Abstract
Carotid artery stenting is widely performed for extracranial carotid artery stenosis. In-stent thrombosis is a rare but potentially devastating complication. We present a case of acute in-stent thrombosis immediately following stent insertion and post-balloon dilatation in a 64-year-old male. Thrombosis was successfully treated by intravenous tirofiban, a glycoprotein IIb/IIIa receptor inhibitor.
Carotid artery stenting is increasingly performed for moderate to severe extracranial carotid stenosis and is reported to have similar stroke prevention and risk compared to endarterectomy.1,2 Carotid stent thrombosis is rare compared to coronary artery stent thrombosis,3,4 however it can still result in devastating complications.5 Although glycoprotein IIb/IIIa receptor inhibitors (GPI) have been effectively used in percutaneous coronary intervention, with and without intracoronary stenting, adjunctive GPI use in carotid stenting is unusual. There are several case reports on abciximab, but none on tribofiban.6-8 We present a case of acute in-stent thrombosis successfully treated by intravenous tirofiban.
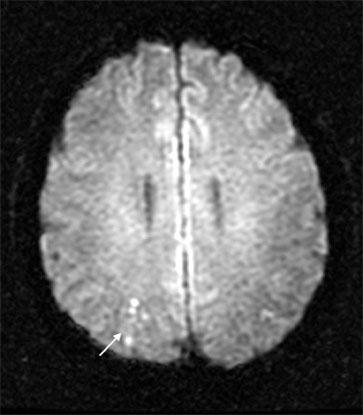
A 63-year-old male was admitted for management of known carotid artery stenosis. Medical history was significant for nasopharyngeal lymphoma status post chemo and radiation therapy 14 years ago, and two episodes of left middle cerebral artery territory infarction, one and seven years ago. Since the last event, he has been on antiplatelet agents (aspirin 100 mg/d). Left common carotid artery stenosis was diagnosed by MR angiography two years ago. Other medications include an oral hypoglycemic and anti-hypertensive agent for diabetes mellitus and hypertension. Neurologic examination showed no deficits. Aspirin (100 mg/d) and clopidogrel (75 mg/d) were administered for two weeks prior to the procedure as usual preventive medication. A digital subtraction angiography showed severe (85%) long segmental stenosis of the left common carotid and mild stenosis of the right vertebral artery orifice (Fig. 1A). A 4,000 unit heparin bolus was given pre-dilatation and 5000 units mixed to 1000 mL of normal saline was used for intra-procedure continuous infusion. After Savvy balloon (4 × 40mm, Cordis, Roden, Netherlands) pre-dilatation of the stenotic left common carotid, a SMART self-expandable carotid stent (7 × 80mm, Cordis, Miami, USA) was deployed. Due to residual stenosis, Savvy balloon (5 × 40mm, Cordis, Roden, Netherlands) post-dilatation was performed for approximately 20 seconds. Immediately post-dilatation, a small filling defect at the distal stent aspect was noted (Fig. 1B). As the defect acutely developed, we suspected acute platelet rich thrombus. Parenteral antiplatelet agent, tirofiban, was infused intravenously with 0.4 µg/kg/min loading dose for 30 minutes, followed by 0.1 µg/kg/min continuous infusion. In-stent thrombus was completely dissolved after 30 minutes of infusion (Fig. 1C). There was no occlusion of the distal intracranial vessels. He received continuous infusion for the next 26 hours. Brain MRI after tirofiban showed small asymptomatic acute infarction on the right occipital lobe in diffusion-weighted images (Fig. 2). There were no hemorrhagic complications. He was discharged without complication on the fourth post-procedure day.
Thrombosis can cause serious post-procedural complications of stent occlusion or distal embolization, resulting in acute cerebral infarction. Acute stent thrombosis rate is reported to be approximately 0.5%.3,9 In the CAVATAS (Carotid and Vertebral Artery Transluminal Angioplasty Study) trial, stroke occurred in 5% of patients immediately or soon after balloon dilatation and stenting. Although the incidence of stroke attributable to acute stent thrombosis is unclear, a substantial proportion is assumed to be a direct result of stent thrombosis or an indirect result by distal embolization.2 Several factors, including mechanical plaque disruption, intimal injury, and stent thrombogenicity predispose the patient to thromboembolic events.10,11 Platelet adhesion, activation, and aggregation play main roles in mural thrombus formation. Considering the mechanism of acute thrombosis, antiplatelet agents may be the best candidates for rescue treatment. GPIs prevent thrombus formation and subsequent distal embolization by inhibiting the final common pathway of platelet aggregation. GPIs have the advantage of parenteral use, and rapid and strong action compared to oral antiplatelet agents. There are three GPIs (abciximab, tirofiban, eptifibatide) available for clinical use; significant differences exist in biological and plasma half-life between abciximab and the small molecule agents (tirofiban and eptifibatide). Various trials of GPIs in percutaneous coronary intervention showed favorable results. However, several trials evaluating routine adjuvant GPI use in carotid artery stent have demonstrated conflicting results. Kapadia et al. showed decreasing procedural complications while other studies showed increased hemorrhagic complications.10-13 Most clinical studies used abciximab, and little data exists on tirofiban; abciximab was used alone or combined with thrombolytics or mechanical thrombectomy in acute stent thrombosis.6-8 Two cases used doses (0.25 mg/kg intravenous bolus and 0.125 µg/kg/min for 12 hours intravenous infusion) typically administered in coronary artery disease and one case used a half dose (0.125 mg/kg) intra-arterially followed by a full dose 12 hour infusion. All cases reported patent ICA after treatment. Tirofiban is a non-peptide tyrosin derivative that mimics the RGD integrin recognition sequence; it has a very short platelet-bound half-life and relatively long plasma half-life. Therefore, it has an advantage when rapid antiplatelet action reversal is required, such as patients with a high risk of hemorrhage or in combined use with thrombolytics. When considering thrombolytics or emergency surgical treatment in cases of GPI failure, tirofiban may be more suitable than abciximab. Furthermore, tirofiban is reported to produce a dose-dependent dethrombotic effect on stent thrombosis and inhibit acute de novo thrombosis under high-shear flow conditions.14
Surgical management is another possible option for acute stent thrombosis. However, as acute thrombosis is rare, it is difficult to accumulate evidence for a preferred treatment strategy. Setacci et al. reported positive results of embolectomy, with or without stent removal, in cases of acute stent thrombosis following stenting while surgical treatment was commonly used in cases of thrombosis after endarterctomy.9,15,16 We chose medical management rather than surgery, because the event occurred in the angiography suite allowing immediate drug infusion. In this case, surgical intervention would have resulted in substantial delay and increased time for ischemia. Furthermore, we had the experience of GPI success in acute thrombosis.17
This case demonstrates that intravenous tirofiban can successfully resolve acute in-stent thrombosis during carotid stent insertion. Until the benefit of routine GPI adjuvant use is proven by a large randomized clinical trial, GPIs should not be recommended for routine use. However, for intra-procedure thrombus, it can be an effective rescue treatment.6,17
Figures and Tables
References
1. Shawl FA. Carotid artery stenting: acute and long-term results. Curr Opin Cardiol. 2002. 17:671–676.

2. CAVATAS investigators. Endovascular versus surgical treatment in patients with carotid stenosis in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): a randomised trial. Lancet. 2001. 357:1729–1737.
3. Tsumoto T, Terada T, Tsuura M, Matsumoto H, Masuo O, Yamaga H, et al. Carotid artery stenting for stenosis with intraluminal thrombus. Neuroradiology. 2006. 48:54–59.

4. Green DW, Sanchez LA, Parodi JC, Geraghty PJ, Ferreira LM, Sicard GA. Acute thromboembolic events during carotid artery angioplasty and stenting: etiology and a technique of neurorescue. J Endovasc Ther. 2005. 12:360–365.

5. Chaturvedi S, Sohrab S, Tselis A. Carotid stent thrombosis: report of 2 fatal cases. Stroke. 2001. 32:2700–2702.
6. Tong FC, Cloft HJ, Joseph GJ, Samuels OB, Dion JE. Abciximab rescue in acute carotid stent thrombosis. AJNR Am J Neuroradiol. 2000. 21:1750–1752.
7. Steiner-Böker S, Cejna M, Nasel C, Minar E, Kopp CW. Successful revascularization of acute carotid stent thrombosis by facilitated thrombolysis. AJNR Am J Neuroradiol. 2004. 25:1411–1413.
8. Bush RL, Bhama JK, Lin PH, Lumsden AB. Transient ischemic attack due to early carotid stent thrombosis: successful rescue with rheolytic thrombectomy and systemic abciximab. J Endovasc Ther. 2003. 10:870–874.

9. Setacci C, de Donato G, Setacci F, Chisci E, Cappelli A, Pieraccini M, et al. Surgical management of acute carotid thrombosis after carotid stenting: a report of three cases. J Vasc Surg. 2005. 42:993–996.

10. Chaturvedi S, Yadav JS. The role of antiplatelet therapy in carotid stenting for ischemic stroke prevention. Stroke. 2006. 37:1572–1577.

11. Wholey MH, Wholey MH, Eles G, Toursakissian B, Bailey S, Jarmolowski C, et al. Evaluation of glycoprotein IIb/IIIa inhibitors in carotid angioplasty and stenting. J Endovasc Ther. 2003. 10:33–41.

12. Qureshi AI, Suri MF, Ali Z, Kim SH, Lanzino G, Fessler RD, et al. Carotid angioplasty and stent placement: a prospective analysis of perioperative complications and impact of intravenously administered abciximab. Neurosurgery. 2002. 50:466–475.

13. Kapadia SR, Bajzer CT, Ziada KM, Bhatt DL, Wazni OM, Silver MJ, et al. Initial experience of platelet glycoprotein IIb/IIIa inhibition with abciximab during carotid stenting: a safe and effective adjunctive therapy. Stroke. 2001. 32:2328–2332.

14. Rukshin V, Azarbal B, Finkelstein A, Shah PK, Cercek B, Tsang V, et al. Effects of GP IIb/IIIa receptor inhibitor tirofiban (aggrastat) in ex vivo canine arteriovenous shunt model of stent thrombosis. J Cardiovasc Pharmacol. 2003. 41:615–624.

15. Findlay JM, Marchak BE. Reoperation for acute hemispheric stroke after carotid endarterectomy: is there any value? Neurosurgery. 2002. 50:486–493.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download