Abstract
Purpose
This study aimed to evaluate the cancer detection rate in a Korean population with prostate-specific antigen (PSA) levels greater than or equal to 20.0ng/mL.
Materials and Methods
A total of 174 men 50 to 79 years old (median 69) included in the study. The median prostate volume of the patients was 44.8mL (range 14.1 to 210.0) and their serum PSA ranged from 20.0 to 9725.0ng/mL (median 44.8).
Results
Of 174 men 141 (81.0%) were diagnosed with prostate cancer on initial biopsy. In the total number of patients, the positive predictive value (PPV) was 62.9% for PSA 20 to 29.9, 72.7% for PSA 30 to 39.9 and 100% for PSA 40 to 49.9ng/mL. In patients with an abnormal digital rectal examination (DRE), the values for these PSA ranges increased to 89.5%, 91.7% and 100%, respectively. The PPV was 81.0% for PSA cutoff of 20, 89.2% for a cutoff of 30, 95.4% for a cutoff of 40, and 94.7% for a cutoff of 50ng/mL. In conjunction with an abnormal DRE, the values for these PSA cutoffs increased to 95.9%, 98.1%, 100%, and 100%, respectively.
Conclusion
Our data suggest the ability to predict the presence of prostate cancer reliably on initial biopsy when PSA threshold is greater than or equal to 50ng/mL. This PSA threshold may be lowered to 40ng/mL in the presence of an abnormal DRE. In Korean men with high PSA, the detection rate of prostate cancer on biopsy appears to be comparable to that for American men.
There is general agreement among clinicians that the prostate-specific antigen (PSA) test has the highest predictive value for prostate cancer.1 Widespread use of PSA resulted in a downward trend in clinical and pathologic stages of prostate cancer. A serum PSA cutoff of 4ng/mL is most often used for early detection of prostate cancer. The probability of cancer is around 25% if serum PSA is between 4.1 and 10ng/mL and it is estimated that the probability of cancer is more than 30%.when serum PSA is higher than 10ng/mL2,3 However, to date, information on the prevalence of biopsy-detectable prostate cancer among men with PSA values of 20.0ng/mL or greater is limited.4,5 Furthermore, information on the accuracy of high PSA for prostate cancer diagnosis among Asian men is also scarce. Serum PSA concentration is known to be different across the ethnic groups.6,7 Thus, a given PSA value may have different clinical meaning for patients of different races. We evaluated the cancer detection rate in a Korean population with PSA levels greater than or equal to 20.0ng/mL.
We reviewed the records of 1369 patients undergoing a transrectal ultrasonography (TRUS)-guided prostate biopsy at the Department of Urology in three hospitals. We enrolled individuals who visited our department for a variety of reasons, including prostate cancer screening and voiding symptoms, regardless of whether the visit was primary or referred. Patents with an abnormal digital rectal examination (DRE) and/or a serum PSA level greater than 2.0ng/mL underwent a biopsy by a radiologist after patients provided written informed consent.
All men underwent detailed clinical examinations, including determination of serum levels of total PSA quantified by immunoradiometric assay (Izotop, Hungary), DRE, and TRUS. Blood samples were obtained before patients were examined by a physician. All blood was stored at -70℃ for less than 1 week and assayed for serum PSA concentration. Transaxial and sagittal scanning of the prostate was performed by radiologist experienced in this procedure using a 7.0-MHz transducer (Ultramake 9, ATL Inc., Washington, D.C., USA). In specimens diagnosed as prostate cancer, additional review was performed using the Gleason score and the percentage of cancer cores (number of cores involved with cancer divided by the total number of biopsy cores).
Men were excluded from the analysis if they had previously undergone prostate biopsy, had received a prior diagnosis of prostate cancer, had undergone prostate surgery or radiation treatment, had a serum PSA less than 20ng/mL, had received 5α-reductase inhibitors, had acute urinary retention or an indwelling catheter, had a duration of more than 3 months between PSA measurement and biopsy, or evidence of an acute urinary infection (pyuria and bacteriuria) on urinalysis. A total of 174 men met these criteria and constituted the study cohort. In patients examined, their median age was 69 years (range 50 to 89). The median prostate volume of the patients was 44.8mL (range 14.1 to 210.0) and their serum PSA ranged from 20.0 to 9725.0ng/mL (median 44.8).
Values of continuous variables are presented as median (range) and rates are expressed as a number (%). Patients were divided to the cancer group and the no cancer group. Comparisons of data were made using the chi-square test for categorical variables and Mann-Whitney U test for continuous variables. A 5% level of significance was used for all statistical testing and all statistical tests were 2-sided. The accuracy of PSA, alone or in conjunction with DRE findings, in predicting cancer was determined for these patients. Positive predictive values (PPVs) were calculated for PSA ranges and PSA cutoffs. The statistical software package SPSS 10.0 (SPSS, Inc., Chicago, IL, USA) was used for all statistical analyses.
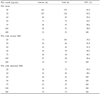
Of the 174 men, 141 (81.0%) were diagnosed with prostate cancer on initial biopsy. Characteristics of patients with and without cancer and their prostatic histology are reported in Table 1. Patients who were diagnosed with cancer on initial biopsy were older (p = 0.018), had greater PSA levels (p < 0.001), had smaller prostates (p < 0.001), and had more abnormal DRE findings (p < 0.001) than those who did not. No statistically significant differences in number of cores per biopsy between the two groups were seen but core density (number of cores divided with prostate volume) was higher in the cancer group (p = 0.004).
The PPVs of different serum PSA ranges, alone or in combination with DRE findings, are listed in Table 2. In the total number of patients, the PPV was 62.9% for PSA levels 20 to 29.9, 72.7% for PSA levels 30 to 39.9 and 100% for PSA levels 40 to 49.9ng/mL. In patients with an abnormal DRE, the values for these PSA ranges increased to 89.5%, 91.7% and 100%, respectively. There was a trend that Gleason score and percentage of cancer core increased with an increasing serum PSA level.
Table 3 lists the PPVs for various PSA cutoffs, alone or in combination with DRE findings. The PPV was 81.0% for PSA cutoff of 20, 89.2% for a cutoff of 30, 95.4% for a cutoff of 40, and 94.7% for a cutoff of 50ng/mL. In conjunction with an abnormal DRE, the values for these PSA cutoffs increased to 95.9%, 98.1%, 100%, and 100%, respectively.
Subranges of serum PSA levels have been used to help counsel men with regard to the detection rate of cancer on biopsy. This is the basic information used by patients and clinicians to determine whether a prostate biopsy is necessary. The probability of cancer is around 25% if serum PSA is between 4.1 and 10ng/mL, and it is estimated that the probability of cancer when serum PSA is higher than 10ng/mL is more than 30%.2,3 The detection rate of prostate cancer with a low PSA value in Korean men and Japanese men is lower than that in American men.7-10 In studies on Korean men, the cancer detection rate for PSA subgroups of 4ng or more to less than 10ng/mL was 13.8% and 15.9%.8,9 This is similar to the 15.8% rate in Japanese men reported by Egawa et al.10 In a meta-analysis using results from the Korean literature, the pooled sensitivity and specificity for a PSA level greater than 4ng/mL were 91.3% and 35.9%, respectively.11
It is well known that as PSA levels significantly increase, it becomes a more reliable tumor marker. Serum PSA levels greater than 20ng/mL have been associated with cancer detection rates greater than 70% and it is uncommon for benign prostatic hyperplasia or chronic prostatitis to increase PSA to extremely high levels without concurrent cancer in the gland.4,12,13 Our analysis demonstrated that a serum PSA level greater than or equal to 20ng/mL, independent of DRE findings, was 81.0% accurate in predicting the presence of prostate cancer on initial biopsy. A serum PSA level greater than or equal to 50ng/mL had a PPV of 94.7%. An abnormal DRE improved the accuracy of PSA in predicting malignancy over PSA alone. For a PSA cutoff of 40ng/mL, when combined with an abnormal DRE, the PPV was 100%. These findings are consistent with previous studies.4,5 Heyns et al.4 reported a PPV of 90% for PSA greater than 30ng/mL and a PPV of 98% for PSA greater than 60ng/mL. Gerstenbluth et al.5 demonstrated that a serum PSA level of 20ng/mL or greater, independent of DRE findings, was 87.2% accurate in predicting the cancer and a serum PSA level of 50ng/mL or greater had a PPV of 98.5%.
To our knowledge, this is the first study to evaluate the cancer detection rate in Asian men with PSA levels greater than or equal to 20.0ng/mL. Our data suggest the ability to predict prostate cancer reliably on the initial biopsy when the PSA threshold is greater than or equal to 50ng/mL. This PSA threshold may be lowered to 40ng/mL in the presence of an abnormal DRE. Our findings show that, even though the PPVs were lower in Korean men with low-end high pSA levels, detection of prostate cancer on biopsy appears to be comparable to American men.5
The exact reason for no discrepancy in the PPV for high PSA values between Korean men and Western population is not certain. The incidence of prostate cancer has been reported to vary widely in different parts of the world, with the highest recorded in North America and Western Europe. The incidence of prostate cancer in Asian men is clearly increasing due to the widespread use of the serum PSA level test and possibly to the changing dietary habits of Asian men, but it is still much lower than those in Western countries. This variation may in part reflect racial differences in the incidence of prostate cancer. However, at least 30% of Japanese men aged > 50 years of age have histological evidence of prostate cancer, which is similar to the rate in Western countries.14,15 Differences in the incidence of prostate cancer among racial groups are not necessarily reflected in the mean PSA values; e.g. no substantial differences in PSA levels between native Japanese and Japanese-American men have been found, even though there are substantial differences in prostate cancer incidence between these groups.16 Thus, prostate cancer incidence in many high-risk countries is likely to be affected by aggressive screening in their population, while the lack of screening, the lower quality of cancer diagnosis, and the incompleteness of cancer registration may contribute to some underreporting in some low-risk populations.17 Therefore, to address this question, a more extensive study focusing on this subject is needed.
Knowledge of the PPVs presented in this study may be important for counseling Asian men with high PSA before they undergo biopsy. From a recent series of studies, the estimated major complication rate of the procedure, defined as a need for hospitalization or intravenous therapy, was only 1.9%.18 However, although prostate biopsy is a relatively uncomplicated procedure with minimal morbidity, an elderly patient with severe co-morbidities or on anticoagulation may not be an optimal candidate for the procedure. These patients may benefit from having prostate biopsy omitted if serum PSA is greater than 50ng/mL or if serum PSA is greater than 40ng/mL in the presence of abnormal DRE.
Some issues of the current study should be mentioned. Our study was not a community-based one. Our aim had not been to estimate the epidemiologic incidence of prostate cancer in men with high PSA levels but was to evaluate the rate of prostate cancer detection in these men in our daily practice. However, the predictive value of the screening tests may be different in patients presenting with symptoms as opposed to the general population. Thus, our data cannot be applied to population-based screening. In addition, in our study, patients did not undergo a repeat biopsy after a negative initial biopsy. Since a negative biopsy for an increased PSA greater than 20ng/mL is often false-negative,4,5 the study may underestimate the accuracy of PSA.
Figures and Tables
References
1. Carter HB. Prostate cancers in men with low PSA levels-must we find them? N Engl J Med. 2004. 350:292–294.
2. Catalona WJ, Richie JP, deKernion JB, Ahmann FR, Ratliff TL, Dalkin L, et al. Comparison of prostate specific antigen concentration versus prostate specific antigen density in the early detection of prostate cancer: receiver operating characteristic curves. J Urol. 1994. 152:2031–2036.

3. Cooner WH, Mosley BR, Rutherford CL, Beard JH, Pond HS, Terry WJ, et al. Prostate cancer detection in a clinical urological practice by ultrasonography, digital rectal examination and prostate specific antigen. J Urol. 1990. 143:1146–1152.

4. Heyns CF, Naudé AM, Ahmed G, Stopforth HB, Stellmacher GA, Visser AJ. Serum prostate-specific antigen as surrogate for the histological diagnosis of prostate cancer. S Afr Med J. 2001. 91:685–689.
5. Gerstenbluth RE, Seftel AD, Hampel N, Oefelein MG, Resnick MI. The accuracy of the increased prostate specific antigen level (greater than or equal to 20ng./ml.) in predicting prostate cancer: is biopsy always required? J Urol. 2002. 168:1990–1993.

6. Masumori N, Tsukamoto T, Kumamoto Y, Miyake H, Rhodes T, Girman CJ, et al. Japanese men have smaller prostate volumes but comparable urinary flow rates relative to American men: results of community based studies in 2 countries. J Urol. 1996. 155:1324–1327.

7. Ku JH. Race-specific reference ranges of serum prostate-specific antigen levels in countries with a low incidence of prostate cancer. BJU Int. 2006. 97:69–72.

8. Kim JW, Lee HY, Hong SJ, Chung BH. Can a 12 core prostate biopsy increase the detection rate of prostate cancer versus 6 core?: a prospective randomized study in Korea. Yonsei Med J. 2004. 45:671–675.

9. Yang WJ, Lee DH, Chung BH, Cho JS, Choi YD, Kim SJ, et al. Detection rate of prostate cancer on biopsy according to serum prostate-specific antigen in Korean men: a multicenter study. Urology. 2006. 67:333–336.

10. Egawa S, Matsumoto K, Yoshida K, Iwamura M, Kuwao S, Koshiba K. Results of transrectal ultrasound-guided biopsies and clinical significance of Japanese prostate cancer. Jpn J Clin Oncol. 1998. 28:666–672.

11. Song JM, Kim CB, Chung HC, Kane RL. Prostate-specific antigen, digital rectal examination and transrectal ultrasonography: a meta-analysis for this diagnostic triad of prostate cancer in symptomatic Korean men. Yonsei Med J. 2005. 46:414–424.

12. Labrie F, Dupont A, Suburu R, Cusan L, Tremblay M, Gomez JL, et al. Serum prostate specific antigen as pre-screening test for prostate cancer. J Urol. 1992. 147:846–852.

13. Orozco R, O'Dowd G, Kunnel B, Miller MC, Veltri RW. Observations on pathology trends in 62,537 prostate biopsies obtained from urology private practices in the United States. Urology. 1998. 51:186–195.

14. Yatani R, Shiraishi T, Nakakuki K, Kusano I, Takanari H, Hayashi T, et al. Trends in frequency of latent prostate carcinoma in Japan from 1965-1979 to 1982-1986. J Natl Cancer Inst. 1988. 80:683–687.

15. Sakr WA, Haas GP, Cassin BF, Pontes JE, Crissman JD. The frequency of carcinoma and intraepithelial neoplasia of the prostate in young male patients. J Urol. 1993. 150:379–385.

16. Shibata A, Whittemore AS, Imai K, Kolonel LN, Wu AH, John EM, et al. Serum levels of prostate-specific antigen among Japanese-American and native Japanese men. J Natl Cancer Inst. 1997. 89:1716–1720.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download