INTRODUCTION
By virtue of the improved medical and public health care system, the elderly population is expanding in our society. The socioeconomic environment, characterized by improving economic status, easy accessibility to hospital care, and increasing concern about one's own health, encourages people to detect their own health problems sooner and to obtain appropriate management in proper time. It is expected that the mean life span of Korean society will increase to approximately 80 years by 2020, which is in contrast to the life span observed in the early 1970s (less than 60 years).1
Pancreatic ductal adenocarcinoma has the highest incidence between the ages of 60 and 70 years.2 Removal of the entire tumor with oncologic R0 resection may offer the only chance for a potential cure for pancreatic cancer. Pancreaticoduodenectomy (PD) is well established as the traditional procedure for treating pancreatic head cancer, but many surgeons are hesitant to attempt radical surgery for the advanced pancreatic cancer, especially in elderly patients, not only because of the high rate of relevant morbidity and mortality, but also the nihilistic opinion of pancreatic cancer. As the elderly population has been increasing in the last several decades, the proportion of patients older than 70 years of age with resectable pancreatic cancer is expected to increase in our society.3,4
The purpose of the present study is to evaluate the safety of PD in patients older than 70 years and to assess the survival benefit of such a "demanding procedure" in elderly patients based on our institutional experiences.
MATERIALS AND METHODS
This was a retrospective study of patients older than 70 years of age who could undergo PD of ductal adenocarcinoma in the head of the pancreas. Available medical records for all patients who underwent resection of a pancreatic ductal adenocarcinoma at Yonsei Medical Center (an academic tertiary referral medical center), in Seoul, Korea, were retrospectively reviewed from January 1990 to June 2005. The study population was divided into two groups according to patients' age. "Group Y" (Young) patients were younger than 70 years and "Group O" (Old) patients were 70 years or older. Perioperative mortality defined as 30-day or in-hospital death, and perioperative morbidity which occurred during hospitalization were evaluated. The delayed gastric emptying was defined as the inability to consume a regular diet by day 10 postoperatively as well as the need for nasogastric drainage tube on or beyond 10 postoperatively.16 All gastrojejunal anastomosis or duodenojejunal anastomosis were performed in pre-colic fashion and erythromycin was not given for management of delayed gastric emptying. Demographic characteristics, past medical history, intraoperative data, pathologic data, and surgical outcomes were collected. The data including survival outcomes were compared between the two groups. Results were expressed as the mean (SD) and frequency (%). Univariate comparisons were carried out using the Fisher test and chi-square test for discrete variables and Student's t-test for continuous variables. The survival data was compared using the Kaplan-Meier method. A two-tailed p value less than 0.05 was considered statistically significant.
RESULTS
General aspects of PD for pancreatic head cancer
PD was performed in seventy-seven cases for treating ductal adenocarcinoma in the head of pancreas head at the Yonsei Medical Center between January 1990 and June 2005. Among them, 11 patients (14.3%) were 70 years or older (Group O) and the other 66 patients (85.7%) were less than 70 years old (Group Y). Over the 15-year period, total number of PD performed for pancreatic head cancer increased, however, proportion of the elder patients (≥ 70 years old) seems relatively steady (Fig. 1).
Demographics of the elderly patients
The elderly population consisted of 5 women and 6 men, with a mean (SD) age of 73.4 (± 2.4) years. Diabetes was the most frequent co-morbidity. Four patients (36.4%) had diabetes at the time of operation and 1 case each of hypertension, pulmonary disease and hypothyroidism was observed. Most patients (8 out of 11, 72.7%) required preoperative biliary decompression, such as percutaneous transhepatic biliary drainage (PTBD), endoscopic nasobiliary drainage (ENBD), and endoscopic retrograde biliary drainage (ENBD).
Pathology of pancreatic head cancer of the elderly patients
All elderly patients had pT3 ductal adenocarcinoma in the pancreas head. The mean (SD) tumor diameter was 2.7 (± 0.9)cm. The American Joint Committee on Cancer (AJCC) staging distribution in elderly patients was 7 stage IIA patients (63.6%), and 4 stage IIB patients (36.4%). Lymphovascular invasion was observed in 2 patients and perineural invasion was noted in 3 patients. Three patients (27.3%) had resection margins that were contaminated by malignant cell (R1 resection). Two cases of retroperitoneal margin and 1 case of pancreatic resection margin were shown to have microscopic pancreatic cancer.
Surgical outcomes
All patients underwent PDs for pancreatic head cancer. Conventional PD was performed in 4 patients (36.4%) and pylorus preserving pancreaticoduodenectomy (PPPD) in 7 patients (63.6%). The mean operative time was 360.5 (± 84.1) minutes and mean blood loss was 687.5 (± 448.6) ml. Six patients (54.5%) needed a perioperative transfusion and the mean transfusion requirement was 1.3 (± 1.2) units. While no patients experienced any surgery related mortality, 8 patients (72.7%) had morbidity related to PD. Delayed gastric emptying (DGE) was the most common morbidity (3 out of 8 patients, 37.5%) (Table 1). The overall hospital stay was recorded as 49.2 (± 13.8) days, and patients were discharged at 28.5 (± 16.5) days postoperatively. The median survival was 27.4 months postoperatively.
Comparative analysis between Group Y and Group O
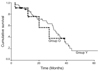
No significant differences were observed between the two groups, except in age (p < 0.001), length of total hospital stay (p = 0.012), preoperative hospital stay (p = 0.024), frequency of postoperative complication (p = 0.049), and delayed gastric emptying (p = 0.035). The duration of postoperative hospital stay had no significant differences between the two groups (p = 0.066) (Table 2). Mean follow up period was 24.5 month. PDs for pancreatic head cancer in the elderly patients did not cause any negative effects on patients' survival as compared to those performed in young patients with pT3 pancreatic head cancer (p = 0.7808, Fig. 2).
DISCUSSION
Elderly people older than 65 years have accounted for 7.2% of the overall Korean population since 2000, indicating that Korea has recently become an "aging" society. By the year 2018, it is predicted the majority of Korean society will be "aged". The progress in medical and public health intervention, such as the introduction of new medications and therapeutic techniques as well as cancer screening programs, have resulted in an increased life expectancy. According to the data released by the Korea National Statistical Office,1 the average life span has increased by more than 5 years over the last 10 years from 71.7 years of age in 1991 to 77.0 years in 2002, with the average life span expected to increase up to 81.0 years by 2020. Despite the average life span increasing and the death rate decreasing in elderly people, malignant neoplasm is still the most common cause of mortality in elderly people. Based on 2004 statistics,1 pancreatic carcinoma is the 7th most common cause of cancer-related death in Korea behind lung cancer, hepatoma, stomach cancer, colon cancer, prostate cancer and uterine cancer.
Pancreatic ductal adenocarcinoma has the highest incidence between the age of 60 and 70 years1,2,5 and has an extremely rapid, aggressive growth behavior with unfavorable prognosis. Only complete surgical removal can provide potential curability for pancreatic cancer and PD is a well-established procedure of choice for malignancy located in the pancreas head.6 Pancreatic resection in large volume centers has been shown to result in long-term survival and satisfactory quality of the remainder of life.7,8 However, morbidity and mortality cannot be ignored when PD is considered.
Because the elderly population has increased during the last several decades, the proportion of older people with resectable pancreatic malignancy has increased.4,9 This creates new challenges not only for surgeons but also for the patients and their family members. According to our results, the number of the elderly patients older than 70 years of age requiring PD for pancreatic ductal adenocarcinoma together with total number of PD were steadily increased over the past 15 years, however, the proportion of the elderly is relatively steady (Fig. 1).
A major concern regarding PD on elderly patients is that they could be extremely vulnerable to surgical stress, possibly compounded by underlying medical diseases at the time of surgery which could adversely affect the postoperative recovery. Our data showed the most frequent medical problem in elderly patients to be diabetes, which accounted for 36.4% among the 11 patients. However, other literature dealing with the results of PD in elderly patients suggested that cardiovascular diseases, such as hypertension, coronary artery disease, and pulmonary disease are risky conditions for major operations.9-12
Though we have limited experiences with PD for pancreatic adenocarcinoma in elderly patients, this major surgical procedure does not appear to cause discernable adverse effects on early and late post-surgical outcomes According to our results, postoperative morbidity and length of hospital stay were statistically different between elderly patients and younger patients less than 70 years of age. However, all complications were successfully managed in a conservative way without surgery-related death. Postoperative overall morbidity in the elderly has been reported to range from 14% to 69% 5.12-14 In particular, Riediger et al.15 claimed that patients over 65 years of age were significantly associated with DGE, regardless of pylorus-preserving procedures. In our studies, 72.7% of patients experienced postoperative complications, DGE being the most frequent (3 out of 11 patients, 27.3%). In addition to significant differences in the occurrence of postoperative morbidity between group Y and group O (p = 0.049, Table 2), the elderly patients had more DGE after PD, 3 out of 66 in group Y (4.5%) vs. 3 out of 11 in group O (27.3%), (p = 0.035, Fisher's Exact test). In conclusion, these frequent postoperative complications might be related to a prolonged duration of hospital stay. Our data showed no statistical difference in the postoperative hospital stay between the two groups (p = 0.066). However, the statistic power is apparently marginal. Brooks et al.16 reported that patients' age was an independent factor influencing the length of hospital stay. Their study, however, may contain selection bias because almost 50% of patients underwent operations before 1992 with more frequent postoperative complications as compared with their more recent postoperative outcomes. However, increased surgical experience and advances in perioperative care associated with better patient selection resulted in comparable postoperative surgical outcomes in elderly patients. One of the recent studies by Scurtu et al.10 showed no significant difference in the overall hospital stay between the two groups of patients. In our study, a statistically significant difference in overall hospital stay was mainly influenced by the duration of the preoperative period (13.5 ± 9.3 days vs. 20.9 ± 10.9 days, student t-test, p = 0.024). This indicates that careful preoperative evaluation and a detailed preparation were required for PD in the elderly.
Pancreatic fistula is the most threatening complication after PD. However, in the present study, only four patients in the group Y experienced pancreatic fistula (5.2%). This favorable result might be resulted from the consistency of the remaining pancreas. Almost patients had pT3 pancreatic cancer with its size about 2.7cm in diameter result in hard remnant pancreas with pancreatic duct dilatation. Not only experienced surgical skill but also this favorable environment of remnant pancreas attributed to the low incidence of pancreatic fistula in our study. Furthermore, current survival analysis suggests that age is not a limiting factor for PD regarding survival outcomes once macroscopically curative resection of the pancreatic head cancer was performed in elderly patients (Fig. 2). The recently reported median overall survival of elderly patients after PD for cancer ranged from 18 to 20 months.9,10,17 In the present study, the median survival of 27.4 months after PD in elderly patients with pancreatic ductal adenocarcinoma was similar to recent reports and is an improvement over the 8.9 months observed in patients treated by radiochemotherapy alone.18
The expanding elderly population in our society should not be ignored, and we need to prepare for any demand of health problems that the increasing elderly population could possibly create. This social phenomenon is expected to bring new demands and specific clinical situations of more frequent resectable pancreatic ductal adenocarcinoma in very elderly patients, which would place surgeons, medical doctors, and family members of the elderly patients in a dilemma concerning the most appropriate treatment approach. This dilemma may originate from the poor survival results of pancreatic cancer, as well as the high risk of morbidity and mortality related to PDs. Additionally, we cannot know exactly the remaining life span in each elderly patient. Though several other studies5,9,10,12,19,20 strongly suggest that age should not be considered as a contraindication for PDs, the potential benefits and disadvantages of PD in elderly patients from the viewpoint of the average remaining life span, co-morbidity and their general condition should be considered.
The number of patients older than 70 years old in present study is so limited that it seems to be difficult to reach definitive conclusions. We need to be careful when interpreting our results because our observation of PD in the elderly is basically retrospective nature. Especially, current study does not include patients with cardiovascular disease, such as CAD or CHF which recently has been shown to increase morbidity after pancreatic surgery. Therefore, there is high probability of selection bias in our study. However, our results provide surgical outcomes of pancreaticoduodenectomy in the elderly with pancreatic head cancer in our institution and suggest this surgical procedure for treatment of pancreatic head cancer in elderly patients can be an appropriate, and offers no adverse effects on survival after surgery as long as the surgery is performed safely and the patients are well selected. We need more experiences of pancreaticoduodenectomy in the elderly and well controlled study in future.
In order to facing upcoming challenge of the elderly in the near future, careful preoperative evaluations, proper patient selection, advanced surgical experiences, and perioperative management are mandatory to ensure the safety of PDs performed in even the very elderly (> 80 years) with pancreatic ductal adenocarcinoma.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download