Abstract
Purpose
The aim of this study was to investigate the pathologic characteristics of nodular gastritis in children and young adults infected with Helicobacter pylori (H. pylori).
Materials and Methods
A total of 328 patients were enrolled in this study, and the diagnosis of H. pylori infection was done with gastroduodenal endoscopy concomitant with a CLO™ test and pathologic analysis of the biopsy specimens. Diagnoses of normal, superficial gastritis, nodular gastritis, and peptic ulcer disease were made from the gastroduodenal endoscopic findings. The density of H. pylori organisms in the gastric mucosa was rated as normal, mild, moderate, or marked. The pathologic findings of nodular gastritis were based on the histopathologic findings of inflammation, immune activity, glandular atrophy and intestinal metaplasia. Each of these findings was scored as either normal (0), mild (1), moderate (2), or marked (3) according to the updated Sydney system and using visual analog scales. The gastritis score was the sum of the four histopathologic scores.
Results
In this study, nodular gastritis (50.6%) was most common, and mild density (51.5%) H. pylori infection was also common upon microscopic examination. Intestinal metaplasia occurred in 9 patients (2.7%).
Conclusion
Logistic regression revealed a significant increase in the incidence of nodular gastritis with gastritis score (p = 0.008), but not an association with sex, age, or H. pylori density. Gastritis score was the only significant factor influencing the occurrence of nodular gastritis. Intestinal metaplasia, which was originally thought to be a pre-malignant lesion, occurred in 2.7% of the patients with H. pylori infection.
Helicobacter pylori (H. pylori) is the most common cause of chronic gastritis and peptic ulcer disease, and is associated with gastric cancer and mucosa associated lymphoid tissue lymphoma (MALToma).1 About 30-100% of children with nodular gastritis,2-5 90% of duodenal ulcer,2,3,6,7 and about 25% of gastric ulcers2,6,8,9 had H. pylori infections. In contrast to adult patients, histopathologic findings of H. pylori infection in children show little neutrophil infiltration, more monocytes and lymphoid follicles microscopically, and more nodular gastritis endoscopically.3,4,10,11 Chronic active gastritis can be diagnosed with histopathologic examination in H. pylori infected children who exhibited normal findings upon endoscopic examination.12,13 We examined the factors influencing the development of nodular gastritis in association with H. pylori infection in children with recurrent abdominal pain. H. pylori infection commonly progresses from active gastritis to atrophic gastritis, intestinal metaplasia, gastric dysplasia, and finally to gastric cancer.14 We further performed a histopathologic study to determine the degree of inflammation and H. pylori density.
All children and young adults who visited Yonsei University, Severance Hospital with the chief complaint of recurrent abdominal pain from January 1993 to March 2004 underwent endo-scopic examination, a CLO™ test, and histopathologic examination of biopsy specimens. Of these patients, a total of 328 had H. pylori infection. Exclusion criteria for our study included contraindication for endoscopy, use of antibiotics, bismuth, H2 blockers, proton pump inhibitors within 30 days of the procedure, and use of anti-inflammatory drugs or acetyl salicylic acid (ASA) within 3 days of the procedure.
An EG-2530 (Pentax Inc., Tokyo, Japan) was used for upper gastrointestinal endoscopy, and the diagnosis of endoscopic nodular gastritis was made when the mucosa had an appearance of a cobblestone pavement. Two biopsy samples each were collected from the gastric antrum and body for use in the CLO™ test and histopathologic examination. When the CLO™ test showed red-violet color within 24 hours at room temperature, or H. pylori was found on histopathologic examination in biopsy specimens, the diagnosis of H. pylori infection was made. The possible endoscopic diagnoses included normal, superficial gastritis, nodular gastritis, and peptic ulcer disease.
T.W. Noh examined the biopsies (stained with hematoxylin and eosin, and Giemsa) for H. pylori and gastritis. He was kept blind to the patients' endoscopic or clinical findings throughout the examination. The histologic findings were used to classify the H. pylori density as normal, mild, moderate, or marked without scoring, according to the updated Sydney system.5 The degree of inflammation was divided into ① monocyte infiltration, ② neutrophil infiltration, ③ glandular atrophy, or ④ intestinal metaplasia, and scored as normal (0), mild (1), moderate (2), or marked (3) using the visual analogue scale applied to microscopic examination results. The sum of the scores obtained from each patient was used as the gastritis score.15 We did not differentiate between children, young adults, and adults in assessing intestinal metaplasia. We only divided the groups according to pathologic findings and the type of intestinal metaplasia. Statistical analysis was performed to determine the occurrence of nodular gastritis in association with sex, age, H. pylori density, and gastritis score.
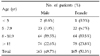
Of 328 cases of H. pylori infection, there were 163 males and 165 females with the male-female ratio of 1:1.1, spanning a range of ages from 2.3 to 19.9 years (average, 10.3 ± 8.2 years). Three cases were under the age of 5, 45 cases were between 5-7 years old, 128 cases between 8-10 years old, and 152 cases over 11 years old (Table 1).
Of 328 patients with H. pylori, 267 cases (81.4%) showed abnormal endoscopic findings, of which 72 cases (22.0%) were superficial gastritis, 166 cases (50.6%) were nodular gastritis, and 29 cases (8.8%) had peptic ulcer disease (Table 2).
H. pylori density on histologic examination was normal in 126 (38.4%) of the 382 infected patients, mild in 169 cases (51.5%), moderate in 33 cases (10.1%), and none had a marked degree of H. pylori density; the most common degree was mild (Table 3). Nodular gastritis was the most common endoscopic finding in cases of mild degree H. pylori density (Fig. 1).
Based on the updated Sydney system, the histopathologic findings were divided into monocyte infiltration, neutrophil infiltration, glandular atrophy, and intestinal metaplasia. In the case of monocyte infiltration, the ages ranged from 2.3 to 19.9 years old, and 120 cases (36.6%) were normal, 142 cases were (43.3%) mild, 66 cases (20.1%) moderate, and none were marked. For neutrophil infiltration, the ages ranged from 2.3 to 19.9 years old, 83 cases (25.3%) were normal, 152 cases (46.3%) were mild, 92 cases (28.0%) were moderate, and 1 case (0.3%) was marked. For glandular atrophy, the patients were 2.3 to 18.8 years old, and 136 cases (41.5%) were normal, 181 cases (55.2%) mild, 11 cases (3.4%) moderate and none in marked degree. For intestinal metaplasia, the patients were 7.7 to 15 years old, and 319 cases (97.3%) were normal, 7 cases (2.1%) were mild, 1 case (0.3%) was moderate, and 1 case (0.3%) showed marked results, for a total of 9 cases (2.7%) showing intestinal metaplasia (Table 3).
The gastritis scores ranged from 0 to 8. Patients with scores of 3, 4, and 5 were 21.6%, 22.6% and 11.3%, respectively, which totalled 55.5% of all patients (Fig. 2). The gastritis score of patients with nodular gastritis was significantly higher than those with superficial gastritis or peptic ulcer disease (p < 0.001), and nodular gastritis was most common in patients with gastritis scores of 3, 4, or 5 (Fig. 3). Notably, in 9 cases with intestinal metaplasia, 2 cases had a score of 8, 1 had a score of 7, 1 had a score of 5, 4 had a score of 4, and 1 had a score of 2. Histopathologic severity was more profound in patients with intestinal metaplasia than those without.
The combined effects were assessed using a logistic regression model to obtain adjusted odds ratio in the association of sex, age, H. pylori density, and gastritis score with nodular gastritis. Mutual adjustments in the variables showed that sex, age, and H. pylori density were independently associated with the occurrence of nodular gastritis. Increased gastritis scores were significantly associated with nodular gastritis (Table 4).
In 1983, the spiral-shaped gram-negative bacterium Helicobacter pylori (H. pylori) was isolated and identified in gastric biopsy specimens of gastritis patients by Warren and Marshall.16 H. pylori is the major cause of peptic ulcer disease, including chronic active inflammatory reactions of stomach and gastric cancer (adenoma and lymphoma).17 It has been proven that most idiopathic gastritis is caused by H. pylori,18 prompting reclassification of gastritis. The classification of chronic gastritis is based on Schindler's classification from 1947.19 To date, there had been no uniform guidelines regarding the diagnosis of gastritis, methods for describing visual findings, or precise terminology. Therefore a revised gastritis classification, "the Sydney system",20 was announced at the 9th World Congress in Gastroenterology held in Australia in 1990. The Sydney system for the classification of gastritis emphasized the importance of combining topographical, morphological, and etiological information into a scheme that would assure reproducible and clinically useful diagnoses. To reappraise the Sydney system 4 years after its introduction, a group of pathologists from various parts of the world met in Houston, Texas, in September 1994, and revised the Sydney system to establish a common terminology for gastritis and to identify, define, and attempt to resolve some of the problems. Overall, the general principles and grading as originally proposed in the Sydney system were retained, but grading was improved by the provision of a visual analogue scale.5 In this study, the diagnosis of gastritis was based on the updated Sydney system, and the visual analogue scale was used to classify the histopathologic findings.
About 30-100% of children with nodular gastritis,2-5 90% with duodenal ulcer,2,3,6,7 and 25% with gastric ulcer disease2,6,8,9 are known to be infected with H. pylori. The rate of H. pylori infection is intimately connected to a country's socioeconomic level, race, and age, and is higher in developing countries than in developed countries. As the economic state worsens, the rate of infection rises, and as age increases, the frequency of infection also increases.21,22 Bahu et al.15 reported that in children with H. pylori infection, the frequency of nodular gastritis and the density of H. pylori increase as they age. Gastritis diagnoses were based on histopathologic findings of monocyte infiltration, neutrophil infiltration, glandular atrophy, and intestinal metaplasia using the visual analogue scale, and these findings were scored as normal (0), mild (1), moderate (2), or marked (3). The final gastritis score is the sum of the four histopathologic scores. They assessed the combined effects using logistic regression to obtain adjusted odds ratios for the association of age, H. pylori density, and gastritis score with nodular gastritis. As a result, mutual adjustments of variables showed that increased age and H. pylori density were independently associated with the occurrence of nodular gastritis. Increases in the gastritis score was dependent on increased H. pylori density and significantly associated with occurrence of nodular gastritis. Rafeey et al.23 reported that the frequency of endoscopic nodular gastritis was related to increasing age (p < 0.0001), presence of H. pylori, a grade of histologic gastritis, and H. pylori density (p < 0.0001). In this study, of a total 328 patients, nodular gastritis was most common in 166 cases (50.6%), and the H. pylori density was statistically higher in nodular gastritis than in superficial gastritis or peptic ulcer disease (p < 0.001). There were no statistically significant correlations between sex, age, and H. pylori density with the occurrence of nodular gastritis. Increased gastritis scores were only significantly associated with the occurrence of nodular gastritis.
Kamada et al.24 studied the endoscopic and histologic findings in young patients with H. pylori infection by using biopsy specimens of gastric antrum from 112 Japanese patients under 29 years of age. They reported that in monocyte infiltration, 6 cases (5.4%) were mild, 52 cases (46.4%) were moderate, and 54 cases (48.2%) were classified as marked, and all cases showed monocyte infiltration. For neutrophil infiltration, 13 cases (11.6%) were mild, 76 cases (67.9%) were moderate, and 23 cases (20.5%) were marked, with all cases showing neutrophil infiltration. For glandular atrophy, 81 cases (72.3%) were normal, 29 cases (25.9%) were mild, 2 cases (1.8%) were moderate, and none were marked. A total 31 cases (27.7%) presented with glandular atrophy. In cases of intestinal metaplasia, 106 cases (94.6%) had no metaplasia, while 6 cases (5.4%) had mild metaplasia. Kato et al.25 examined whether H. pylori infection and mucosal inflammation resulted in gastric atrophy based on histopathologic findings of gastric biopsy specimens obtained from 131 cases of H. pylori infected Japanese children ranging in age from 1 to 16 years old. Monocyte infiltration was found in 59.5% of the children, most of which were moderate, while neutrophil infiltration was seen in 84.0%, most of which were mild . Glandular atrophy was seen in 51.9% of the cases, most of which were mild. Intestinal metaplasia was found in 4.6% of the cases. In this study, we found that for monocyte infiltration, 120 cases (36.6%) were normal, 142 cases (43.3%) were mild, 66 cases (20.1%) were moderate, and none had any marked degree of infiltration. Patients aged from 2.3 to 19.9 years with mild and moderate monocyte infiltration (63.4%) had lower frequencies and degrees of monocyte infiltration than those of Japanese patients. For neutrophil infiltration, 83 cases (25.3%) were normal, 152 cases (46.3%) were mild, 92 cases (28.0%) were moderate, and 1 case (0.3%) showed a marked degree of infiltration. Our patients (ranging in aged from 2.3 to 19.9 years old) with neutrophil infiltration (74.7%) had lower frequencies and degrees of neutrophil infiltration than those of Japanese. In glandular atrophy, 136 cases (41.5%) were normal, 181 cases (55.2%) were mild degree, 11 cases (3.4%) were moderate, and none showed any marked degree of atrophy. Our patients (agedranging in age from 2.3 to 18.8 years old) with mild and moderate glandular atrophy (58.5%) had similar or higher frequency and degree of glandular atrophy than those of Japanese. In the case of intestinal metaplasia, 319 cases (97.3%) were normal, 7 cases (2.1%) were mild, 1 case (0.3%) was moderate, and another 1 case (0.3%) exhibited a marked degree of metaplasia. Patients aged from 7.7 to 15 years in this study showed intestinal metaplasia (2.7%) at about half the frequency as those in the Japanese (4.6-5.4%) study.23,24 The inflammatory degree of gastritis caused by H. pylori in Korean patients is thought to be not as severe as that in Japanese.
As noted, in Korean patients, the histopathologic lesions of gastritis start as early as the age of 2.3, and these lesions progress to intestinal metaplasia after the age of 7.7, which means gastritis might occur from a young age and progress to intestinal metaplasia in some patients as they grow older.
In conclusion, the present study demonstrated that the more the gastritis scores increase, the higher the rate at which nodular gastritis occurs. Most of the patients infected with H. pylori at an earlier age have no specific symptoms or complications, but some patients progress to conditions including active gastritis, atrophic gastritis, and intestinal metaplasia. Therefore, the early diagnosis and treatment of H. pylori infection with nodular gastritis is a prudent investment.
Figures and Tables
Fig. 1
Endoscopic diagnoses and H. pylori density. Nodular gastritis is most common with mild H. pylori density (p < 0.001). (SG, superficial gastritis; NG, nodular gastritis; PU, peptic ulcer disease.)

Fig. 2
Distribution of patients infected with H. pylori and their gastritis scores. About 55.5% of patients had a gastritis score of 3, 4 or 5.

Fig. 3
Endoscopic diagnoses and gastritis scores. Nodular gastritis is the most common finding in patients with gastritis scores of 3, 4 or 5. (SG, superficial gastritis; NG, nodular gastritis; PU, peptic ulcer disease.)

References
1. Sherman P, Czinn S, Drumm B, Gottrand F, Kawakami E, Madrazo A, et al. Helicobacter pylori infection in children and adolescents: Working Group Report of the First World Congress of Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2002. 35:Suppl 2. S128–S133.
2. Macarthur C, Saunders N, Feldman W. Helicobacter pylori, gastroduodenal disease, and recurrent abdominal pain in children. JAMA. 1995. 273:729–734.
3. Queiroz DM, Rocha GA, Mendes EN, Carvalho AS, Barbosa AJ, Oliveira CA, et al. Differences in distribution and severity of Helicobacter pylori gastritis in children and adults with duodenal ulcer disease. J Pediatr Gastroenterol Nutr. 1991. 12:178–181.
4. Hassall E, Dimmick JE. Unique features of Helicobacter pylori disease in children. Dig Dis Sci. 1991. 36:417–423.
5. Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol. 1996. 20:1161–1181.
6. De Giacomo C, Fiocca R, Villani L, Lisato L, Licardi G, Diegoli N, et al. Helicobacter pylori infection and chronic gastritis: clinical, serological, and histologic correlations in children treated with amoxicillin and colloidal bismuth subcitrate. J Pediatr Gastroenterol Nutr. 1990. 11:310–316.
7. Bujanover Y, Konikoff F, Baratz M. Nodular gastritis and Helicobacter pylori. J Pediatr Gastroenterol Nutr. 1990. 11:41–44.
8. Bujanover Y, Rief S, Yahav J. Helicobacter pylori and peptic disease in the pediatric patient. Pediatr Clin North Am. 1996. 43:213–234.
9. Sbeih F, Abdullah A, Sullivan S, Merenkov Z. Antral nodularity, gastric lymphoid hyperplasia and Helicobacter pylori in adults. J Clin Gastroenterol. 1996. 22:227–230.
10. Robert ME, Weinstein WM. Helicobacter pylori associated gastric pathology. Gastroenterol Clin North Am. 1993. 22:59–72.
11. Zaitoun AM. Histological study of chronic gastritis from the United Arab Emirates using the Sydney system of classification. J Clin Pathol. 1994. 47:810–815.
12. Belair PA, Metz DC, Faigel DO, Furth EE. Receiver operator characteristic analysis of endoscopy as a test for gastritis. Dig Dis Sci. 1997. 42:2227–2233.
13. Genta RM, Hammer HW. The significance of lymphoid follicles in the interpretation of gastric biopsy specimens. Arch Pathol Lab Med. 1994. 118:740–743.
14. Blaser MJ. Helicobacter pylori and the pathogenesis of gastroduodenal inflammation. J Infect Dis. 1990. 161:626–633.
15. Bahu Mda G, da Silveira TR, Maguilnick I, Ulbrich-Kulczynski J. Endoscopic nodular gastritis: an endoscopic indicator of high-grade bacterial colonization and severe gastritis in children with Helicobacter pylori. J Pediatr Gastroenterol Nutr. 2003. 36:217–222.
16. Marshall BJ, Warren JR. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984. 1:1311–1315.
17. Moss S, Calam J. Helicobacter pylori and peptic ulcer: the present position. Gut. 1992. 33:289–292.
18. Misiewicz JJ. The Sydney System: a new classification of gastritis. Introduction. J Gastroenterol Hepatol. 1991. 6:207–208.
19. Schindler R. Gastritis. 1947. New York: Grune & Stratton.
20. Price AB. The Sydney system: histological division. J Gastroenterol Hepatol. 1991. 6:209–222.
21. Choi WJ, Kim JW, Chung KS. Therapeutic outcome and recurrence rate of Helicobacter pylori infection in children. Korean J Pediatr Gastroenterol Nutr. 1998. 1:37–44.
22. Choi IK, Lee SY, Chung KS. Effect of one or two week triple therapy with omeprazole, amoxicillin, and clarithromycin on eradication of Helicobacter pylori infection in children. Korean J Pediatr Gastroenterol Nutr. 2002. 1:19–25.
23. Rafeey M, Jafari Rouhi AH, Gassemi BA, Rouhi AJ. Relationship between endoscopic nodular gastritis and Helicobacter pylori infection in children. Indian J Gastroenterol. 2004. 23:138–139.
24. Kamada T, Sugiu K, Hata J, Kusunoki H, Hamada H, Kido S, et al. Evaluation of endoscopic and histological findings in Helicobacter pylori-positive Japanese young adults. J Gastroenterol Hepatol. 2006. 21:258–261.
25. Kato S, Nakajima S, Nishino Y, Ozawa K, Minoura T, Konno M, et al. Association between gastric atrophy and Helicobacter pylori infection in Japanese children: a retrospective multicenter study. Dig Dis Sci. 2006. 51:99–104.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download