Abstract
Purpose
The aim of this study was to evaluate the changes of the regulatory T cell subset in peripheral blood caused by gestational age and premature rupture of membranes (PROM) with or without labor to verify the role of regulatory T cells in pregnancy.
Patients and Methods
We investigated regulatory T cell distribution in the peripheral blood of pregnancies during the first trimester (group I, n = 2), the second trimester (group II, n = 12), and the third trimester without PROM and labor (group III, n = 15). In addition, we evaluated pregnancies in the third trimester complicated by PROM (group IV, n = 4) and labor with no complication by PROM (Group V, n = 5). Comparisons were made with non-pregnant controls (group VI, n = 4) using flow cytometry.
Results
During uncomplicated pregnancy, the CD4+CD25bright regulatory T cell population decreased with advancing gestational age (group I = 3.35 ± 0.47, group II = 2.91 ± 1.44, group III = 2.81 ± 1.36, group VI = 2.52 ± 0.71, p = NS). When we compared group IV with group III and V to evaluate the changes of the regulatory T cells with PROM, the CD4+CD25bright regulatory T cell population was significantly decreased in group IV compared to group III (p = 0.001) and group V (p = 0.026).
Traditionally, the fetus has been viewed as a semi-allograft. However, pregnant women do not experience fatal rejection. This has been explained by the concept that pregnancy is an immunosuppressive state even though pregnant women are not susceptible to overwhelming infection. It, however, remains unknown how the maternal immune system copes with the fetus without activating rejection. Recently, regulatory T cells have been suggested to be important players in the immune tolerance of the fetus during pregnancy.1,2 These regulatory T cells are present at the fetal-maternal interface and have been reported to be important for the maternal acceptance of the allogenic fetus.1 The population of decidual CD4+CD25bright regulatory T cells was found to be decreased with spontaneous abortions compared to normal pregnancies, suggesting that decidual CD4+CD25bright regulatory T cells contribute to the mechanisms that mediate maternal immune tolerance during pregnancy.3 Regulatory T cells have also been found in the peripheral blood lymphocytes of pregnant women.4,5
Like many other obstetrical problems, the etiology of PROM is multifactorial. However, a subclinical intrauterine infection has been implicated as a major factor contributing to the pathogenesis of PROM.6 Most subclinical infections are believed to have ascended from the lower genital tract. The pathogens are thought to ascend into the decidua and enter the fetal membranes, where they generate a cascade of maternal and fetal inflammatory responses that culminate in membrane weakening and rupture.7 Patients with preterm PROM have phenotypic changes in granulocytes and monocytes that are consistent with the presence of intravascular maternal inflammation.8 The physiological processes that regulate the onset of labor have not yet been specifically defined, nevertheless, it has been suggested that the maternal inflammatory response is important to the onset of labor. Therefore, we hypothesized that if the regulatory T cells in maternal blood were decreased, the maternal inflammatory cascade might be activated, leading to PROM and labor.
The aim of this study was to investigate the changes in the CD4+CD25bright regulatory T cell subset of the peripheral blood associated with gestational age, PROM, and labor to determine the role of regulatory T cells in pregnancy.
We collected blood from women visiting Korea University Medical Center from September 2005 to August 2006. Inclusion criteria were healthy non-pregnant women of reproductive age and women in the first, second, and third trimesters of a normal singleton pregnancy. Patients with medical problems such as hypertensive disorder, diabetes mellitus, or autoimmune diseases were excluded. Blood samples were obtained from women in the first trimester during routine prenatal laboratory testing at 7 - 9 weeks gestation and from women in the routine second trimester screening for gestational diabetes at 25 - 27 weeks gestation. Third trimester samples were obtained from women without labor or PROM who were admitted for elective cesarean section as well as from women with labor or PROM at 37 - 40 weeks gestation. Non-pregnant controls were healthy volunteers of reproductive age. The institutional review board approved this study and informed consent was obtained from all patients.
The diagnosis of PROM was confirmed by the clinical findings of a posterior vaginal pool and the vaginal PH or ferning. Labor was defined as painful regular uterine contractions with cervical effacement. There were 32 patients enrolled in the present stud, and they were divided into the following 6 groups: (1) group I, 2 women in the first trimester of pregnancy; (2) group II, 12 women in the second trimester of pregnancy; (3) group III, 15 women in the third trimester of pregnancy without labor or PROM; (4) group IV, 4 women in the third trimester complicated with PROM; (5) group V, 5 women in the third trimester with labor; and (6) group VI, 4 women who were non-pregnant controls.
Fresh blood samples were collected in ethylenediaminetetraacetic acid (EDTA) tubes and analyzed within 24 h. Regulatory T cells were assayed by flow cytometry using CD4-FITC, CD25-PC5.5, CD152-PE (Beckman Coulter, CA, USA) or Foxp3-FITC (eBioscience, CA, USA) monoclonal antibodies. Then, 100 µL of blood were incubated with 10 µL of antibodies for 15 min at room temperature in the dark. After incubation, the cells were lysed by Optylase (RBC lysis buffer, Beckman Coulter), washed, and measured. Data acquisition was performed using Cytomics FC500 (Beckman Coulter).
All data are expressed as median and interquartile ranges. Statistical analysis was performed using the Mann-Whitney U test. A p < 0.05 was considered statistically significant.
In all lymphocyte isolates derived from blood, CD4+CD25bright regulatory T cells could be identified (Fig. 1). We analyzed the levels of CD4+CD25bright regulatory T cells in each of the study groups. Table 1 shows the results. First, we compared the percentage of CD4+CD25bright regulatory T cells in women with uncomplicated pregnancies (groups I, II, and III) to the non-pregnant controls (group IV). During the first trimester, the regulatory T cell population was the highest followed by the second trimester, third trimester, and the non-pregnant controls, but the differences were not statistically significant (Fig. 2). Second, to investigate the changes of the CD4+CD25bright regulatory T cells during the third trimester in pregnancies with PROM, we compared group IV to group III and V, and found that the regulatory T cells were significantly decreased in group IV compared to group III (p < 0.001) and group V (p = 0.026). Fig. 3 shows that the percentage of CD4+CD25bright regulatory T cells decreased in pregnancies with PROM. Finally, there was no significant difference identified (Fig. 4) in the distribution of the regulatory T cells between the third trimester in pregnancies with or without labor (groups III and V).
In this study, we demonstrated the differences in CD4+CD25bright regulatory T cells in the peripheral blood of pregnant women according to gestational age, with or without PROM, and labor for the first time. Pregnancies with PROM during the third trimester showed a statistically lower population of CD4+CD25bright regulatory T cells in the blood than that of pregnancies without PROM. Inflammation has been implicated as a factor responsible for PROM. Many studies have focused on the detection of evidence of inflammation in both the maternal and fetal interface. 9,10 Regulatory T cells play a role in the generation of immunological tolerance to antigens and CD4+CD25bright regularoty T cells, among these regulatory T cells, have shown to have potent regulatory properties.11-13 Our results suggest that the regulatory T cells are involved in the maintenance of the decidua barrier at the fetal-maternal interface during late pregnancy. Due to the relative decrease in the percentage of CD4+CD25bright regulatory T cells in the peripheral blood, a woman could be susceptible to systemic inflammatory responses, possibly leading to a breakdown of the barrier. Consistent with our findings, a normal-term pregnancy has an increased percentage of CD4+CD25bright regularoty T cells in the decidua parietalis compared to the decidua basalis.5 However, the etiology of PROM is multifactorial. The present case-control study had a relatively small sample size and did not include pregnancies with preterm premature rupture of membranes. Therefore, the results should be interpreted with caution.
There are 2 arms of the immune system, the innate and the adaptive system, both of which have cellular and humoral components.14 During pregnancy, the maternal innate immune system is stimulated,15,16 and the adaptive response is either avoided or suppressed.17 This modulation might play an important role during implantation and in overall maternal defenses. Sasaki et al. demonstrated that CD4+CD25bright regulatory T cells are diminished in the blood and decidua in cases with spontaneous abortion compared to normal early pregnancy.3 Our study demonstrated that the percentage of CD4+CD25bright regulatory T cells increased in the blood samples from pregnant women compared to non-pregnant controls, and were the highest in the first trimester followed by the second and third trimesters although these differences were not statistically significant. In addition, CD4+CD25+ regulatory T cells have been reported to decrease in the maternal peripheral blood during the third trimester of pregnancy compared to the first and second trimester, however, with no differences detected between CD4+CD25dim and CD4+CD25bright regulatory T cells.4,18 In this study, we calculated the percentages of CD4+CD25bright regularoty T cells within the total number of lymphocytes. In contrast to our present results, a recent study showed that there was no significant change in the percentage of CD4+CD25bright regulatory T cells within the CD3+CD4+ cell fraction in the peripheral blood during early pregnancy (17 - 23 weeks gestation) compared to term pregnancy (37 - 42 weeks gestation).5 The differences in CD4+CD25+ T-cell subsets might be explained by different gestational ages at sampling time.
The process of decidual activation for the initiation of parturition stimulates an inflammatory reaction, which is an inevitable consequence of labor. During this inflammatory reaction, a number of cytokines, such as tumor necrosis factor-α (TNF-α) and interleukin-1, 6, 8 and 12, are produced and these molecules activate granulocytes such as neutrophils and eosinophils.19 Initially, we hypothesized that the regulatory T cells might be diminished in women during labor, but, our results did not support this. Our study showed that the percentage of CD4+CD25bright regulatory T cells during the third trimester did not differ between women in labor and women not in labor. These findings might be due to activation of the innate immune system, which is an integral part of the immune response during labor, rather than the adaptive immune system regardless of regulatory T cells.
In conclusion, the increase in regulatory T cells during early pregnancy might be related to maternal tolerance during implantation period of the fetus. We identified for the first time the possibility that a decreased number of regulatory T cells might be one of the causes of PROM during the third trimester. Further study is needed to determine the relationship between PROM and regulatory T cells in a larger population of women under different conditions.
Figures and Tables
Fig. 1
Representative FACS (fluorescence-activated cell sorting) stainings for CD4+CD25bright regulatory T cells during the third trimester of normal pregnancy. (A) Plots for CD25 versus CD4 expression demonstrating CD4+CD25bright regualtory T cells. (B) Plots for Foxp3 vs CD25 expression of gated CD4+ T cells.

Fig. 2
Distribution of CD4+CD25bright regulatory T cells in peripheral blood by gestational age (p > 0.05).
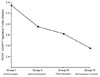
Fig. 3
Distribution of CD4+CD25bright regulatory T cells in the third trimester with or without PROM. Regulatory T cells were significantly decreased in group IV compared to group III (A) and group V (B). The edges of the box plots represent the first and third quartiles, and the horizontal solid line represents the median.

Fig. 4
Distribution of CD4+CD25bright regulatory T cells in the third trimester with or without labor (p > 0.05). The edges of the box plots represent the first and third quartiles, and the horizontal solid line represents the median.

Table 1
The Percentage of CD4+CD25bright Regulatory T Cells in Each Group

Group I, the first trimester of pregnancy; Group II, the second trimester of pregnancy; Group III, the third trimester of pregnancy without labor or PROM; Group IV, the third trimester complicated with PROM; Group V, the third trimester with labor; Group VI, non-pregnant controls.
Data are median and interquartile ranges.
References
1. Aluvihare VR, Kallikourdis M, Betz AG. Regulatory T cells mediate maternal tolerance to the fetus. Nat Immunol. 2004. 5:266–271.

2. Zenclussen AC, Gerlof K, Zenclussen ML, Sollwedel A, Bertoja AZ, Ritter T, et al. Abnormal T-cell reactivity against paternal antigens in spontaneous abortion: adoptive transfer of pregnancy-induced CD4+CD25+ T regulatory cells prevents fetal rejection in a murine abortion model. Am J Pathol. 2005. 166:811–822.

3. Sasaki Y, Sakai M, Miyazaki S, Higuma S, Shiozaki A, Saito S. Decidual and peripheral blood CD4+CD25+ regulatory T cells in early pregnancy subjects and spontaneous abortion cases. Mol Hum Reprod. 2004. 10:347–353.

4. Heikkinen J, Möttönen M, Alanen A, Lassila O. Phenotypic characterization of regulatory T cells in the human decidua. Clin Exp Immunol. 2004. 136:373–378.

5. Tilburgs T, Roelen DL, van der Mast BJ, van Schip JJ, Kleijburg C, de Groot-Swings GM, et al. Differential distribution of CD4(+)CD25(bright) and CD8(+)CD28(-) T-cells in decidua and maternal blood during human pregnancy. Placenta. 2006. 27:Suppl A. S47–S53.

6. Romero R, Chaiworapongsa T, Espinoza J, Gomez R, Yoon BH, Edwin S, et al. Fetal plasma MMP-9 concentrations are elevated in preterm premature rupture of the membranes. Am J Obstet Gynecol. 2002. 187:1125–1130.

7. Simhan HN, Caritis SN, Krohn MA, Hillier SL. The vaginal inflammatory milieu and the risk of early premature preterm rupture of membranes. Am J Obstet Gynecol. 2005. 192:213–218.

8. Gervasi MT, Chaiworapongsa T, Naccasha N, Pacora P, Berman S, Maymon E, et al. Maternal intravascular inflammation in preterm premature rupture of membranes. J Matern Fetal Neonatal Med. 2002. 11:171–175.
9. Parry S, Strauss JF 3rd. Premature rupture of the fetal membranes. N Engl J Med. 1998. 338:663–670.

10. Gomez R, Ghezzi F, Romero R, Muñoz H, Tolosa JE, Rojas I. Premature labor and intra-amniotic infection. Clinical aspects and role of the cytokines in diagnosis and pathophysiology. Clin Perinatol. 1995. 22:281–342.

11. Graca L, Thompson S, Lin CY, Adams E, Cobbold SP, Waldmann H. Both CD4(+)CD25(+) and CD4(+)CD25(-) regulatory cells mediate dominant transplantation tolerance. J Immunol. 2002. 168:5558–5565.

12. Sakaguchi S, Sakaguchi N, Asano M, Itoh M, Toda M. Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J Immunol. 1995. 155:1151–1164.
13. Baecher-Allan C, Brown JA, Freeman GJ, Hafler DA. CD4+CD25high regulatory cells in human peripheral blood. J Immunol. 2001. 167:1245–1253.

14. Sacks G, Sargent I, Redman C. An innate view of human pregnancy. Immunol Today. 1999. 20:114–118.

15. Koumandakis E, Koumandaki I, Kaklamani E, Sparos L, Aravantinos D, Trichopoulos D. Enhanced phagocytosis of mononuclear phagocytes in pregnancy. Br J Obstet Gynaecol. 1986. 93:1150–1154.

16. Shibuya T, Izuchi K, Kuroiwa A, Okabe N, Shirakawa K. Study on nonspecific immunity in pregnant women: increased chemiluminescence response of peripheral blood phagocytes. Am J Reprod Immunol Microbiol. 1987. 15:19–23.

17. Sargent IL. Maternal and fetal immune responses during pregnancy. Exp Clin Immunogenet. 1993. 10:85–102.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download