Abstract
Purpose
Since 1993, Koreans have used diagnostic criteria set by the Korean Society on Thrombosis and Hemostasis (KSTH) in the diagnosis of overt disseminated intravascular coagulation (DIC). In 2001, the Scientific and Standardization Committee (SCC) of the International Society on Thrombosis and Hemostasis (ISTH) proposed new diagnostic criteria for the diagnosis of overt DIC. We wanted to compare the use of the ISTH versus KSTH criteria in the diagnosis of overt DIC.
Materials and Methods
We enrolled 131 patients over the age of 15 years, who had been admitted and diagnosed as having DIC from May 2000 to April 2005 at the Youngdong Severance Hospital, Seoul, Korea. Of the 131 patients, there were 71 males and 60 females, with a median age of 61 years. Hemostatic tests, including platelet counts, PT, aPTT, fibrinogen level and D-dimer, were evaluated based on the respective scoring systems. To assess the concordance between the two diagnostic systems, we used the Student's t-test and the K-coefficient.
Results
There were 79 patients compatible with the ISTH criteria and 63 patients with the KSTH criteria. Sixty-one patients were compatible with both diagnostic systems. The grade of agreement, or concordance rate, was 84.7% and the K-coefficient, or interrater reliability, was as low as 0.6 without significance. However, if we scored 1 point for a fibrinogen level of 100-150mg/dL, and 2 points for a level below 100mg/dL, for the ISTH criteria, then 63 patients were compatible with both diagnostic systems, and the concordance rate increased to 85.5% and the K-coefficient to 0.71 with significance.
Disseminated intravascular coagulation (DIC) is characterized by hyperactivation of systemic blood coagulation resulting in the consumption of platelets and coagulation factors and possibly leading to severe bleeding. Fibrinolytic activities are depressed and fibrin deposition occurs in microcirculation, contributing to multiple organ failure. DIC is frequently associated with severe infections, malignant diseases, obstetrical disorders, and traumas. Most clinicians are familiar with the clinical features of DIC, but the exact diagnostic approach is speculative. The early diagnosis and prompt treatment of DIC are very important and can improve the outcome. Since 1993, Koreans have used the criteria set by the Korean Society on Thrombosis and Hemostasis (KSTH) in the diagnosis of overt DICs. But in 2001, the Scientific and Standardization Committee (SCC) of the International Society on Thrombosis and Hemostasis (ISTH) proposed new diagnostic criteria for the diagnosis of overt DIC. Therefore, we sought to assess the usefulness of the ISTH criteria over the KSTH criteria in the diagnosis of overt DICs.
For this retrospective study, we enrolled 131 patients over the age of 15 years, who were consecutively admitted for DIC based on medical records from May 2000 to April 2005 in Youngdong Severance Hospital, Seoul, Korea.
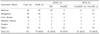
Global hemostatic tests, including platelet counts, PT, aPTT, plasma fibrinogen level and D-dimer, were confirmed from medical records and overt DIC was diagnosed based on both scoring systems (Table 1).1,2
Characteristics of each criterion were analyzed by the Student's t-test and a p value less than 0.05 was denoted as significant.
The grade of agreement between the two diagnostic systems, represented by the concordance rate and k-coefficient, were calculated and a k-coefficient more than 0.7 was denoted as significant.
Of the 131 patients enrolled in this study, there were 71 males and 60 females, with a male to female ratio of 1:0.85. The patients ranged in age from 17 to 91 years, with a median age of 61.0 years.
The primary underlying causative disease was infection, followed by malignancy and liver disease (Table 2).
The mortality rate was 60.0% as a whole, 65.9% according to KSTH criteria and 63.4% according to ISTH criteria (Table 3).
Among the 131 patients diagnosed with DIC, there were 79 overt DIC patients by ISTH criteria and 63 were compatible with KSTH criteria. Sixty-one patients were compatible with the two diagnostic systems simultaneously.
The concordance rate was high at 84.7% but the k-coefficient was low at 0.6 without significance (Table 4).
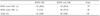
The diagnosis of DIC patients with the ISTH criteria resulted in a significantly lower mean value for platelet count and a significantly higher mean value for D-dimer than diagnosis with KSTH criteria. However, there were no differences in values for PT, aPTT, and plasma fibrinogen levels between the two diagnostic criteria sets (Table 5). There was only a small decrease in plasma fibrinogen levels for ISTH and KSTH criteria-based diagnosis (Table 6).
If we scored 1 point for a plasma fibrinogen level less than 150mg/dL according to the ISTH criteria, there were 2 additional patients, for a total 63 patients, that were compatible with the two diagnostic systems, resulting in a concordance rate of 85.5% and a k-coefficient of 0.71 with significance.
Therefore, to improve the diagnostic sensitivity for DIC using the ISTH criteria, it may be better to score 1 point for a fibrinogen level of 100-150mg/dL and 2 points for a level below 100mg/dL.
Disseminated intravascular coagulation (DIC) is usually associated with several predisposing clinical causes and few data have been reported during the last decade in Korea.3-5 In our study, infectious diseases were the most common causes of DIC, followed by malignant diseases and liver diseases.
The frequency of infectious cause found using the KSTH criteria (38.1%) was almost the same as that found with ISTH criteria (36.6%). Also, the frequency of malignant disease found using the KSTH criteria (17.4%) was almost the same as that found with the ISTH criteria (19.5%) and was very similar to frequencies found in previous Korean reports.3-5
In this study, the mortality rates were 60.0% as a whole, 65.9% with KSTH criteria and 63.4% with ISTH criteria. The mortality rate in DIC was somewhat high (50-80%) in early foreign reports,6,7 but somewhat lower in Korean reports (36-50%).3,5 But our study showed more than 60% mortality and such high mortality rate might be due to the infectious causes of DIC.
The rate of concordance in the diagnosis of overt DIC by ISTH criteria and by KSTH criteria was 84.7%. This agreement is higher than that of a Japanese report (67.4%) in which only 2.0% of non-DIC patients according to the Japanese Ministry of Health and Welfare (JMHW) criteria were diagnosed with overt DIC according to the ISTH criteria. In contrast, our study showed that a more percentage (22.5%) of non-DIC patients according to the KSTH criteria were diagnosed with overt DIC according to the ISTH criteria.8 Our k-coefficient, or interrater reliability, was 0.6 with no significance. One previous Korean report showed a concordance rate of 89.5% and a k-coefficient of 0.78 with significance.9 But our study showed a lower k-coefficient value without significance.
Although clinical symptoms and other signs are recommended in the diagnosis of overt DIC,8 they are not objective, so we decided not to include the clinical assessment as recommended by the SCC.1
Abnormalities in global hemostatic tests such as platelet counts, PT, and aPTT, are easily detected. Under the ISTH criteria, these laboratory values are more precisely scored. The mean value for platelet count was significantly lower in overt DIC patients with the ISTH criteria than with the KSTH criteria, which is similar to results from other reports.8,9 PT and aPTT can be easily used by calculating the prolongation of their values.
D-dimer levels were also significantly increased in ISTH-diagnosed DIC patients compared to KSTH-diagnosed DIC patients, as observed in other reports.8,9
Plasma fibrinogen levels only differed by a small amount between the ISTH-diagnosed and KSTH-diagnosed DIC patients but is still a specific marker for overt DIC diagnosis.
Plasma fibrinogen level is only scored as 1 point if below 100mg/dL according to ISTH overt DIC criteria, but if we scored 1 point for a fibrinogen level of 100-150mg/dL and 2 points for a level below 100mg/dL, the concordance rate increased to 87.0% and the k-coefficient to 0.71 with significance.
The ISTH criteria for diagnosis of overt DIC do not have a lower sensitivity or higher specificity than KSTH criteria for DIC diagnosis. And while ISTH diagnostic criteria for overt DIC are useful for the diagnosis of typical DIC, they are not sufficient for the diagnosis of most early stage preDIC cases. Especially in cases of sepsis, diagnosis of early nonovert DIC is very important for a good outcome.10,11
Further, additional studies on universally applicable molecular markers such as D-dimer,11 antithrombin, protein C, soluble fibrin monomer,12 thrombin-antithrombin complex,13,14 tissue factor, and tissue factor pathway inhibitor15 are needed.
Our findings suggest that to achieve a good agreement between the ISTH and KSTH diagnostic systems for overt DIC, the plasma fibrinogen cut-off value in the ISTH criteria should be changed from 100mg/dL to 150mg/dL and a level below 100mg/dL should be scored as 2 points.
Figures and Tables
References
1. Taylor FB, Toh CH, Hoots WK, Wada H, Levi M. Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis(ISTH). Toward definition, clinical and laboratory criteria and scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001. 86:1327–1330.

2. Song KS, Kim BS, Yoon HS. Diagnostic efficacy of plasma D-dimer assay in evaluating disseminated intravascular coagulation: Comparison with serum FDP assay based on ROC method. Korean J Hematol. 1992. 27:75–80.
3. Korean Society of Hematology. Disseminated intravascular coagulation in Korea: An analysis of clinical and laboratory findings. Korean J Hematol. 1989. 24:259–273.
4. Jang SH, Dong ES, Koo HH, Han HS, Shin HY, Ahn HS. A clinical study of disseminated intravascular coagulation for pediatric patients. Korean J Hematol. 1990. 25:485–495.
5. Kwon CI, Kim HT, Chong SY, Oh DY, Ryu JH, Song KS. Disseminated intravascular coagulation in Korean adult population: The predisposing disease and mortality. Korean J Thromb Hemost. 2000. 7:11–15.
6. Mant MJ, King EG. Severe, acute disseminated intravascular coagulation. A reappraisal of its pathophysiology, clinical significance and therapy based on 47 patients. Am J Med. 1979. 67:557–563.
7. Siegal T, Seligsohn U, Aghai E, Modan M. Clinical and laboratory aspects of disseminated intravascular coagulation (DIC): a study of 118 cases. Thromb Haemost. 1978. 39:122–134.

8. Wada H, Gabazza EC, Asakura H, Koike K, Okamoto K, Maruyama I, Shiku H, et al. Comparison of diagnostic criteria for disseminated intravascular coagulation (DIC): Diagnostic criteria of the International Society of Thrombosis and Hemostasis and of the Japanese Ministry of Health and Welfare for overt DIC. Am J Hematol. 2003. 74:17–22.

9. Han KC, Kim SH, Lee SJ, Kim DH, Ko EH, Jang MJ, et al. Comparision between diagnostic criteria for disseminated intravascular coagulation (DIC) of the International Society on Thrombosis and Hemostasis (ISTH) and the Korean Society on Thrombosis and Hemostasis (KSTH). Korean J Hematol. 2004. 39:223–227.
10. Song JW, Choi JR, Song KS, Rhee JH. Plasma factor XIII activity in patients with disseminated intravascular coagulation. Yonsei Med J. 2006. 47:196–200.

11. Beal AL, Cerra FB. Multiple organ failure syndrome in the 1990s. Systemic inflammatory response and organ dysfunction. JAMA. 1994. 271:226–233.

12. Bredbacka S, Blombäck M, Wiman B. Soluble fibrin: a predictor for the development and outcome of multiple organ failure. Am J Hematol. 1994. 46:289–294.

13. Teitel JM, Bauer KA, Lau HK, Rosenberg RD. Studies of the prothrombin activation pathway utilizing radioimmunoassays for the F2/F1+2 fragment and thrombin-antithrombin complex. Blood. 1982. 59:1086–1097.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download