye, which had developed about 3 weeks before. He had undergone LASIK surgery 3 months prior at another clinic without apparent complications. Pre-operatively, manifest refraction was - 1.75 - 0.25 × 180 OD and - 1.00 OS, yielding 20/20 best spectacle-corrected visual acuity (BSCVA) in both eyes.
Two months after the surgery, he was infected with viral conjunctivitis from his 6-year old son and was treated for about 3 weeks at the local clinic. During the treatment period, filamentary keratitis developed. Filaments were mechanically removed, and a therapeutic bandage contact lens was applied to the right eye for 2 weeks.
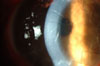
Our examination revealed a corrected visual acuity of 20/100 in the right eye and 20/20 in the left eye. There was an epithelial defect, which involved the temporal one-third of the anterior flap surface OD. The flap was edematous and seemed to be detached from the remaining stromal bed with irregular hazy interface opacities (Fig. 1). Under the edematous flap, a white demarcation line was observed. In the left eye, multiple subepithelial infiltrates were noted.
On his first visit to our clinic, the patient underwent surgery for the interface opacities. Under an operating microscope, an 8-blade marker was used to mark the cornea. The flap was easily elevated, and an epithelial sheet was noted on the stromal side of the flap. Scraping was performed on the surface of the posterior remaining stroma and on the posterior surface of the corneal flap with a no. 15 Bard-Parker knife. The interface was irrigated with balanced salt solutions and Vigamox®(Alcon, Ft. Worth, TX, USA) eye drops. The flap was repositioned, and the edge was closed with several interrupted and double continuous 10 - 0 nylon sutures to prevent epithelial ingrowth. Topical fluorometholone 0.1% and Vigamox 4 times a day were prescribed.
On post-operative day 1, UCVA was 20/200, and there was a moderate degree of edema on the flap. At the 1 week follow-up, UCVA was 20/100 OD, and there was a mild haze in the interface without recurrence of epithelial ingrowth (Fig. 2). Topical fluorometholone was switched to prednisolone 1%.
One month after the surgery, sutures were removed and prednisolone eye drops were tapered by one drop every month. Two months after the surgery, the patient's refraction was + 1.0 - 0.25 × 180 in the right eye with a corrected visual acuity of 20/20 (Fig. 3). The patient was followed up for six months, maintaining a corrected visual acuity of 20/20 without recurrence of epithelial ingrowth.
A case of delayed epithelial ingrowth associated with viral conjunctivitis in a patient who had LASIK surgery 3 months ago has been described. As the patient showed no complications before he got viral conjunctivitis, we suspect that the viral infection would be the triggering factor in the epithelial ingrowth beneath the flap. Because viral conjunctivitis is highly prevalent in young adults, who are also the majority of the candidates for LASIK surgery, more patients could suffer from this significant complication.
Clinically significant epithelial ingrowth is an infrequent complication after LASIK. When it occurs, about 90% of the epithelial ingrowths are detected within 2 months post-operatively.5 The origin of the epithelium was known to be from the limbus rather than from the epithelial islet left during the procedure. The epithelium from the limbus invades the interface against the adhesive force between the flap and the stroma. As a result, a weakened adhesion occurs due to loose epithelium, epithelial defects, hyperopic LASIK surgeries, or repeated LASIK surgeries.5,6,8 Braunstein et al.9 showed one case of epithelial ingrowth after phacoemulsification, which brought us the idea that phacoemulsification producing stromal edema would result in weakening of the adhesive force between the flap and the posterior stroma. During the conjunctivitis episode, the patient had filamentary keratitis, and a therapeutic bandage contact lens was applied to the right eye for 2 weeks. The filamentary keratitis in viral conjunctivitis associated with punctuate keratitis results in flap edema and a weakening of the adhesive force. Contact lenses on the diseased cornea may also induce flap edema, resulting in the weakening of the adhesive force of the flap to the stroma, even though some surgeons have advocated using a bandage contact lens for the prevention of epithelial ingrowth after primary LASIK, re-treatment, and debridement of epithelial ingrowth in the sound cornea.4,6,10,11 Other possible mechanisms are the mechanical removal of the filament may cause an iatrogenic abrasion or the contact lens adhering to the diseased epithelium may cause the initial erosion. The corneal erosion causes the flap to swell and loosens its adherence to the stoma. We believe epithelial ingrowth, which occurred in this patient, was caused by the edematous flap and the weakened interfacial force, which is mostly induced by the filamentary and the bandage contact lens use with/without corneal erosion.
The causative agent of the conjunctivitis in this case is not confirmed because no organism was positively cultured. We, however, believe the causative agent to be a virus, probably an adenovirus, because of the clinical findings of a conjunctival follicular reaction lasting for three weeks and including characteristic subepithelial infiltrates in the opposite cornea. Moreover, the disease was transmitted from his son.
In conclusion, it should be noted that viral keratoconjunctivitis causing edema of the corneal flap may induce epithelial ingrowth under the flap. Patients who have viral conjunctivitis after LASIK surgery should be examined carefully and managed with consideration of flap complications.
Figures and Tables
Fig. 1
On initial examination in our clinic, there were irregular opacities underneath the flap. (A) The flap is edematous and seems to be detached from the remaining stromal bed. (B) On fluorescein staining, an epithelial defect involving the temporal one-third of the anterior flap surface was noted.

References
1. Rumelt S, Cohen I, Skandarani P, Delarea Y, Ben Shaul Y, Rehany U. Ultrastructure of the lamellar corneal wound after laser in situ keratomileusis in human eye. J Cataract Refract Surg. 2001. 27:1323–1327.

2. Ambrósio R Jr, Wilson SE. Complications of laser in situ keratomileusis: etiology, prevention, and treatment. J Refract Surg. 2001. 17:350–379.

3. Melki SA, Azar DT. LASIK complications: etiology, management, and prevention. Surv Ophthalmol. 2001. 46:95–116.
4. Walker MB, Wilson SE. Incidence and prevention of epithelial growth within the interface after laser in situ keratomileusis. Cornea. 2000. 19:170–173.

5. Wang MY, Maloney RK. Epithelial ingrowth after laser in situ keratomileusis. Am J Ophthalmol. 2000. 129:746–751.
6. Jabbur NS, Chicani CF, Kuo IC, O'Brien TP. Risk factors in interface epithelialization after laser in situ keratomileusis. J Refract Surg. 2004. 20:343–348.

7. Alvarenga L, Marinho S, Mark M. Krachmer JH, Mannis MJ, Holland EJ, editors. Viral conjunctivitis. Cornea. 2005. vol 1:2nd ed. Philadelphia: Elsevier Mosby;629–638.

8. Dastgheib KA, Clinch TE, Manche EE, Hersh P, Ramsey J. Sloughing of corneal epithelium and wound healing complications associated with laser in situ keratomileusis in patients with epithelial basement membrane dystrophy. Am J Ophthalmol. 2000. 130:297–303.

9. Braunstein RE, Airiani S, Chang S. Epithelial ingrowth under a laser in situ keratomileusis flap after phacoemulsification. J Cataract Refract Surg. 2003. 29:2239–2241.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download