Abstract
Purpose
To investigate whether serum amyloid A (SAA) levels are increased in patients with ankylosing spondylitis (AS) and whether its levels correlate well with AS disease activity.
Materials and Methods
Thirty-eight patients with AS and 38 age- and sex-matched control subjects were enrolled in this cross-sectional study. Their SAA levels were quantitatively measured by immunonephelometry. An established, self-administered instrument for evaluating disease activity (Bath Ankylosing Spondylitis Disease Activity Index, BASDAI) was used to measure and acute phase reactants, including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), in patients with AS.
Results
Patients with AS had a significantly higher mean SAA level than controls (9.52 ± 7.49 mg/L versus 2.73 ± 1.57 mg/L, p < 0.05), and the mean BASDAI score of patients with elevated SAA levels was significantly higher than that of patients with normal SAA levels (5.6 ± 1.3 versus 4.4 ± 1.5, p < 0.05). SAA levels showed significant correlations with BASDAI scores (r = 0.431, p = 0.007), ESR (r = 0.521, p = 0.001) and CRP levels (r = 0.648, p < 0.001). Additionally, the correlation between ESR and CRP levels also appeared significant (r = 0.703, p < 0.001). In those with normal ESR or CRP levels, SAA levels and BASDAI scores were elevated (p < 0.05) and showed a trend of positive correlation with one another.
Biological markers of inflammation have long been used for the diagnosis and monitoring of various diseases such as infection, tissue damage, neoplasm and inflammatory rheumatic disease. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), both major acute phase reactants, are well-known indicators of disease activity. Measurement of their levels are clinically helpful for evaluating the disease status in patients with various rheumatic diseases, but their role is sometimes limited because of their lack of specificity.
Serum amyloid A (SAA), a kind of apolipoprotein, is one of the acute phase proteins and is primarily synthesized in the liver by activated monocytes and macrophages.1 Previous studies have shown that in vivo concentrations of SAA can be dramatically increased (up to 1000-fold) in plasma during acute inflammatory conditions, and its increase is as greatly amplified as CRP level.2,3 This dramatic induction of SAA in response to pro-inflammatory stimuli is due largely to the synergistic effects of cytokine signaling pathways, primarily those of the interleukin (IL)-1, IL-6 and tumor necrosis factor (TNF)-α.4,5 Several studies about the relationship between the SAA level and disease activity have been reported repeatedly, and in some rheumatic diseases such as rheumatoid arthritis (RA), polymyalgia rheumatica (PMR) and sarcoidosis, the value of SAA is estimated as being a highly useful indicator of disease activity and therapeutic monitoring.6-9
In ankylosing spondylitis (AS), clinical assessment of disease activity and response to treatment is complex and difficult. Although the two traditional markers of acute phase response, ESR and CRP, have been used for assessment, they may not often correlate with the patient's symptoms or radiologic progression. Thus, it is important to find more sensitive and specific surrogate markers that can more accurately reflect disease activity.
Therefore, in order to evaluate the usefulness of SAA as an indicator of disease activity, we determined the levels of SAA in patients with AS and investigated whether its levels correlated with AS disease activity.
This cross-sectional study was conducted involving 38 patients (26 men and 12 women; mean age, 29.6 ± 10.7 years) who fulfilled the modified New York criteria for the classification of AS.10 Thirty-eight age- and sex-matched healthy control subjects (25 men and 13 women; mean age, 30.1 ± 8.7 years) were also enrolled. All patients were seen at Yonsei University Medical Center, Seoul, Korea, from December 2002 to June 2003. We excluded patients who had a medical or surgical illness such as recent infection, trauma and/or a neoplastic disease, in order to remove other confounding factors affecting SAA level.
We measured the validated clinical criteria from the AS assessment working group for disease activity, Bath Ankylosing Spondylitis Disease Activity Index (BASDAI),11 which is a reliable, self-administered instrument focusing on fatigue, axial pain, peripheral pain, enthesopathy and morning stiffness in all patients with AS. At the time of clinical measurements, blood samples were obtained from both patients with AS and the controls. Samples were immediately centrifuged and stored at -70℃ until analysis. SAA levels were quantitatively measured by immunonephelometry using an N-Latex SAA reagent (Dade Behring Inc., Marburg, Germany) and the Equil Nephelometer-Analyzer (Behring Co., Behring, Germany) according to the manufacturer's protocol. Precision testing of SAA was performed using the National Committee on Clinical Laboratory Standards (NCCLS) EP15-P protocol guideline.12 The within run and total precision coefficients of variation were 3.4% and 3.5%, respectively, and the reference range for SAA levels was defined as less than 6.4 mg/L. Serum ESR was measured using the modified Westergren method (reference range < 15mm/hr in men and < 20mm/hr in women), and CRP levels were measured by immunonephelometry (BN-II nephelometer; Dade-Behring, Marburg, Germany, reference range < 0.8 mg/dL) in the patients with AS.
All statistical analyses were performed using the SPSS software package (for Windows, Version 11.5, SPSS Inc, Chicago, IL, USA). All data are shown as mean ± standard deviation, and biochemical data represent duplicate measurements. The results were analyzed using the independent t-test and chi-square tests as appropriate, and correlations were evaluated using Pearson's correlation test. A p-value less than 0.05 was considered statistically significant.
The baseline characteristics of the study subjects are summarized in Table 1. Mean age and men-to-women ratio did not differ between patients with AS and the controls. All patients with AS had sacroiliitis proven by radiograph. Peripheral arthritis, Achilles' tendonitis, uveitis, inflammatory bowel disease, and renal amyloidosis were found in 27 (71.1%), 14 (36.8%), 9 (23.7%), 1 (2.6%) and 1 (2.6%) patients with AS, respectively. Thirty-seven (97.4%) patients with AS were on non-steroidal anti-inflammatory drugs (NSAIDs), and 14 (36.8%) patients were on NSAIDs and sulfasalazine. The one remaining patient was on corticosteroids for renal amyloidosis.
All control subjects had normal SAA levels, and their mean SAA level was 2.73 ± 1.57 mg/L. Patients with AS had increased SAA levels, with a mean value of 9.52 ± 7.49 mg/L. Patients with AS had significantly higher mean SAA levels than controls (p < 0.05) (Fig. 1).
In patients with AS, SAA levels showed significant correlations with BASDAI scores (r = 0.431, p = 0.007, Fig. 2A), ESR (r = 0.521, p = 0.001, Fig. 2B) and CRP levels (r = 0.648, p < 0.001, Fig. 2C). Additionally, the correlation between ESR and CRP levels also appeared to be significant (r = 0.703, p < 0.001, Fig. 2D). However, the presence of peripheral arthritis, Achilles' tendonitis and uveitis were not significantly associated with SAA levels, and differences in medications did not affect SAA levels, either.
Twenty of 38 patients (52.6%) had increased SAA levels, but the remaining 18 patients (47.4%) had normal SAA levels. The mean BASDAI score of those with normal SAA levels was 4.4 ± 1.5, and the mean score of those with increased SAA levels was 5.6 ± 1.3. The mean BASDAI score of patients with increased SAA levels was significantly higher than that of patients with normal SAA levels (p < 0.05). Particularly, of the 20 patients with increased SAA levels, 16 (80%) patients had a normal ESR, and nine (45%) had normal CRP levels. All patients who had normal CRP levels also had a normal ESR. Mean BASDAI scores of those with a normal ESR and CRP levels were 5.39 and 4.78, respectively, which indicate non-negligible inflammatory burdens. The mean SAA levels in these patients were 13.7 ± 6.2 mg/L and 10.9 ± 5.2 mg/L, respectively. Although statistical significance was not found, SAA levels showed a trend of positive correlation with BASDAI scores in these patients (Fig. 3A and B).
AS is one of the chronic inflammatory rheumatic diseases that primarily involves the axial skeleton and peripheral joints. Besides skeletal involvement, disabling extra-articular manifestations, including inflammatory bowel disease, uveitis and amyloidosis, can occur.10,13 For the past several decades, the management of this disease has been largely restricted to the use of NSAIDs and so-called disease-modifying drugs.14-16 However, recent trials of biologic agents like anti-TNF therapy have demonstrated effectiveness in relieving symptoms and controlling disease activity.16-18 In addition, the effect of these agents on extra-articular manifestations and radiographic progression has now been investigated intensely.19,20 Thus, appropriate monitoring of disease activity in order to guide the therapeutic modalities is crucial to reduce or prevent further complications and disease progression. However, the surrogate markers most appropriate for this purpose are lacking in AS, and the discrepancy between patient's symptoms and laboratory markers is often encountered in clinical practice.11,21 This study was based on the fact mentioned above, and the supposition that SAA, a sort of acute phase protein, can be considered as a useful activity marker in AS. We evaluated SAA production in the serum of patients with AS as compared to controls, and investigated the relationship between SAA and previously established disease activity indicators. As a result, we found that SAA levels of patients with AS were significantly higher than in the control patients and showed significant positive correlations with both clinical and laboratory parameters reflecting the inflammatory burden of AS. These findings indicate a usefulness of SAA measurement for monitoring disease activity. In particular, significant elevations of both SAA levels and BASDAI scores were noted in those with normal ESR and CRP levels, and SAA levels and BASDAI scores showed a trend of positive correlation with one another in these patients. These findings may suggest that SAA can be used as a more sensitive laboratory marker than ESR or CRP for monitoring disease activity of AS. To confirm the superiority of SAA to other acute phase reactants, further investigations involving a large number of subjects would be needed.
According to previous studies regarding the clinical markers in RA, SAA is massively produced through the signaling pathways of pro-inflammatory cytokines such as IL-1β, IL-6 and TNF-α, and its level is more sensitive than CRP.6,21-23 Other reports on PMR suggested that serum SAA is more predominant than ESR or CRP with regard to sensitivity and specificity, respectively, and its level can reflect the disease activity effectively.8,24,25 But, in AS, SAA has not been studied as extensively as in RA or PMR, and we could find only a few studies investigating the association between SAA and disease activity of AS.21,26,27 One of these studies reported that SAA levels in patients with AS correlated well with BASDAI scores, and that ESR and CRP levels seem to be a good indicator of disease activity.21 Our results were also similar to those previously reported, but we tried to identify the superiority of SAA to ESR or CRP in determining the extent of AS disease activity. Some research concerning the acute phase proteins revealed that both SAA and CRP are produced in the liver, but serum levels of the former depend on a larger number of pro-inflammatory cytokines than the latter.8,28-30 Consequently, we can guess that there is a possible difference between SAA and CRP in reflecting disease activity, and this phenomenon originated not only from the facilities of synthesis by their own structural properties, but also the types and amounts of cytokines participate in the production.
It has been reported that SAA has an influence on the pathogenesis of several diseases such as inflammatory arthritis, infection, neoplasia, atherosclerosis (by means of both pro- and anti-inflammatory activities, and by changing the cholesterol metabolism and transport).31-33 Moreover, SAA can cause secondary amyloidosis, derived from deposits of amyloid fibrils and plaques in specific organs.33 The precise mechanisms involved in amyloid formation and deposition are poorly understood, but amyloidogenic factors like incomplete proteolysis of SAA or both initiation and growth of amyloid fibrils by macrophage have been proposed.33,34 Even though the role of SAA in amyloidogenesis still remains unclear, it is certain that high concentrations and long exposure of SAA in serum are the most important pathogenic factors.21,33 In the present study, one of patients with AS had renal amyloidosis confirmed by renal biopsy. Although this patient had much higher SAA levels than that of controls, interestingly, the level did not differ from the mean SAA level of other patients with AS. The reason for this observation is not clear, but it is well established that glucocorticoids participate in the control of an inflammatory response by providing negative feedback on the production of various cytokines, such as IL-1, IL-6 and TNF-α, which are important inducers of SAA production35,36 Our patient with amyloidosis was on glucocorticoids, and thus, there is a possibility that the suppression of inflammatory cytokines with glucocorticoids might also suppress the synthesis of SAA.
In conclusion, we found a significant elevation of SAA levels in patients with AS as compared to controls, and a strong positive correlation between SAA level and AS disease activity. We also determined SAA to be a more sensitive laboratory marker than ESR or CRP. Therefore, we suggest that SAA can be used as a valuable indicator of disease activity in AS.
Figures and Tables
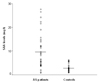 | Fig. 1Comparison of SAA levels between patients with AS and controls. The mean SAA level of patients with AS was significantly higher than that of controls (9.52 ± 7.49 mg/L versus 2.73 ± 1.57 mg/L, p < 0.05). The horizontal bar represents the mean SAA value of each group. |
 | Fig. 2Correlation of SAA levels with BASDAI scores, ESR and CRP levels, and the correlation between ESR and CRP levels in patients with AS. (A) SAA levels correlated well with BASDAI scores (r = 0.431, p = 0.007). (B) SAA levels correlated well with ESR (r = 0.521, p = 0.001). (C) SAA levels correlated well with CRP levels (r = 0.648, p < 0.001). (D) ESR correlated well with CRP levels (r = 0.703, p < 0.001). |
 | Fig. 3Correlation of SAA levels with BASDAI scores in patients with a normal ESR and CRP levels. A. SAA levels showed a trend of positive correlation with BASDAI scores in patients with a normal ESR (r = 0.460, p = 0.073). B. SAA levels showed a trend of positive correlation with BASDAI scores in patients with normal CRP levels (r = 0.486, p = 0.185). |
References
1. Uhlar CM, Whitehead AS. Serum amyloid A, the major vertebrate acute-phase reactant. Eur J Biochem. 1999. 265:501–523.
2. Hoffman JS, Benditt EP. Changes in high density lipoprotein content following endotoxin administration in the mouse. Formation of serum amyloid protein-rich subfractions. J Biol Chem. 1982. 257:10510–10517.
3. Marhaug G. Three assays for the characterization and quantitation of human serum amyloid A. Scand J Immunol. 1983. 18:329–338.
4. Dowton SB, Peters CN, Jestus JJ. Regulation of serum amyloid A gene expression in Syrian hamsters by cytokines. Inflammation. 1991. 15:391–397.
5. Strissel KJ, Girard MT, West-Mays JA, Rinehart WB, Cook JR, Brinckerhoff CE, et al. Role of serum amyloid A as an intermediate in the IL-1 and PMA-stimulated signaling pathways regulating expression of rabbit fibroblast collagenase. Exp Cell Res. 1997. 237:275–287.
6. O'Hara R, Murphy EP, Whitehead AS, FitzGerald O, Bresnihan B. Acute-phase serum amyloid A production by rheumatoid arthritis synovial tissue. Arthritis Res. 2000. 2:142–144.
7. Vallon R, Freuler F, Desta-Tsedu N, Robeva A, Dawson J, Wenner P, et al. Serum amyloid A (apoSAA) expression is up-regulated in rheumatoid arthritis and induces transcription of matrix metalloproteinases. J Immunol. 2001. 166:2801–2807.
8. Shimojima Y, Matsuda M, Gono T, Ishii W, Ikeda S. Serum amyloid A as a potent therapeutic marker in a refractory patient with polymyalgia rheumatica. Intern Med. 2005. 44:1009–1012.
9. Salazar A, Pinto X, Mana J. Serum amyloid A and high-density lipoprotein cholesterol: serum markers of inflammation in sarcoidosis and other systemic disorders. Eur J Clin Invest. 2001. 31:1070–1077.
10. van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984. 27:361–368.
11. Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol. 1994. 21:2286–2291.
12. National Committee for Clinical Laboratory Standards. User demonstration of performance for precision and accuracy; proposed guideline EP15-P. 1998. Wayne, PA: NCCLS.
13. Lance NJ, Curran JJ. Amyloidosis in a case of ankylosing spondylitis with a review of the literature. J Rheumatol. 1991. 18:100–103.
14. van der Linden S, van der Heijde D. Clinical aspects, outcome assessment, and management of ankylosing spondylitis and postenteric reactive arthritis. Curr Opin Rheumatol. 2000. 12:263–268.
15. Kirwan J, Edwards A, Huitfeldt B, Thompson P, Currey H. The course of established ankylosing spondylitis and the effects of sulphasalazine over 3 years. Br J Rheumatol. 1993. 32:729–733.
16. Scalapino KJ, Davis JC Jr. The treatment of ankylosing spondylitis. Clin Exp Med. 2003. 2:159–165.
17. Braun J, Brandt J, Listing J, Zink A, Alten R, Golder W, et al. Treatment of active ankylosing spondylitis with infliximab: a randomised controlled multicentre trial. Lancet. 2002. 359:1187–1193.
18. Rosenbaum JT. Effect of etanercept on iritis in patients with ankylosing spondylitis. Arthritis Rheum. 2004. 50:3736–3737.
19. Ortiz-Santamaria V, Valls-Roc M, Sanmarti M, Olive A. Anti-TNF treatment in secondary amyloidosis. Rheumatology. 2003. 42:1425–1426.
20. Baraliakos X, Listing J, Rudwaleit M, Brandt J, Sieper J, Braun J. Radiographic progression in patients with ankylosing spondylitis after two years of treatment with the tumour necrosis factor-α antibody infliximab. Ann Rheum Dis. 2005. 64:1462–1466.
21. Lange U, Boss B, Teichmann J, Klor HU, Neeck G. Serum amyloid A- an indicator of inflammation in ankylosing spondylitis. Rheumatol Int. 2000. 19:119–122.
22. Cunnane G, Grehan S, Geoghegan S, McCormack C, Shields D, Whitehead AS, et al. Serum amyloid A in the assessment of early inflammatory arthritis. J Rheumatol. 2000. 27:58–63.
23. Marhaug G, Dowton SB. Serum amyloid A: an acute phase apolipoprotein and precursor of AA amyloid. Baillieres Clin Rheumatol. 1994. 8:553–573.
24. Hachulla E, Saile R, Parra HJ, Hatron PY, Gosset D, Fruchart JC, et al. Serum amyloid A concentrations in giant-cell arteritis and polymyalgia rheumatica: a useful test in the management of the disease. Clin Exp Rheumatol. 1991. 9:157–163.
25. Yamane T, Yamauchi H, Abe N, Torio N, Shimada R, Senba T, et al. Serum amyloid A as a useful index of disease activity in polymyalgia rheumatica. Ryumachi. 2003. 43:544–548.
26. Vinje O, Moller P, Mellbye J. Immunological variables and acute-phase reactants in patients with ankylosing spondylitis (Bechterew's syndrome) and their relatives. Clin Rheumatol. 1984. 3:501–513.
27. Ostensen M, Marhaug G, Husby G. Amyloid-related serum protein (SAA) during and after pregnancy in healthy women and women with rheumatic disease. Acta Pathol Microbiol Immunol Scand[c]. 1985. 93:1–5.
28. Hagihara K, Nishikawa T, Isobe T, Song J, Sugamata Y, Yoshizaki K. IL-6 plays a critical role in the synergistic induction of human serum amyloid A (SAA) gene when stimulated with proinflammatory cytokines as analyzed with an SAA isoform real-time quantitative RT-PCR assay system. Biochem Biophys Res Commun. 2004. 314:363–369.
29. Thorn CF, Lu ZY, Whitehead AS. Regulation of the human acute phase serum amyloid A genes by tumor necrosis factor-alpha, interleukin-6 and glucocorticoids in hepatic and epithelial cell lines. Scand J Immunol. 2004. 59:152–158.
30. Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999. 340:448–454.
31. Malle E, Steinmetz A, Raynes JG. Serum amyloid A (SAA): an acute phase protein and apolipoprotein. Atherosclerosis. 1993. 102:131–146.
32. Kisilevsky R, Tam SP. Acute phase serum amyloid A, cholesterol metabolism, and cardiovascular disease. Pediatr Pathol Mol Med. 2002. 21:291–305.
33. Cunnane G. Amyloid precursors and amyloidosis in inflammatory arthritis. Curr Opin Rheumatol. 2001. 13:67–73.
34. Kluve-Beckerman B, Liepnieks JJ, Wang L, Benson MD. A cell culture system for the study of amyloid pathogenesis. Amyloid formation by peritoneal macrophages cultured with recombinant serum amyloid A. Am J Pathol. 1999. 155:123–133.
35. Ray A, Zhang DH, Siegel MD, Ray P. Regulation of interleukin-6 gene expression by steroids. Ann N Y Acad Sci. 1995. 762:79–87.
36. Knudsen PJ, Dinarello CA, Strom TB. Glucocorticoids inhibit transcriptional and post-transcriptional expression of interleukin 1 in U937 cells. J Immunol. 1987. 139:4129–4134.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download