Abstract
Human papillomavirus (HPV) infection is a co-carcinogen of lung cancer and contributes to its pathogenesis. To evaluate the prevalence of HPV infection, polymerase chain reaction (PCR) was employed to detect HPV 16, 18, and 33 DNA in tumor tissues of 112 patients with non-small cell lung cancer (NSCLC) who underwent curative surgery from Jan. 1995 to Dec. 1998 at Severance Hospital, Seoul, Korea. The patients consisted of 90 men and 22 women. Nineteen patients were under 50 years old (17%), and 92 patients (82%) were smokers. Fifty-three patients had adenocarcinomas, while 59 patients had non-adenocarcinomas. Early stage (I and II) cancer was found in 64 patients (57.1%) and advanced stage (III and IV) found in 48 (42.9%). The prevalence of HPV 16, 18, and 33 were 12 (10.7%), 11 (9.8%), and 37 (33.0%), respectively. Smoking status, sex, and histologic type were not statistically different in the presence of HPV DNA. The presence of HPV 16 was more common in younger patients and HPV 18 was more common in advanced stage patients. This study showed that the prevalence rate of HPV 16 and 18 infections in NSCLC tissue was low, suggesting HPV 16 and 18 infections played a limited role in lung carcinogenesis of Koreans. However, the higher prevalence of HPV 33 infections in Korean lung cancer patients compared to other Asian and Western countries may be important and warrants further investigation.
The incidence of lung cancer has been increasing steadily, and it is the leading cause of cancer deaths worldwide and in Korea.1 Its prominence is due in part to tumors being disseminated by the time of lung cancer is diagnosed. Epidemiologic studies suggest that cigarette smoking is the principal, but not only, factor involved in lung carcinogenesis.2 Over the past three decades, the incidence of lung adenocarcinoma has increased worldwide. Most individuals with lung adenocarcinoma (especially women) are non-smokers, and the exploration of carcinogenic etiologies other than cigarette smoking is warranted. HPV has been shown to be implicated in human neoplasm of the uterus, cervix, vulva, skin, esophagus, and head and neck.3 HPV is most commonly associated with the development of cervical carcinomas, and HPV 16 and HPV 18 are the types most frequently detected in high-grade squamous intraepithelial lesions and invasive carcinomas. E6 proteins, encoded by HPV, can bind to the host cellular tumor suppressor protein, p53, and trigger its degradation through the ubiquitin pathway.4,5 The inactivation of p53 by HPV-E6 is considered to play a crucial role in human carcinogenesis.6
Evidence for the involvement of human papillomavirus (HPV) in lung carcinogenesis has accumulated through several distinct lines of research. HPV DNA has been detected in around 50% of benign bronchial squamous cell papillomas. The detection of morphological changes on light microscopy suggests HPV infection in bronchial cancer and its precursor lesions.7 Recently, Taiwanese reports suggested that HPV infection was closely related to adenocarcinomas of the lung, especially in non-smoking women.8,9 Some data from Japan and Northern European countries such as Finland and Norway have shown that significantly higher frequencies of HPV infection (69-78.3%) were observed in conjunction with lung carcinomas.10-13 These data suggest that the association between HPV infection and lung cancer may be geography- and race-dependent.
To evaluate the prevalence of HPV infection in Korean lung cancer patients and the association of HPV with histologic cell types of lung cancer, we screened for HPV DNA using polymerase chain reaction (PCR) with HPV 16, 18, and 33 type-specific primers, which encode for the high cancer risk indicators in lung cancer tissues. Furthermore, we assessed the prognostic relevance of HPV infection and survival of patients with lung cancer.
One hundred and twelve patients with primary non-small cell lung cancer who had undergone thoracic surgery at Severance Hospital, Seoul, Korea from Jan. 1995 to Dec. 1998, were studied. All patients underwent pathologic stage examination by a board-certified pathologist (DH Shin).
None of the patients had received radiation therapy or chemotherapy prior to surgery. Demographic data including age, gender, smoking status, and survival were collected on each individual from patient interviews, their records of the Yonsei Cancer Registry Center, and a review of medical records.
Genomic DNA was prepared from tissue sections by a conventional phenol-chloroform extraction, ethanol precipitation, and finally dissolved in 20 µl of sterile distilled water. HPV viral DNA was amplified with type specific primers (TAKARA Bio Inc., Shiga, Japan) flanking the E6 region to identify the HPV subtype.14 The forward primer (5'-AAGGG CGTAA CCGAA ATCGG T-3') was common to the sequence of HPV 16, 18, and 33 DNA. The reverse primer sequences for HPV 16, 18, and 33 were 5'-GTTTG CAGCT CTGTG CATA-3', 5'-GTGTT CAGTT CCGTG CACA-3', and 5'-GTCTC CAATG CTTGG CACA-3', respectively. The final PCR product of 10 µl was loaded onto a 2% agarose gel, stained with ethidium bromide, and visualized under UV illumination. The final product sizes, including the E6 region, were 140bp in HPV 16 and HPV 18, and 141bp in HPV 33. Appropriate negative and positive controls were included in each PCR reaction for HPV 16, 18, and 33. A part of the medium was amplified to exclude false-negative results, while DNA preparations of a HPV template from the manufacturer were used as positive controls (Fig. 1).
Statistical analysis was performed using the SPSS statistical software program (SPSS Inc., Chicago, IL). Differences between HPV 16, 18, and 33, and between gender, smoking status, histologic cell types, and tumor stage were calculated using the Chi-square test. Logistic regression analysis was used to assess which variable was important for HPV infection and which variable may act as a lung cancer risk factor. Kaplan-Meier survival curves were used to evaluate the correlation between HPV subtype and survival of lung cancer patients.
The patients ranged from 34 to 78 years of age (mean 59 ± 11 years), 90 of 112 were males, and 19 were under 50 years old. Ninety-two patients had a history of cigarette smoking (mean 39 ± 20 pack years), while 20 were non-smokers.
Histologic examination of the tumors revealed 53 cases of adenocarcinoma, including five bronchioloalveolar cell carcinomas and seven peripheral adenocarcinomas with BAC pattern. Fifty-nine non-adenocarcinomas, including 53 squamous cell carcinomas and six large cell carcinomas, were also found. Tumor stages I, II, III, and IV were observed in 40 (35.7%), 24 (21.4%), 44 (39.3%), and four patients (3.6%), respectively.
The detection rates of HPV 16, 18, and 33 DNA in tumor tissue by PCR were 10.7%, 9.8%, and 33.0%, respectively. As shown in Table 1, the prevalence of HPV was similar in male and female patients for all HPV types. Likewise, the prevalence of HPV was not different in adenocarcinoma and non-adenocarcinoma tumors. However, patients under 50 years old had a significantly higher rate of HPV 16 than patients older than 50 (26.3% vs. 7.5%, p = 0.016). For HPV 18, patients with tumor stages I and II had a lower prevalence than those with stages III and IV (4.7% vs. 16.7%, p=0.035). The prevalence of HPV 33 was indistinguishable between patients with well-differentiated tumors and those with moderate or poor tumor differentiation (45.2% vs. 21.3% or 38.2%, respectively, p = 0.063) (Table 1). The co-infection of HPV 16 and/or HPV 18 also did not show significant results (data not shown).
Multivariate logistic regression analysis showed that the presence of HPV 16 had a four-fold higher risk in NSCLC patients under 50 years old, and that HPV 18 had a 3.9-fold higher risk in NSCLC patients with a tumor stage of III or IV after adjusting for other factors (Table 2).
The survival times of NSCLC patients were compared, using the Kaplan-Mayer test method with a log rank test. None of the HPV infections had any statistically significant effect on survival time (Fig. 2).
The prevalence of HPV DNA in lung cancer patients varies significantly by geographical region. In the literature, the prevalence of HPV infection in lung carcinomas varies from 0% to 79%.12,15-17 Hirayasu et al. reported that the prevalence of HPV 16 and 18 infections in Okinawa, a subtropical island of southern Japan, was high (58.1% and 58.1%, respectively), but in Niigata, the mainland of Japan, was lower (6.7% and 23.3%, respectively).12 However, Taiwan, the nearest neighbor to Okinawa, had a high prevalence of HPV 16 and 18 infections (35.5% and 41.1%, respectively) in lung carcinomas.8 Our study of 112 NSCLC patients resulted in the detection rates of HPV DNA 16, 18, and 33 in 12 (10.7%), 11 (9.8%), and 35 (31.3%) patients, respectively. This is the first study of HPV DNA prevalence in lung cancer patients from Korea, where the prevalence rate was lower than that of other Asian countries. The overall prevalence of HPV 16 and 18 infections of the cervix was 12.6% (389/3091) and was calculated at 15.5% when standardized in a Korean study of healthy women.18 This value was similar to the 18.2% (4/22) of women in this study.
The geographic variability is associated with sexual behavior and environmental factors.19 Okinawa was considered a HPV high prevalence region, but recent improvements in hygiene (water supply, toilets, and sewage disposal) after Okinawa reverted to Japan have greatly reduced the incidence of HPV infection.20 This change was followed by a decrease in the incidence of squamous cell carcinoma, especially well-differentiated cases. In Taiwan, non-smoking females with adenocarcinomas had a high prevalence of HPV 16 and 18 infections in lung carcinomas.8,9 In our study, gender, smoking status, tumor differentiation, and histologic cell types were not associated with HPV 16, 18, and 33 infections among patients with lung cancer. These discrepancies might result, in part, from the different detection systems, sample conditions, and geographic sexual activity and behavior. Furthermore, a decreasing trend in the prevalence of HPV in lung squamous cell carcinomas, especially the well-differentiated, is related to a decline in HPV infection.21
In our study, co-infection of HPV 16 and 18 occurred in only one case (0.9%), while co-infection with HPV types 16 and 33, and HPV types 18 and 33 occurred in five cases each (3.6%). In a Taiwanese study, a higher prevalence of co-infection with multiple HPV types had a higher risk of lung cancer compared to patients with only one type of HPV infection.8 However, Japanese patients22 and Korean patients in our study demonstrated a lower prevalence of co-infection, and had a lower risk of lung cancer (Table 3). These findings suggest that HPV infection might be type-specific and have a synergistic effect on lung carcinogenesis through multiple steps and modeling.
HPV 33 infections had previously been considered less important than HPV 16 and 18 in lung cancer. However, our study showed a high prevalence of HPV 33 infections in Korean lung cancer patients. We reviewed the literature and compared the prevalence of HPV 33 infections in several countries (Table 4). Other Asian and Western countries had an HPV prevalence of 0% to less than 10% in all except one study.11,12,16,23-27 This implied that HPV 33 might be specific and play an important role in Korean lung carcinogenesis. However, one limitation of our study was not enrolled normal lung tissues from non-cancer subjects, which may have yielded a lower frequency of HPV 33 infection.
The observation of certain types of HPV in association with cervical and oral squamous cell carcinoma raises the possibility of sexual transmission of HPV from the cervix to the oral cavity, with subsequent transmission to the larynx, and then to the lung.28 It is likely that the transmission of viral infection to non-genital sites occurs as a consequence of certain sexual behaviors, such as oral-genital contact, or by autoinoculation from a genital infection and, therefore, is acquired by standard sexual behavior measures. Sexual characteristics known to be associated with HPV exposure include a high number of lifetime sexual partners, young age at first intercourse, and a history of sexually transmitted disease.29 Another transmission pathway of HPV infection to the lung is blood circulation. A recent study showed that HPV E6 mRNA was detected in the peripheral blood of advanced cervical cancer patients. This observation seems to reflect the possibility that HPV infection in lung tissues may originate in the cervix, and would then be mediated by blood circulation.30 Several head and neck squamous cell carcinoma patients carrying HPV positive sera were found to develop distant metastasis.31
Since younger patients have a higher sexual activity, they also have a higher risk of HPV infection.18 In our study, the presence of HPV 16 had a four-fold higher prevalence in NSCLC patients under 50 years old and HPV 18 had a 3.9-fold higher prevalence in NSCLC patients with a tumor stage of III & IV after adjusting for other factors (Table 2). These results were similar with that of Taiwanese studies.8,9,32 One reason may be that HPV 18 may play a role in the development of rapidly progressive tumors. Kurman et al. suggested that the deficit of HPV 18 in intraepithelial neoplasia, as compared with invasive carcinoma, could represent a rapid transit time through the precursor stage of cervix cancer.33 Walker et al. also suggested that HPV 18-containing tumors might progress to invasion without a prolonged preinvasive stage.34 Alternatively, Barbosa et al. further demonstrated that the rate of phosphorylation of Rb by HPV 16 and 18 E7 varies, with HPV 18 E7 being phosphorylated 2-fold faster than HPV 16 E7 which in turn is 2-fold faster than HPV 6 E7.35 This can explain why these three viruses differ in their relative efficiency in carcinogenesis, while they all possess E7 proteins. The association of HPV 18 with advanced stage lung cancer may be explained by the apparently higher oncogenic potential of this virus. Furthermore, cellular receptors with a specific potential for binding with each of the HPV types may exist.36
Viral copy number is another important factor in the distribution of HPV viral particles and metastasis. Recently, E5 protein of HPV 16 was found to be expressed in the early stages of neoplastic transformation; HPV vaccines, targeting E5, are being developed.37 Further studies are required to monitor the viral copy number in blood and association those levels with various clinical parameters. The presence of HPV 16, 18 and 33 infections was not associated with the survival times of NSCLC patients (Fig. 2). In a literature review, high Langerhans cell infiltration22 and p53 protein accumulation38 with HPV infection was associated with the prognosis of lung cancer. In the present study, Langerhans cell infiltration was not frequently observed in pathologic samples, and p53 protein regulation was not examined.
The sensitivities of the HPV DNA detection systems have varied between reports (Table 3). Standardization of the detection system is needed, including the primers and probes used. The age and handling of samples needs to be standardized. When old samples were used, the detection rate of HPV DNA decreased with sample age. Fresh samples obtained immediately after surgery without fixation, or at most one or two months after surgery, yielded better results.
In conclusion, our study showed that the prevalence of HPV 16 and 18 infections in lung cancer tissue was low, suggesting HPV 16 and 18 infections played a limited role in lung carcinogenesis of Koreans. However, the higher prevalence of HPV 33 infection may be important for Korean lung cancer patients, and warrants further investigation.
Figures and Tables
 | Fig. 1Representative results of polymerase chain reaction (PCR) with HPV-type specific primers for negative and positive HPV DNA detection in tumor tissue. SM, size marker; Lane 1: negative HPV DNA; Lane 2: positive HPV DNA; Lane 3: positivecontrol; Lane 4: negative control. |
 | Fig. 2Kaplan-Meier survival curves of HPV 16, 18, and 33 infections in patients with non-small cell lung cancer. No significant difference in survival times was observed (log rank test, p > 0.05). |
Table 1
Relationships between the Presence of HPV DNA Detected by PCR in Tumor Tissues and Clinical-Pathologic Parameters
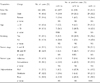
Table 2
Multivariate Logistic Regression Analysis for the Relationship between HPV DNA Detection in Tissues of Lung Cancer Patients and Clinical Parameters

References
1. Korea Central Cancer Registry, Ministry of Health and Welfare Republic of Korea. Annual Report of the Korea Central Cancer Registry. 2002.
2. Wood ME, Kelly K, Mullineaux LG, Bunn PA Jr. The inherited nature of lung cancer: a pilot study. Lung Cancer. 2000. 30:135–144.

4. Werness BA, Levine AJ, Howley PM. Association of human papillomavirus types 16 and 18 E6 proteins with p53. Science. 1990. 248:76–79.

5. Scheffner M, Werness BA, Huibregtse JM, Levine AJ, Howley PM. The E6 oncoprotein encoded by human papillomavirus types 16 and 18 promotes the degradation of p53. Cell. 1990. 63:1129–1136.

6. Storey A, Thomas M, Kalita A, Harwood C, Gardiol D, Mantovani F, et al. Role of a p53 polymorphism in the development of human papillomavirus-associated cancer. Nature. 1998. 393:229–234.

8. Cheng YW, Chiou HL, Sheu GT, Hsieh LL, Chen JT, Chen CY, et al. The association of human papillomavirus 16/18 infection with lung cancer among non-smoking Taiwanese women. Cancer Res. 2001. 61:2799–2803.
9. Chiou HL, Wu MF, Liaw YC, Cheng YW, Wong RH, Chen CY, et al. The presence of human papillomavirus type 16/18 DNA in blood circulation may act as a risk marker of lung cancer in Taiwan. Cancer. 2003. 97:1558–1563.

10. Tsuhako K, Nakazato I, Hirayasu T, Sunakawa H, Iwamasa T. Human papillomavirus DNA in adenosquamous carcinoma of the lung. J Clin Pathol. 1998. 51:741–749.

11. Soini Y, Nuorva K, Kamel D, Pollanen R, Vahakangas K, Lehto VP, et al. Presence of human papillomavirus DNA and abnormal p53 protein accumulation in lung carcinoma. Thorax. 1996. 51:887–893.

12. Hirayasu T, Iwamasa T, Kamada Y, Koyanagi Y, Usuda H, Genka K. Human papillomavirus DNA in squamous cell carcinoma of the lung. J Clin Pathol. 1996. 49:810–817.

13. Hennig EM, Suo Z, Karlsen F, Holm R, Thoresen S, Nesland JM. HPV positive bronchopulmonary carcinomas in women with previous high-grade cervical intraepithelial neoplasia (CIN III). Acta Oncol. 1999. 38:639–647.

14. Shimada M, Fukushima M, Mukai H, Kato I, Nishikawa A, Fujinaga K. Amplification and specific detection of transforming gene region of human papillomavirus 16, 18 and 33 in cervical carcinoma by means of the polymerase chain reaction. Jpn J Cancer Res. 1990. 81:1–5.

15. Shamanin V, Delius H, de Villiers EM. Development of a broad spectrum PCR assay for papillomaviruses and its application in screening lung cancer biopsies. J Gen Virol. 1994. 75:1149–1156.

16. Szabo I, Sepp R, Nakamoto K, Maeda M, Sakamoto H, Uda H. Human papillomavirus not found in squamous and large cell lung carcinomas by polymerase chain reaction. Cancer. 1994. 73:2740–2744.

17. Welt A, Hummel M, Niedobitek G, Stein H. Human papillomavirus infection is not associated with bronchial carcinoma: evaluation by in situ hybridization and the polymerase chain reaction. J Pathol. 1997. 181:276–280.

18. Joo WD, Kim SH, Kim DY, Suh DS, Kim JH, Kim YM, et al. Prevalence of human papillomavirus infection in Korean women: risks of abnormal pap smear and cervical neoplasia. Korean Soc Gynecol Oncol Colposcopy. 2004. 15:309–316.

19. Skegg DC, Corwin PA, Paul C, Doll R. Importance of the male factor in cancer of the cervix. Lancet. 1982. 2:581–583.

20. Okinawa Prefectural Government. Annual statistical report of health and environment 1986-1995. 1995. Okinawa: Okinawa Prefectural Government.
21. Miyagi J, Tsuhako K, Kinjo T, Iwamasa T, Hirayasu T. Recent striking changes in histological differentiation and rate of human papillomavirus infection in squamous cell carcinoma of the lung in Okinawa, a subtropical island in southern Japan. J Clin Pathol. 2000. 53:676–684.

22. Miyagi J, Kinjo T, Tsuhako K, Higa M, Iwamasa T, Kamada Y, et al. Extremely high Langerhans cell infiltration contributes to the favourable prognosis of HPV-infected squamous cell carcinoma and adenocarcinoma of the lung. Histopathology. 2001. 38:355–367.

23. Clavel CE, Nawrocki B, Bosseaux B, Poitevin G, Putaud IC, Mangeonjean CC, et al. Detection of human papillomavirus DNA in bronchopulmonary carcinomas by hybrid capture II: a study of 185 tumors. Cancer. 2000. 88:1347–1352.

24. Hiroshima K, Toyozaki T, Iyoda A, Ohwada H, Kado S, Shirasawa H, et al. Ultrastructural study of intranuclear inclusion bodies of pulmonary adenocarcinoma. Ultrastruct Pathol. 1999. 23:383–389.

25. Yousem SA, Ohori NP, Sonmez-Alpan E. Occurrence of human papillomavirus DNA in primary lung neoplasms. Cancer. 1992. 69:693–697.

26. Bohlmeyer T, Le TN, Shroyer AL, Markham N, Shroyer KR. Detection of human papillomavirus in squamous cell carcinomas of the lung by polymerase chain reaction. Am J Respir Cell Mol Biol. 1998. 18:265–269.

27. Gorgoulis VG, Zacharatos P, Kotsinas A, Kyroudi A, Rassidakis AN, Ikonomopoulos JA, et al. Human papilloma virus (HPV) is possibly involved in laryngeal but not in lung carcinogenesis. Hum Pathol. 1999. 30:274–283.

28. Chen YC, Chen JH, Richard K, Chen PY, Christiani DC. Lung adenocarcinoma and human papillomavirus infection. Cancer. 2004. 101:1428–1436.

29. Gillison ML, Shah KV. Chapter 9: Role of mucosal human papillomavirus in nongenital cancers. J Natl Cancer Inst Monogr. 2003. 31:57–65.

30. Tseng CJ, Pao CC, Lin JD, Soong YK, Hong JH, Hsueh S. Detection of human papillomavirus types 16 and 18 mRNA in peripheral blood of advanced cervical cancer patients and its association with prognosis. J Clin Oncol. 1999. 17:1391–1396.

31. Capone RB, Pai SI, Koch WM, Gillison ML, Danish HN, Westra WH, et al. Detection and quantitation of human papillomavirus (HPV) DNA in the sera of patients with HPV-associated head and neck squamous cell carcinoma. Clin Cancer Res. 2000. 6:4171–4175.
32. Shyu JS, Chen CJ, Chiu CC, Huang SC, Harn HJ. Correlation of human papillomavirus 16 and 18 with cervical neoplasia in histological typing and clinical stage in Taiwan: an in-situ polymerase chain reaction approach. J Surg Oncol. 2001. 78:101–109.

33. Kurman RJ, Schiffman MH, Lancaster WD, Reid R, Jenson AB, Temple GF, et al. Analysis of individual human papillomavirus types in cervical neoplasia: a possible role for type 18 in rapid progression. Am J Obstet Gynecol. 1988. 159:293–296.

34. Walker J, Bloss JD, Liao SY, Berman M, Bergen S, Wilczynski SP, et al. Human papillomavirus genotype as a prognostic indicator in carcinoma of the uterine cervix. Obstet Gynecol. 1989. 74:781–785.
35. Barbosa MS, Edmonds C, Fisher C, Schiller JT, Lowy DR, Vousden KH, et al. The region of the HPV E7 oncoprotein homologous to adenovirus E1a and Sv40 large T antigen contains separate domains for Rb binding and casein kinase II phosphorylation. EMBO J. 1990. 9:153–160.

36. Dallenbach-Hellweg G, Lang G. Immunohistochemical studies on uterine tumors. Invasive squamous cell carcinomas of the cervix and their precursors. Pathol Res Pract. 1991. 187:36–43.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download