Abstract
A 44-year-old woman underwent surgery for an asymptomatic primary tumor of the heart located in the right atrium. The tumor was detected incidentally during follow-up computed tomography for a resected breast cancer. The mass, lying along the lower portion of the right atrial septum, was homogenous and cystic in nature, as detected by transthoracic and transesophageal echocardiography. Complete resection was performed via a median sternotomy under cardiopulmonary bypass. The postoperative course was uneventful. However, the histological result was surprising: the mass was a cardiac lymphangioma.
Primary cardiac tumors are rare, their incidence ranging from 0.0017% to 0.33% at autopsy.1 Benign tumors account for 75% of all primary cardiac tumors, of which 75% are myxomas. Among adults, the most frequently encountered nonmyxomatous benign tumors are lipomas and fibromas.1 Cystic lymphangioma, which is usually confined to the head and neck, is a well-recognized tumor that occurs during childhood.2 However, a cardiac lymphangioma is exceptionally uncommon and a particularly rare form of cardiac disease.1 Here, we report a case of cystic lymphangioma developing from the lower limbus of the fossa ovalis, presenting as a cystic mass in the right atrium.
A 44 year-old female with a history of breast cancer, which was removed by modified radical mastectomy three years previously, was referred to us by her surgeon for evaluation of a mass in the right atrium (RA) that was discovered incidentally during follow-up computed tomography (CT). On enhanced CT imaging, a slightly enhancing homogenous round low-density mass was observed in the RA (Fig. 1). The patient had remained asymptomatic following her breast cancer resection, specifically denying dyspnea, lightheadedness, syncope, or lower extremity edema.
On examination, the patient appeared well nourished and in no acute distress. Vital signs included a blood pressure of 118/78 mmHg and heart rate of 75 beats per minute. Baseline biochemical and hematological tests were within normal limits. A chest X-ray revealed a normal-sized heart and no evidence of metastatic nodules in the lung fields. On auscultation, there was a regular rate and rhythm without murmur and clear breath sounds in both lung fields. The patient had normal peripheral pulses and no peripheral edema.
Transthoracic echocardiography (TTE) revealed a cystic tumor in the RA with homogenous echogenicity, adjacent to the interatrial septum but not obstructing the right ventricular inflow. The mass was difficult to visualize by TTE because of its low echogenicity and its thin fibrous capsule. There was no pericardial effusion or epicardial mass suspected as metastasis from the breast cancer. Transesophageal echocardiography (TEE) demonstrated a mobile mass in the RA with homogenous low echogenicity that measured 28 × 29 mm. A bicaval view at a 119° angle of rotation revealed that the mass did not develop from the mid portion of the fossa ovalis and that it nearly filled the lower portion of the RA cavity in this image plane (Fig. 2A). We advanced the TEE probe and rotated the angle to 87° to obtain a longitudinal image plane that included the orifice of the inferior vena cava (IVC) and the lower interatrial septum. The mass protruded into the RA and was attached to the interatrial septum near the orifice of the IVC (Fig. 3). Contrast echocardiography using an intravenous injection of agitated saline provided a clearer delineation and spatial resolution of the mass, revealing a lobulated surface (Fig. 2B and Fig. 3).
A right atriotomy was performed under total cardiopulmonary bypass. The right atrial mass was found to arise from the lower limbus of the fossa ovalis, and it had a well-developed capsule. Successful resection of the mass resulted in a 1 cm sized defect of the interatrial septum, which was closed with a pericardial patch. The remainder of the operative course was uneventful.
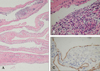
Histopathologically, the lesion was cystic and contained transparent fluid. The cyst was lined with a single layer of endothelial cells with fibrous septa and lymphoid infiltrates (Fig. 4A and 4B). Immunohistochemically, the endothelial cells demonstrated a positive reaction for CD34 (Fig. 4C). The final diagnosis was a cardiac lymphangioma.
Cardiac lymphangioma is a very rare tumor of the heart, first reported in 1911 by Armstrong and Monckeberg.3 Only nine cases of cardiac lymphangioma have been reported in the medical literature.3-11 More than half of the reported cases have occurred in patients under 10 years of age.3,4,6,8,9,11 Mediastinal lymphangiomas are most often asymptomatic masses incidentally discovered on chest X-ray. However, cardiac lymphangiomas are commonly revealed during congestive heart failure, syncopal or embolic pathology, arrhythmias, palpitations, or cardiac tamponade.3,4,7,9,10,12
Common malignancies, such as breast or lung cancer, account for the greatest percentage of nonprimary cardiac tumors. Metastatic disease involvement is frequently located in the pericardium, resulting in pericardial effusion and epicardial involvement.13 However, in the current case there was no pericardial effusion nor any epicardial mass suspected to be metastasis from the previous breast cancer. The well-defined and encapsulated nature of the mass suggested that it was benign rather than malignant. The most common diagnosis for a primary cardiac tumor in adults is a myxoma. In 15 - 20% of cases, myxomas are located in the right atrium, usually around the fossa ovalis,14 with a nonhomogeneous texture, and lucent centers or areas of calcification upon echocardiogram. Our case did not share these features. Echocardiography and CT suggested a well-defined space-occupying lesion adjacent to the orifice of the IVC, possibly a cystic tumor of the atrioventricular (AV) node15,16 and cardiac varix.17,18
Cystic tumors of the AV node (sometimes called "benign mesotheliomas of the AV node") are rare lesions associated with complete heart block, ventricular tachycardia or fibrillation, which can cause sudden death. Accordingly, diagnosis is usually confirmed post-mortem. These tumors originate in the AV nodal region and have a broad connection with the interatrial septum and no stalk.15,16 Histologically, the cystic walls are composed of fibrous connective tissue covered by a layer of squamous or cuboidal epithelium. The current case had features that were inconsistent with this entity. Specifically, this mass had a narrow stalk, originated from the lower limbus of the fossa ovalis, not from the AV nodal region, and its cystic wall was covered by endothelium rather than epithelium.
Cardiac varices are endocardial, unilocular blood filled cysts lined by endothelial cells and filled with phleboliths. As in the current case, they are situated in the lower part of the interatrial septum. However, in the present case the cystic mass was not filled with blood or phleboliths, but rather with transparent fluid. Histopathologically, there were lymphoid infiltrates beneath a layer of endothelial cells. Therefore, the current case is not consistent with a cardiac varix but instead is best described as a cardiac lymphangioma.
On gross pathological examination, cardiac lymphangiomas may be either soft and spongy or firm and fibrous. The size of these tumors varies, and the largest one reported was 9 cm in diameter. The tumors most commonly occur in the pericardial space,19 but other unusual primary sites include the myocardium, the posterior wall of the left atrium, and the AV node regions.4,10,11 The primary site of the cardiac lymphangioma in the present case (lower part of the interatrial septum) differs from all prior reports of this tumor. In general, lymphangiomas are considered to be malformations that arise from sequestration of lymphatic tissue that fails to communicate normally with the rest of the lymphatic system. Although the head, neck and axilla are sites that account for one half to three fourths of all lymphangiomas, these masses may affect almost any part of the body,20,21 including the heart, as in the current case.
Surgery is indicated both to confirm the diagnosis and to avoid the risk of a lethal arrhythmia. Four of the nine patients previously were reported to have cardiac lymphangioma presented with arrhythmias or palpitations.3-5,7 Two of these four patients experienced cardiac arrest caused by heart blockage,3,4 and another one died during cardiac catheterization.7 Moreover, cystic lymphangiomas have a potential risk of recurrence, especially if there has been incomplete resection.22 Therefore, we believe that complete resection is essential.
The unique features of this case of cardiac lymphangioma were its cystic nature and its attachment to the interatrial septum near the lower margin of the fossa ovalis in the right atrium. This finding broadens the spectrum of potential presentation of cardiac lymphangioma. After two years of follow-up, the patient has been symptom-free and has shown no evidence of recurrence or arrhythmia.
Figures and Tables
Fig. 1
Enhanced computed tomography imaging showing a slightly enhancing homogenous round mass with low density in the right atrium.

Fig. 2
Transesophageal images from a bicaval view of the right atrium at 119°. (A) An encapsulated cystic mass (arrow heads) is noted in the lower portion of the right atrium but the boundary of the mass is not well-defined. (B) Contrast enhances the right atrium revealing a lobular mass that is not arising from the mid portion of the fossa ovalis. LA, left atrium; RA, right atrium; SVC, superior vena cava.

Fig. 3
Magnified transesophageal echocardiographic image, in the longitudinal plane at 87°. A cystic mass protrudes into the right atrium, and is attached to the atrial septum near the orifice of the inferior vena cava. Contrast with intravenous injection of agitated saline provided a clearer delineation of the mass. IVC, inferior vena cava; M, mass; RA, right atrium.

Fig. 4
Photomicrographs. (A) Collapsed and infolded cyst wall (H&E, × 40). (B) Higher power view of cyst wall structure, showing loose connective tissue stroma lined by flat endothelial cells beneath which is seen a lymphocytic infiltration (H&E, × 400). (C) The endothelial cells show a positive immunostaining for CD 34-related antigen.
References
1. Burke A, Virmani R. Tumors of the heart and great vessels: Atlas of tumor pathology series 3. 1996. vol 16. Washington, DC: Armed Forces Institute of Pathology;1–11.
2. Glasson MJ, Taylor SF. Cervical, cervicomediastinal and intrathoracic lymphangioma. Prog Pediatr Surg. 1991. 27:62–83.
3. Armstrong H, Monckeberg JG. Herzblock bedingt durch primaren Hertztumor, bei einem funf Jahrigen Kinde. Deutsch Arch Klin Med. 1911. 102:144–166.
4. Fontaliran F, Guillois B, Colin A, Blanc JJ, Chabaud JJ, Boog G, et al. Congenital atrioventricular block and maternal lupus erythematosus. Histologic discovery of tumor of the atrioventricular node. Arch Mal Coeur Vaiss. 1989. 82:609–613.
5. Nataf P, Mestiri T, Martin de Lasalle E, Benomar M, Gandjbakhch I, Cabrol C. Pericardial hemolymphangioma. Apropos of a case. Arch Mal Coeur Vaiss. 1988. 81:1137–1140.
6. Lymburner RM. Tumours of the heart: histopathological and clinical study. Can Med Assoc J. 1934. 30:368–373.
7. Anbe DT, Fine G. Cardiac lymphangioma and lipoma. Report of a case of simultaneous occurrence in association with lipomatous infiltration of the myocardium and cardiac arrhythmia. Am Heart J. 1973. 86:227–235.
8. Pasaoğlu I, Doğan R, Ozme S, Kale G, Bozer AY. Cardiac lymphangioma. Am Heart J. 1991. 121:1821–1824.
9. Daubeney PE, Ogilvie BC, Moore IE, Webber SA. Intrapericardial lymphangioma presenting as neonatal cardiac tamponade. Pediatr Cardiol. 1996. 17:129–131.
10. Jougon J, Laborde MN, Parrens M, MacBride T. Cystic lymphangioma of the heart mimicking a mediastinal tumor. Eur J Cardiothorac Surg. 2002. 22:476–478.
11. Kaji T, Takamatsu H, Noguchi H, Tahara H, Matsuda H, Nomura Y, et al. Cardiac lymphangioma: case report and review of the literature. J Pediatr Surg. 2002. 37:E32.
12. Miralles A, Bracamonte L, Soncul H, Diaz del Castillo R, Akhtar R, Bors V, et al. Cardiac tumors: clinical experience and surgical results in 74 patients. Ann Thorac Surg. 1991. 52:886–895.
13. Feigenbaum H, Armstrong WF, Ryan T. Masses, tumors, and source of embolus. Feigenbaum's echocardiography. 2005. 6th ed. Philadelphia: Lippincott Willians & Wilkins;708–710.
14. Burke AP, Virmani R. Cardiac myxoma. A clinicopathologic study. Am J Clin Pathol. 1993. 100:671–680.
15. Paniagua JR, Sadaba JR, Davidson LA, Munsch CM. Cystic tumour of the atrioventricular nodal region: report of a case successfully treated with surgery. Heart. 2000. 83:E6.
16. Saito S, Kobayashi J, Tagusari O, Bando K, Niwaya K, Nakajima H, et al. Successful excision of a cystic tumor of the atrioventricular nodal region. Circ J. 2005. 69:1293–1294.
17. Harrity PJ, Tazelaar HD, Edwards WD, Orszulak TA, Freeman WK. Intracardiac varices of the right atrium: a case report and review of the literature. Int J Cardiol. 1995. 48:177–181.
18. Remadi JP, BenAmar A, Baron O. Varix of the heart. Ann Thorac Surg. 2001. 72:264–265.
19. Burke A, Virmani R. Tumors of the heart and great vessels: Atlas of tumor pathology series 3. 1996. vol 16. Washington, DC: Armed Forces Institute of Pathology;87–88.
20. Ozdemir H, Kocakoc E, Bozgeyik Z, Cobanoglu B. Recurrent retroperitoneal cystic lymphangioma. Yonsei Med J. 2005. 46:715–718.
21. Cho BC, Kang SM, Lee SC, Moon JG, Lee DH, Lim SH. Primary idiopathic chylopericardium associated with cervicomediastinal cystic hygroma. Yonsei Med J. 2005. 46:439–444.
22. Icard P, Le Rochais JP, Galateau F, Jehan A, Martel B, Brun J, et al. Cystic lymphangioma of the mediastinum. Apropos of 3 cases, review of the literature. Ann Chir. 1998. 52:629–634.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download