Abstract
Purpose
The clinical features, treatment modality approaches in clinical practice, and prognostic factors for anal canal carcinoma patients were retrospectively analyzed.
Materials and Methods
Between October 1994 and December 2005, 50 patients with anal canal cancer were treated at Samsung Medical Center, Seoul, Korea.
Results
After a median follow up of 37.8 months (range, 6.6 - 136.1 months), the 5-year and 10-year survival rates for the 38 patients with early and locally advanced squamous and cloacogenic carcinoma (squamous cell carcinoma and cloacogenic carcinoma) were 74.8% and 66.5%, respectively. The 5-year survival and disease-free survival rates (DFS) of the 31 patients who received chemoradiation therapy (CRT) were 83.6% and 74.3%, respectively. The overall and DFS could not be determined for the adenocarcinoma group due to the small number of cases (n = 8). Univariate analysis showed that tumor size (p = 0.04) and inguinal node status (p = 0.04) significantly influenced patient survival in patients with squamous cell and cloacogenic carcinomas. Furthermore, univariate analysis also showed that, inguinal node status influenced patient survival in the adenocarcinoma group. Multivariate analysis showed that inguinal node metastasis is a single independent prognostic variable for survival (p = 0.04) in patients with squamous cell and cloacogenic carcinomas.
Conclusion
Combined CRT has been adopted as standard treatment with outcomes that are comparable to those reported in randomized clinical trials. Due to the rarity and complexity of anal canal carcinoma, interdepartmental cooperation is required for disease treatment. Thus, proper treatment of patients should incorporate a team-approach and should be available to as many patients as possible.
Anal canal cancer is rare and only accounts for 1% to 6% of all anorectal malignancies.1 The pathogenesis and treatment of anal canal cancer has undergone substantial reassessments over the past few decades. The current goals of anal cancer treatment are controlling the disease locally, salvaging the sphincter, and avoiding the need for a permanent colostomy. Nigro et al.2 reported the first successful use of concurrent chemoradiation (CCRT) in an attempt to downstage a locally advanced tumor in a patient before an abdominoperineal resection (APR). Since then, chemoradiation therapy has become the standard treatment for anal cancer, even for early disease. Surgery is only recommended for those patients who do not achieve a complete clinical response to primary chemoradiation.3,4 Results from three subsequent randomized trials5-7 demonstrated that concurrent chemoradiotherapy with mitomycin and 5-FU had superior results compared to radiotherapy alone in controlling the local disease and improving survival rates. The trial conducted by the European Organization for Research and Treatment of Cancer (EORTC)6 also showed the superiority of concomitant 5-FU/mitomycin and radiotherapy treatments compared to using radiotherapy alone.
In this study, we retrospectively analyzed the clinical features, treatment modality approaches in clinical practice, and prognostic factors in anal canal carcinoma patients.
Between October 1994 and December 2005, 50 patients with anal canal cancer were treated at Samsung Medical Center, Seoul, Korea. The following data were thoroughly reviewed and collected from the medical records for analyses: demographics, histological type, clinical stage, vital status, recurrence, treatment modality, and treatment outcome. The main outcome measures were treatment response rate and overall survival. Patients were clinically staged according to the American Joint Committee on Cancer (AJCC) TNM staging system.8 Tumor assessments consisted of digital rectal examination, colonoscopy, and abdominopelvic CT scan. Rectal MRI and endorectal ultrasonography were performed as indicated.
Tumor response was assessed 6 weeks after the completion of the CCRT. The criteria for determining response were as follows: 1) complete response (CR) was defined as the clinical disappearance of the tumor, 2) partial response (PR) was defined as a 50% or greater reduction in the largest tumor diameter, and 3) failure of the CCRT regimen or progressive disease was defined as an 25% or greater increase in the largest tumor diameter or the appearance of new lesions.
Only the records of patients whose tumor involved the anal canal (defined as 0 - 4 cm from the anal verge) were considered. If > 50% of the tumor length was proximal to this region, patients were considered to have adenocarcinoma of the rectum and therefore were excluded. In an attempt to eliminate the rectal cancers from the group, hematoxylin-eosin stained slides were reviewed to distinguish between tumors of the rectal mucosa and anal duct origin.
The patient characteristics are outlined in Table 1. Bleeding, with or without perianal pain, was the most common presenting symptom (40.0%) followed by anal pain (18.0%).
The primary treatment modality for 39 patients (78.0%) was CCRT. Thirty patients received a continuous infusion of 5-FU (1000 mg/m2 daily on days 1 - 4 and 29 - 32 of radiation therapy) and a short infusion of 10 mg/m2 mitomycin C during the first course of 5-FU. The remaining nine patients received either cisplatin or capecitabine based on their performance status. Radiotherapy consisted of a daily dose of 1.8 Gy up to a total dose of 45 Gy (twenty-five fractions in 5 weeks) by external beam irradiation on the anoperineal region, including the perirectal nodes. Up to an additional 63 Gy boost radiation was given, depending on the response and gross residual disease. When inguinal lymphadenopathy was present in the patient, the entire inguinal chain including iliac lymph nodes were irradiated with 45 Gy using a anteroposterior/posteroanterior (AP/PA) technique with a narrower PA field covering the true pelvis.
Overall survival (OS) and relapse-free survival (RFS) were estimated using the Kaplan-Meier product-limit method. OS was measured from the date of diagnosis to the date of death or the last follow-up visit. RFS was calculated from the date of diagnosis to the first documented relapse in patients who attained CR. Statistical differences in survival rates were compared using log-rank analysis. Continuous biological variables were dichotomized. P-values less than 0.05 were considered statistically significant.
The median age at presentation was 67 years (range, 39 - 81 years). The patients had the following disease histologies: 33 squamous cell carcinomas (66.0%), 9 cloacogenic (18.0%), and 8 adenocarcinomas (16.0%). Cloacogenic carcinomas were predominant in females (7/9, 77.7%), while squamous cell carcinomas and adenocarcinomas did not show sexual preponderance (Table 1). At the time of diagnosis, 31 patients (62.0%) had locally advanced disease and 4 patients (8.0%) had distant metastases. Of the 31 patients with locally advanced disease, 18 (36.0%) had metastases to the perirectal (N1), inguinal lymph nodes (N2), and/or the internal iliac lymph nodes as detected by clinical examination and/or imaging studies. There were no treatment related morbidities requiring hospitalization and no deaths were recorded. 4 patients were tested for human papilloma virus and 2 out of these 4 patients (50%) tested positive for the virus.
The primary treatment modalities for the 50 patients are presented in Table 2. Thirty-seven patients (74.0%) received the definitive CCRT as their initial treatment. Twenty-eight patients (75.7%) received concomitant radiotherapy with 5-FU and mitomycin C. Five patients (13.5%) were treated concomitantly with 5-FU and cisplatin during radiotherapy. Four patients (10.8%) received radiotherapy with daily oral administration of capecitabine alone due to poor performance status. Four patients (8%) underwent abdominoperineal resection as their initial treatment. The reasons for primary surgical intervention were due to patients' refusal, for complications such as recto-vaginal fistula, or for unknown reasons.
The 5-year and 10-year survival rates for the 38 patients with early and locally advanced squamous cell carcinoma and cloacogenic carcinoma were 74.8% and 66.5%, respectively. The 5-year survival and DFS of the 31 patients who received CRT were 83.6% and 74.3% respectively. The overall survival and DFS could not be determined in the adenocarcinoma patient group due to the small number of cases (n = 8). No notable difference was found in the overall survival between the squamous cell and cloacogenic carcinoma groups and the adenocarcinoma group at the 5- or 10-year time points (p = 0.485).
After definitive chemoradiotherapy, thirty-one patients (83.7%) achieved complete response. Four of the 31 patients (12.9%) who initially achieved complete response had recurrences. All of these 4 patients recurred at distant sites; three of these patients had liver metastases. Two (33.3%) of the patients with recurrences were treated by palliative APR to relieve symptoms, one patient (16.7%) had palliative chemotherapy, and one patient (16.7%) had palliative radiation therapy, Three patients (8.1%) had partial responses and 3 patients demonstrated primary resistance to chemoradiation therapy. Four patients who received primary APR were in remission at the time of analysis. Univariate analyses indicated that the significant parameters influencing survival were tumor size (p = 0.04) and inguinal node status (p = 0.04) (Table 3). Multivariate analysis showed that inguinal node metastasis is a single independent prognostic variable for survival (p = 0.04).
After a median follow up of 37.8 months (range,6.6 - 136.1 months), the 5-year and 10-year survival rates for the 46 patients with early and locally advanced disease were 71.9% and 64.7%, respectively (Fig. 1). The 5-year survival and disease-free survival rates of the 37 patients who received CRT were 76.9% and 69.0%, respectively. The CRT group had a tendency towards better survival than the APR group, although this difference was not statistically significant (p = 0.44) (Fig. 2).
With a median patient age of 67 years (range: 39 - 81 years) and patient group that is predominantly made up of women, our patient group is similar to the patient groups in previous studies.2,3,5-7,9 HIV positive homosexual males have a 36% increased incidence of anal cancer.10,11 None of the Korean patients were HIV positive, probably due to a very low incidence of HIV positive patients (less than 0.1%) in the country.
The initial outcome for 37 patients with locoregional disease who had been treated with concurrent CRT are consistent to the outcomes previously reported in the literature.5,6,12-15 We observed a CR rate of 83.7%, which is comparable to other published series.5,6,12-14 Interestingly, patients with an initial tumor size of less than 5 cm had a tendency towards higher treatment response (87.1%), although this tendency was not statistically significant (p = 0.17). The 5-year survival rate for the subset of patients with squamous and cloacogenic carcinomas was 74.8% in our series, which is slightly higher than the 5-year survival rates reported in the EORTC and UKCCCR trials (3 year survival of 72% and 65%, respectively).5,6
The primary anal adenocarcinoma histological subtype is a rare tumor accounting for only 16.5% of all anal cancers.15,16 The 6 patients with evaluable disease at the start of therapy had T1 and T2 lesions and achieved complete response. None of the patients developed recurrent or metastatic disease. If an accurate diagnosis can be made, one can speculate that anal adenocarcinoma is analogous to other anal canal tumors and thus chemoradiation therapy can be recommended for anal adenocarcinoma patients. No survival difference was found when patients with squamous cell carcinoma and cloacogenic carcinoma patients were combined and compared to anal adenocarcinoma patients (p = 0.17).
The two significant factors that were found by univariate analysis to influence the survival of squamous cell carcinoma and cloacogenic carcinoma patients were tumor size and inguinal lymph node metastases (p = 0.04 and p = 0.04). These findings are in agreement with other studies that reported tumor size and lymph node status are strong predictors of the initial response to treatment and survival.2,3,5-7,9,17 While the tumor size is an independent prognostic factor, this finding reflects that larger tumors are more likely to involve regional lymph nodes,17 which are known to be associated with local recurrences and salvage surgical resections and thus, reduced survival rates.1,17,18
Although distant metastasis is uncommon at presentation,19 we observed that 8% of the patients had distant metastasis at the time of diagnosis and 18% of the patients had inguinal node metastases. The UKCCCR Anal Cancer Trial Working Party reported5 that 40% of the cancer deaths occurred with disease that had been identified outside the pelvis. Further studies need to focus on improving systemic control of the disease. In particular, cisplatin-based regimens should be further investigated since Hung et al.20 recently reported a promising application of this drug for anal carcinoma. Currently, a randomized Radiation Therapy Oncology Group (RTOG) phase III trial is comparing 5-FU and mitomycin C with 5-FU and cisplatin in a multimodal approach combined with radiotherapy. The value of substituting cisplatin for mitomycin in combination-therapy regimens is currently being investigated.
Acceptance of CRT as the "gold standard" for anal cancer treatment not only achieved excellent short- and long-term results, but also improved the quality of life by reducing aggressive surgical approaches and by decreasing the adverse effects associated with high dose radiotherapy.5,6,17,21 The CRT subsequently led to a higher local control rate and preservation of anal sphincter function in a great majority of the patients. As a result, surgery is no longer the treatment of choice, but has become a salvage therapy for the patients who did not achieve CR. Because of the rarity and complexity of anal canal cancer, interdepartmental cooperation is required for patient treatment, thus a team-approach should be available for proper patient treatment. Anal cancer screening and prevention are gaining more acceptance in the clinic, but require further study.11,17,22
Figures and Tables
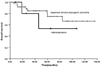 | Fig. 1Overall survival in patients with squamous cell and cloacogenic carcinoma (crosses) versus adenocarcinoma (triangles) for stage I through III (p = 0.485). |
 | Fig. 2Overall survival according to treatment methods (p = 0.44). CRT, chemoradiation; APR, abdominoperinal resection. |
References
1. Whiteford MH, Stevens KR Jr, Oh S, Deveney KE. The evolving treatment of anal cancer: How are we doing? Arch Surg. 2001. 136:886–891.
2. Nigro ND, Vaitkevicius VK, Considine B Jr. Combined therapy for cancer of the anal canal: a preliminary report. 1974. Dis Colon Rectum. 1993. 36:709–711.
3. Nigro ND, Vaitkevicius VK, Considine B Jr. Combined therapy for cancer of the anal canal: a preliminary report. Dis Colon Rectum. 1974. 17:354–356.
4. Cummings B, Keane T, Thomas G, Harwood A, Rider W. Results and toxicity of the treatment of anal canal carcinoma by radiation therapy or radiation therapy and chemotherapy. Cancer. 1984. 54:2062–2068.

5. Epidermoid anal cancer: results from the UKCCCR randomised trial of radiotherapy alone versus radiotherapy, 5-fluorouracil, and mitomycin. UKCCCR Anal Cancer Trial Working Party. UK Co-ordinating Committee on Cancer Research. Lancet. 1996. 348:1049–1054.
6. Bartelink H, Roelofsen F, Eschwege F, Rougier P, Bosset JF, Gonzalez DG, et al. Concomitant radiotherapy and chemotherapy is superior to radiotherapy alone in the treatment of locally advanced anal cancer: results of a phase III randomized trial of the European Organization for Research and Treatment of Cancer Radiotherapy and Gastrointestinal Cooperative Groups. J Clin Oncol. 1997. 15:2040–2049.

7. Flam M, John M, Pajak TF, Petrelli N, Myerson R, Doggett S, et al. Role of mitomycin in combination with fluorouracil and radiotherapy, and of salvage chemoradiation in the definitive nonsurgical treatment of epidermoid carcinoma of the anal canal: results of a phase III randomized intergroup study. J Clin Oncol. 1996. 14:2527–2539.

8. American Joint Committee on Cancer. Ajcc Cancer Staging Manual. 2002. 6th ed. New York: Springer-Verlag;61.
9. Nilsson PJ, Svensson C, Goldman S, Ljungqvist O, Glimelius B. Epidermoid anal cancer: a review of a population-based series of 308 consecutive patients treated according to prospective protocols. Int J Radiat Oncol Biol Phys. 2005. 61:92–102.

10. Goldstone SE, Winkler B, Ufford LJ, Alt E, Palefsky JM. High prevalence of anal squamous intraepithelial lesions and squamous-cell carcinoma in men who have sex with men as seen in a surgical practice. Dis Colon Rectum. 2001. 44:690–698.

11. Palefsky JM, Holly EA, Ralston ML, Arthur SP, Jay N, Berry JM, et al. Anal squamous intraepithelial lesions in HIV-positive and HIV-negative homosexual and bisexual men: prevalence and risk factors. J Acquir Immune Defic Syndr Hum Retrovirol. 1998. 17:320–326.

12. Touboul E, Moureau-Zabotto L, Lerouge D, Pene F, Deniaud-Alexandre E, Tiret E, et al. Radiotherapy of carcinomas of the anal canal. Tenon Hospital experience. Cancer Radiother. 2003. 7:Suppl 1. 91S–99S.
13. Rich TA, Ajani JA, Morrison WH, Ota D, Levin B. Chemoradiation therapy for anal cancer: radiation plus continuous infusion of 5-fluorouracil with or without cisplatin. Radiother Oncol. 1993. 27:209–215.

14. Tanum G, Tveit K, Karlsen KO, Hauer-Jensen M. Chemotherapy and radiation therapy for anal carcinoma. Survival and late morbidity. Cancer. 1991. 67:2462–2466.

15. Myerson RJ, Karnell LH, Menck HR. The National Cancer Data Base report on carcinoma of the anus. Cancer. 1997. 80:805–815.

16. Nielsen OV, Koch F. Carcinomas of the anorectal region of extramucosal origin with special reference to the anal ducts. Acta Chir Scand. 1973. 139:299–305.
17. Esiashvili N, Landry J, Matthews RH. Carcinoma of the anus: strategies in management. Oncologist. 2002. 7:188–199.

18. Wong S, Gibbs P, Chao M, Jones I, McLaughlin S, Tjandra J, et al. Carcinoma of the anal canal: a local experience and review of the literature. ANZ J Surg. 2004. 74:541–546.

19. Pintor MP, Northover JM, Nicholls RJ. Squamous cell carcinoma of the anus at one hospital from 1948 to 1984. Br J Surg. 1989. 76:806–810.

20. Hung A, Crane C, Delclos M, Ballo M, Ajani J, Lin E, et al. Cisplatin-based combined modality therapy for anal carcinoma: a wider therapeutic index. Cancer. 2003. 97:1195–1202.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download