Abstract
Purpose
Fast MRI has provided detailed and reproducible fetal anatomy. This study was performed to evaluate the usefulness of fetal MRI for prenatal diagnosis.
Materials and Methods
Fifty-six fetuses with congenital abnormalities on ultrasonography were evaluated by fetal MRI from 2001 to 2004 in Severance Hospital. Final diagnosis was made by postnatal pathology, postnatal MRI, and other modalities (such as ultrasound, retrograde pyelogram). A 1.5-Tesla superconductive MR imaging unit was used to obtain half-Fourier acquisition single-shot turbo spin images.
Results
Of the 56 fetuses, intracranial abnormalities were found in 26 fetuses, intraabdominal abnormalities in 17 fetuses, intrathoracic in 6 fetuses, head and neck in 5 fetuses, and other sites in 2 fetuses. There were six cases in which the diagnoses of fetal MRI and ultrasonography differed. In such cases, fetal MRI provided more exact diagnosis than ultrasonography (5 vs. 0). Three fetuses with intracranial abnormalities on ultrasonography were diagnosed as normal by fetal MRI and in postnatal diagnosis.
Conclusion
Although ultrasonography is known as a screening modality of choice in the evaluation of fetus because of the cost-effectiveness and safety, the sonographic findings are occasionally inconclusive or insufficient for choosing the proper management. Thus, in this study, we suggest that fetal MRI is more useful than ultrasonography for the evaluation of intracranial abnormalities in some instances. For prenatal counseling and postnatal treatment planning, fetal MRI can be informative when prenatal ultrasonography is inadequate and doubtful.
Ultrasonography is the primary screening modality for fetal imaging because of its relative low cost, lack of harmful effects to the fetus or mother, and real time imaging, among other advantages. However, there are limitations, including small field of view, limited soft-tissue acoustic contrast, beam attenuation by adipose tissue, poor image quality in oligohydramnios, and limited visualization of the posterior fossa after 33 weeks' gestation because of calvarial calcification.1-3 In the past, we have needed additional information regarding fetal anatomy or pathology to make a decision in prenatal care and in some cases abnormalities could not be adequately assessed with ultrasound. In such cases, fetal MRI can be the alternative imaging modality. Taking an MRI of a pregnant woman was first described in 1983,4 but the initial obstetric applications were primarily related to maternal and placental abnormalities.5 Fetal MRI was first introduced to Korea in the early 1990s but was rarely used due to image degradation by fetal motion on a standard sequence and the relatively long acquisition time.6 Since the late 1990s, with ultrafast MRI techniques such as single-shot fast-spin echo and half-Fourier acquisition turbo spin echo (HASTE), fetal motion artifacts are minimized and fetal MRI is playing an increasingly important role in the diagnosis of fetal abnormalities.7 Fetal MRI provides diagnostic accuracy in evaluating fetal brain, spine, neck, chest, abdomen, and urinary tract and it provides important anatomic information that can be helpful in planning antenatal care and surgical procedures.8 Despite the effectiveness of fetal MRI, there has been little study in Korea about the indications and the usefulness of fetal MRI; thus, in this study we chose to evaluate the usefulness of fetal MRI for prenatal diagnosis.
We retrospectively reviewed 56 cases in which fetal MRIs were taken from January 2001 to December 2004 with the intent to make more accurate diagnoses and to detect more fetal abnormalities following abnormal prenatal ultrasonographic findings. The fetal MRIs were performed with informed consent. We selected 30 cases of which final diagnoses were confirmed. We analyzed the 30 cases according to the systems affected and compared the official reading from each modality to the final diagnosis. We excluded cases with cardiac abnormalities because it is a well known fact that fetal MRI is inappropriate for evaluating those cases. In cases where two or more abnormalities coexisted in antenatal ultrasonography, we chose the one associated with the reason for taking fetal MRI. We used Aloka SSD 5500 and Acuson Sequoia for antenatal ultrasonography. A 1.5-Tesla superconductive MR imaging unit was used to obtain HASTE images. The final diagnosis was confirmed by postoperative biopsy, postnatal MRI, and other modalities including ultrasonography, esophagogram, and others.
We were able to confirm the final diagnosis in 30 out of 56 cases. Twenty-two cases were lost in follow-up; in four cases, an autopsy after intrauterine fetal death was denied by the parents. In 56 cases total, fetal MRI was performed for 26 possible cases of intracranial abnormalities, 17 intraabdominal abnormality cases, six intrathoracic abnormality cases, six head and neck abnormality cases, and two cases of other abnormalities (Fig. 1). The most common indication in the intracranial abnormality group for taking fetal MRI was agenesis of the corpus callosum and Dandy-Walker variant and malformation (seven cases each), followed by ventriculomegaly, and then arachnoid cyst (Table 1). As for the time of MRI examination, the fetal MRI was taken between 32 and 35 gestational weeks in 19 cases, between 24 and 27 gestational weeks in 16 cases, and between 28 and 31 gestational weeks in 11 cases. The earliest case was taken at 22 gestational weeks. Among the 30 cases of which the final diagnoses were confirmed, intraabdominal abnormalities were the most common (12 cases), followed by intracranial abnormalities (9 cases), intrathoracic abnormalities (5 cases), head and neck abnormalities (2 cases), and other (2 cases). In 6 out of the 30 cases, the official readings of antenatal ultrasonography differed from those of the fetal MRI (Table 2). Out of those six cases, fetal MRI readings were coincident with the final diagnosis in five cases. In the remaining case, the official readings of both modalities were different from the final diagnosis.
There were nine cases of intracranial abnormalities in the final diagnosis confirmed group. In three cases (suspicious of Dandy-Walker variant {two cases}, Lissencephaly {one case}), the final diagnoses turned out normal, which were coincident with the official reading of fetal MRI. In one case, intracranial hemorrhage was suspected by prenatal ultrasonography, and papilloma by fetal MRI, but the final diagnosis by tissue biopsy was harmatoma. In addition, two cases which showed no specific abnormality except ventriculomegaly in prenatal ultrasonography showed no additional abnormality in both the fetal MRI and final diagnosis. Fig. 2 represents a case in which arachnoid cyst was suspected by prenatal ultrasonography and later turned out to be ACC (agenesis of corpus callosum) by fetal MRI (final diagnosis was not confirmed). A case diagnosed as suspicious Dandy-Walker variant by ultrasonography due to mild cisterna magna enlargement and defect of cerebellar inferior vermis was later diagnosed as Dandy-Walker malformation by fetal MRI since it showed a definite connection between the 4th ventricle and an enlarged cisterna magna (Fig. 3).
In 12 of 17 intraabdominal abnormality cases, the final diagnoses were confirmed. Of the 12 cases, MRI was taken due to suspicious renal agenesis or dysplastic kidney in four cases, renal or adrenal mass in four cases, and gastrointestinal tract obstruction in four cases. In two cases, the official readings of ultrasonography were different from those of fetal MRI. In one case, the reading was left renal agenesis in ultrasonography and both normal in fetal MRI and the final diagnosis. The other case was ultrasonographically diagnosed with a tracheoesophageal fistula or esophageal atresia but there was no dilated pouch in the fetal MRI images, and the case turned out to be normal in postpartum esophagogram. Fig. 4 shows a case diagnosed as suspicious as either an ovarian cyst or meconium pseudocyst by ultrasonography but was later diagnosed to be a small bowel obstruction with meconium pseudocyst by both fetal MRI and postnatal pathology.
In six cases, fetal MRI was taken due to suspicion of chest abnormalities. Four cases were suspected to be pulmonary sequestration or CCAM (congenital cystic adenomatoid malformation) and the other two as congenital diaphragmatic hernias. In five of the six cases, final diagnoses were confirmed. In those five cases, the official readings of both modalities were identical.
Ultrasonography has been the modality of choice in evaluating fetal well-being and detecting fetal structural abnormality, but has shown several shortcomings in some cases. In such cases, fetal MRI can provide useful information that ultrasonography cannot provide for making a therapeutic plan. Nowadays, we use fetal MRI to evaluate some fetal abnormalities such as complete or partial ACC, malformation of posterior fossa, bilateral renal agenesis, and congenital diaphragmatic hernia.9 Since the impact of taking fetal MRI on fetal organogenesis was not fully known, the modality has been usually applied after the 2nd trimester, with little adverse effect reported.10-13 The Safety Committee of the Society for MR imaging concluded that prenatal MR imaging is indicated when other non-ionizing methods are inadequate or when the MR examinations will provide critical information that would otherwise require the use of ionizing radiation.14 As for the intravenous contrast media, since there is no proven level of safety, its use is prohibited.15 The effectiveness of fetal MRI as an optional modality of detecting fetal abnormalities, which was already well known, was reaffirmed by this study. In this study, in 6 out of 30 cases with confirmed final diagnosis, the final diagnosis was changed after taking a fetal MRI. Moreover, in five cases, the outcome of fetal MRI turned out to be true. However, there is little statistical evidence supporting the accuracy of fetal MRI, because of follow-up losses, including pregnancy termination and transferal to other hospitals. The same is true in this study, for we were able to obtain only 30 cases with confirmed final diagnosis out of 56 cases with fetal MRI data available (54%). Fetal MRI has an advantage over ultrasonography in evaluating and diagnosing posterior fossa abnormalities, brain development according to neuronal migration, gyral formation, and myelination.16 In intracranial abnormalities, it is known that the common indication for taking fetal MRI includes ventriculomegaly, agenesis corpus callosum, Dandy-Walker malformation or variant, arachnoid cyst, and holoprosencephaly.17 In cases of ventriculomegaly, the prognosis is poor because the fetuses with ventriculomegaly are usually (in 70-84% of cases) associated with other malformations in the central nervous system and with mental retardation.18-22 The most common reason for taking fetal MRI in this study was also agenesis corpus callosum, Dandy-Walker malformation or variant, and ventriculomegaly. This study shows the usefulness of taking fetal MRI. In three out of nine cases with suspicious intracranial abnormalities, the final diagnoses were changed and those changes were consistent with the results of the fetal MRI. As for intrathoracic abnormalities, the results of ultrasonography and fetal MRI were not so different from each other in this study, but the cases of intrathoracic abnormalities were too small to determine the usefulness of taking a fetal MRI. It is known that fetal MRI is superior to ultrasonography in calculating lung volume and herniated liver volume so as to predict postnatal prognosis and in diagnosing atypical intrathoracic mass.23 Fetal MRI is also known to be useful for evaluating the location of a bowel obstruction and intraabdominal tumors, identifying the different portions of the bowel, and diagnosing renal agenesis.24 In this study, the diagnosis was changed in two cases of intraabdominal abnormalities after taking a fetal MRI, which was coincident with the final diagnosis. The most common neck masses are cystic hygromas, teratomas, and goiters. A fetal MRI characterizes the lesion and defines the relationship to the airway and major neck vessels.25 But, in this study, fetal MRI did not provide additional information above the sonogram in diagnosing cystic hygroma of the neck.
Although ultrasonography provides abundant information in evaluating fetal structural abnormalities and fetal well-being, the ultrasonographic findings are occasionally inconclusive or insufficient for choosing proper management and prenatal counseling. In these cases, alternative imaging with magnetic resonance can be helpful. So, in this study, we suggest that fetal MRI is useful for the evaluation of intracranial and intraabdominal abnormalities in some cases but not in diagnosing other abnormalities. Further studies are needed, however, to decide the proper indications for fetal MRI. In the future, improvements in MRI and ultrasonographic technology will improve our ability to assess fetuses.
Figures and Tables
Fig. 1
Number of cases according to affected organ. *Soft tissue mass in right leg, sacrococcygeal teratoma.

Fig. 2
Agenesis of corpus callosum in a fetus at 24 weeks' gestation. (A) Arachnoid cyst (arrow head) was suggested in axial sonogram. There was neither ventriculomegaly nor a tear-drop sign in sonographic findings. But, sagittal (B) and coronal (C) magnetic resonance images clearly demonstrated a lack of normal connecting white matter fiber.

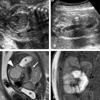
Fig. 3
A case diagnosed as suspicious of Dandy-Walker variant by ultrasonography at 26 weeks' gestation due to mild ventricular enlargement (A) and enlarged cisterna magna (B). Transaxial magnetic resonance image shows direct communication between the 4th ventricle and cisterna magna (C) and sagittal magnetic resonance image shows enlarged posterior fossa (D). This case was diagnosed as Dandy-Walker malformation by fetal MRI.

Fig. 4
A case diagnosed as suspicious of fetal ovarian cyst or meconium pseudocyst by ultrasonography at 24 weeks' gestation. A. Coronal sonogram demonstrates well defined heterogeneous echogenic round mass in the fetal abdomen. B. Axial sonogram shows a dilated fetal small bowel. Same patient at 26 weeks' gestation, T2-W sequence (C) and T1-W sequence (D). C. Sagittal scan shows well defined large cystic structure (arrow head) and dilated bowel loops (arrow) with same intermediate signal. (Bl; urinary bladder, S; stomach) D. Coronal scan shows dilated loops with meconium-like signal (black arrows). This case was diagnosed as small bowel obstruction with meconium pseudocyst in fetal MRI and later confirmed as jejunal atresia with meconium pseudocyst by postnatal pathology.
References
1. Garel C, Brisse H, Sebag G, Elmaleh M, Oury JF, Hassan M. Magnetic resonance imaging of the fetus. Pediatr Radiol. 1998. 28:201–211.

2. Angtuaco TL, Shah HR, Mattison DR, Quirk JG. MR imaging in high-risk obstetric patients: a valuable complement to US. Radiographics. 1992. 12:91–110.

3. Sonigo PC, Rypens FF, Carteret M, Delezoide AL, Brunelle FO. MR imaging of fetal cerebral anomalies. Pediatr Radiol. 1998. 28:212–222.

5. Stark DD, McCarthy SM, Filly RA, Parer JT, Hricak H, Callen PW. Pelvimetry by magnetic resonance imaging. AJR Am J Roentgenol. 1985. 144:947–950.

6. Yuh WT, Nguyen HD, Fisher DJ, Tali ET, Gao F, Simonson TM, et al. MR of fetal central nervous system abnormalities. AJNR Am J Neuroradiol. 1994. 15:459–464.
7. Levine D, Barnes PD, Sher S, Semelka RC, Li W, McArdle CR, et al. Fetal fast MR imaging: reproducibility, technical quality, and conspicuity of anatomy. Radiology. 1998. 206:549–554.

9. Ertl-Wagner B, Lienemann A, Strauss A, Reiser MF. Fetal magnetic resonance imaging: indications, technique, anatomical considerations and a review of fetal abnormalities. Eur Radiol. 2002. 12:1931–1940.

10. Wolff S, Crooks LE, Brown P, Howard R, Painter R. Tests for DNA and chromosomal damage induced by nuclear magnetic resonance imaging. Radiology. 1980. 136:707–710.

11. Schwartz JL, Crooks LE. NMR imaging produces no observable mutations or cytotoxicity in mammalian cells. AJR Am J Roentgenol. 1982. 139:583–585.

12. Kanal E, Gillen J, Evans JA, Savitz DA, Shellock FG. Survey of reproductive health among female MR workers. Radiology. 1993. 187:395–399.

13. Baker PN, Johnson IR, Harvey PR, Gowland PA, Mansfield P. A three-year follow-up of children imaged in utero with echo-planar magnetic resonance. Am J Obstet Gynecol. 1994. 170:32–33.

14. Shellock FG, Kanal E. Policies, guidelines, and recommendations for MR imaging safety and patient management. SMRI safety Committee. J Magn Reson Imaging. 1991. 1:97–101.

15. Shellock FG, Kanal E. Edelman RR, Hesselink JR, Zlatkin MB, editors. Bioeffects and safety of MR procedures. Clinical magnetic resonance imaging. 1996. 2nd ed. Philadelphia: Saunders;429.
16. Hubbard AM, Harty MP, States LJ. A new tool for prenatal diagnosis: ultrafast fetal MRI. Semin Perinatol. 1999. 23:437–447.

17. Blaicher W, Prayer D, Bernaschek G. Magnetic resonance imaging and ultrasound in the assessment of the fetal central nervous system. J Perinat Med. 2003. 31:459–468.

18. Pretorius DH, Davis K, Manco-Johnson ML, Manchester D, Meier PR, Clewell WH. Clinical course of fetal hydrocephalus: 40 cases. AJR Am J Roentgenol. 1985. 144:827–831.

19. Nyberg DA, Mack LA, Hirsch J, Pagon RO, Shepard TH. Fetal hydrocephalus: sonographic detection and clinical significance of associated anomalies. Radiology. 1987. 163:187–191.

20. Vintzileos AM, Campbell WA, Weinbaum PJ, Nochimson DJ. Perinatal management and outcome of fetal ventriculomegaly. Obstet Gynecol. 1987. 69:5–11.
21. Cochrane DD, Myles ST, Nimrod C, Still DK, Sugarman RG, Wittmann BK. Intrauterine hydrocephalus and ventriculomegaly: associated anomalies and fetal outcome. Can J Neurol Sci. 1985. 12:51–59.

22. Chervenak FA, Duncan C, Ment LR, Hobbins JC, McClure M, Scott D, et al. Outcome of fetal ventriculomegaly. Lancet. 1984. 2:179–181.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download