Abstract
We present our surgical experiences with functioning neuroendocrine neoplasms of the pancreas to define its natural history, and to suggest its proper management. From June 1990 to June 2005, patients with diagnosis of functioning neuroendocrine (islet cell) neoplasms of the pancreas were retrospectively reviewed. Fourteen patients (5 men and 9 women) with a median age of 49 years (range, 12 - 68 years) were identified. Twelve patients (86%) had insulinoma, two (14%) had gastrinoma. One (7%) with pancreatic insulinoma was multiple endocrine neoplasia type 1. Intraoperative ultrasound scan (sensitivity, 83%) was the most powerful modality for tumor localization. Fifteen neoplasms with median tumor size 1 cm (range 0-3 cm) were resected. Four insulinomas (26.7%) were located in the head of the pancreas and 5 (36%), in the tail. Another 5 (36%) insulinomas and 1 (7%) gastrinoma were located around the neck area near the SMV or PV. Eleven patients (79%) underwent enucleation, and 2 patients (14%), distal pancreatectomy with splenectomy. 100% of patients with functioning neuroendocrine neoplasms of the pancreas have survived. The overall disease free 10-year survival was found to be about 81%. Exact localization of tumor by intraoperative ultrasound and surgical removal are promising for good prognosis.
An islet cell neoplasm of the pancreas is a rare pathologic condition. An annual incidence of 5 to 10 patients per million is reported.1 This pathologic entity can be divided into "nonfunctioning" and "functioning" neuroendocrine neoplasms of the pancreas according to the tumor's ability to produce pancreatic neuroendocrine hormones, such as, gastrin, insulin, glucagon, somatostatin, and vasoactive intestinal peptide (VIP). This can result in clinical or laboratory serum evidence of neuroendocrine hormone hypersecretion.
Patients with a functioning neuroendocrine neoplasm of the pancreas have characteristic symptoms caused by tumor specific pancreatic neuroendocrine hormones. However, the rarity of these pathologic conditions makes it difficult to recognize even a functioning neuroendocrine neoplasm of the pancreas,2,3 as a result, can lead to delayed in definitive treatment.
The purpose of this study is to review our surgical experiences with functioning neuroendocrine neoplasms of the pancreas. This study focuses on insulinoma, including its clinical presentation, operative management, and perioperative outcomes of patients who underwent surgery for functioning neuroendocrine tumors of the pancreas.
A retrospective review of the medical records of patients with a functioning neuroendocrine neoplasm of the pancreas was performed in Yonsei University Medical Center (academic tertiary care referral center), Seoul, Korea. From June 1990 to June 2005, the medical records of all patients with a functioning neuroendocrine tumor of the pancreas were retrospectively reviewed to identify patients' characteristics, clinical presentation, radiographic localization, operative methods, operative morbidity, tumor characteristics, and prognosis. The diagnosis of a functioning neuroendocrine tumor of the pancreas was based on clinical and histopathologic characteristics. A characteristic clinical syndrome of excessive neuroendocrine hormone, as well as histologic and immunohistochemical confirmation of a pancreatic islet-cell neoplasm, were needed for definitive diagnosis. Perioperative serum levels of neuroendocrine hormones were recorded. Statistics were applied as appropriate to the data. All times were reported in months and survival time was calculated from the date of treatment to a specified end point, for example, death or date of last follow-up. Follow-up was obtained through medical records, telephone contact and personal data provided by official records and was complete as of August 30, 2005.
Fourteen patients who had diagnosis of functioning NENs of pancreas and underwent surgery were identified. There were 5 men and 9 women with a median age of 49 years (range 12-68). Twelve out of 14 (86%) patients had insulinoma, and the other two patients (14%) had gastrinoma. One patient (7%) with pancreatic insulinoma had MEN 1.
All patients presented with signs and symptoms of specific hormonal excess (Table 1). All 12 patients with insulinoma presented with Whipples's triad. They showed clinical symptoms and signs of hypoglycemia, median blood glucose less than 40 mg/dL, and relief of symptoms with glucose administration. Both two cases of gastrinoma presented with peptic ulcer disease for which they had already undergone peptic ulcer surgery, such as antrectomy and gastrojejunostomy with truncal vagotomy, more than 10 years ago. Endoscopic gastroduodenoscopy revealed multiple jejunal ulcerative lesions. However, they did not present with typical diarrhea caused by excessive gastric secretion which is normally stopped by applying nasogastric drainage. Median period from initiation of symptoms to the definitive treatment was 9 months (range 0.5 - 240 month).
The most powerful radiological modality for tumor localization was the intraoperative ultrasound scan (sensitivity, 83%), followed by the endoscopic ultrasound scan (67%), and then the transhepatic portal venous sampling (63%) (Table 2).
Fifteen neoplasms were found among surgically resectable 13 patients. The median tumor size was 1 cm (range 0-3 cm) in diameter. Four insulinomas were located in the head of the pancreas and additional 5 (36%), in the tail. Another 5 insulinomas (36%) and 1 (7%) gastrinoma were located around the neck area near the SMV or PV (Fig. 1).
Three patients (21%) had multiple neuroendocrine tumors. Two patients with insulinoma had two discrete tumors in the head and neck, respectively. One of them was discovered during the second operation for recurred hypoglycemic symptoms after the first surgery. One patient with gastrinoma who had hepatic metastases had multiple masses in the pancreas and duodenum.
A malignant tumor was discovered in 2 patients (14%). One patient had multiple metastatic gastrinomas, and another patient had an insulinoma with local invasion on permanent pathologic report.
The enucleation of tumors was the most common procedure for the treatment of functioning neuroendocrine neoplasms of the pancreas. Eleven patients (79%) underwent enucleation, and 2 patients (14%) underwent distal pancreatectomy with splenectomy. A laparoscopic distal pancreatectomy with splenectomy was performed in one of them. One patient with multiple metastatic gastrinomas did not receive operation.
There were 2 cases (14.3%) of re-operation in functioning neuroendocrine reoperations of the pancreas. One patient underwent distal pancreatectomy with splenectomy after enucleation of the insulinoma, because the permanent pathologic section showed peripancreatic tissue invasion of the tumor, a malignant feature. The other patient underwent transection of the neck of the pancreas and wedge resection of the pancreas with Rouxen-y pancreaticojejunostomy due to a recurred functioning insulinoma after enucleation of the primary neoplasm.
Four patients (30.8%) experienced postoperative complications after surgery. They were focal pancreatitis (1), pleural effusion (1), postoperative ileus (1), and wound problem (1). All were successfully managed by conservative management.
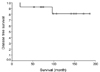
All patients of functioning neuroendocrine tumors survived except 1 patient with insulinoma. This patient died of an acute myocardial infarction which is not believed to be related to insulinoma 70 months after surgery. Therefore, statistically 100% of patients with functioning neuroendocrine neoplasms of the pancreas have survived according to survival analysis. Two patients (15.4%, 2/13 patients), among those who underwent surgery for functioning neuroendocrine neoplasms of the pancreas, developed recurrence of clinical symptoms of functioning neuroendocirne neoplasm (Table 3). Both patients had insulinoma. One patient is suspected to have MEN I, and the other patient is suffering from typical hypoglycemic symptoms, approximately 96 months after surgery. The latter case has been managed conservatively by ingesting sugar containing food early every morning. The overall disease free 10-year survival was found to be about 81% with a mean disease free survival of 164 months (95% confidence interval, 133.14-191.78 months)(Fig. 2). One patient with gastrinoma had serum gastrin levels around 800 pg/mL without evidence of tumor recurrence on image study. It is believed to be derived from a previous vagotomy and a proton pump inhibitor the patient has been taking.
Neuroendocrine neoplasms of the pancreas are uncommon. During the last 15 years, we have experienced only 14 patients with functioning neuroendocrine neoplasms of the pancreas. In 1998, Johns Hopkins reported their 47-year experience of patients with pancreatic neuroendocrine neoplasms.4 According to this paper, it was also about one patient per year for a total of 58 patients. Another report on experience with functioning neuroendocrine neoplasms of the pancreas3 shows a series of 20 surgically-treated patients with functional neuroendocrine tumors over 25 years. This explains less than one patient per year is treated in a busy academic center. The number of present patients is still small for a single center. However, experiences of 14 patients with functioning neuroendocrine neoplasms during the last 15 years are not insignificant.
This rarity of disease must be a major challenge to alert physician for their recognition and requirements of treatment Unlike our expectation that early detection of functioning neuroendocine neoplasm of the pancreas is possible due to tumor specific syndrome caused by excessive hormonal secretion, the symptom complexes of functioning pancreatic neuroendocrine neoplasm are often initially unrecognized as a result of the rarity of these tumors. According to our results, the median time taken from initial symptoms of hormonal excess to definitive treatment was 9 months (range 0.5-240 months). Even in the case of insulinomas, all patients experienced intermittent hypoglycemic symptoms. However, the symptomatic relief after having sugar containing diet or their ignorance of their symptoms caused delays in proper management, as well as delayed diagnosis. In addition, all the patients with gastrinoma underwent surgery for peptic ulcers. Patients and physicians regarded patients' symptoms of epigastric pain as being derived from previous peptic ulcer disease caused by incomplete ulcer surgery.
Preoperative tumor localization of functioning neuroendocrine neoplasms is very important. Functioning neuroendocrine neoplasms, such as insulinoma and gastrinoma, are generally small tumors with a diameter of less than 1 cm. Computed tomography (CT) or occasionally magnetic resonance imaging (MRI) are routinely performed in preoperative investigation for detecting distant metastasis, lymph node metastasis, local invasiveness, as well as tumor location. However, they have low sensitivity for detecting small functioning neuroendocrine neoplasms of the pancreas. 5 Our data shows low sensitivity for detecting tumors of US, CT, and MRI. Occasionally, tumors can be large enough to be detected in those radiological modalities, however, most functioning neuroendocrine neoplasms of the pancreas are not.
The endoscopic ultrasound scan (EUS) has appeared to be the most efficient method in recent reports. It shows nearly 90% sensitivity for visualization of insulinomas.6,7 The disadvantages of this method can be so operator dependent. In our result, 66.6% sensitivity was noted in detecting tumors preoperatively. Emergence of the intra-operative ultrasound (IOUS) has been monumentally important in the treatment of functioning neuroendocrine neoplasms. IOUS has often been considered essential for performing surgery in the treatment of neuroendocrine neoplasms of the pancreas. Our data shows more than 83% sensitivity in detecting functioning small tumors of the pancreas by IOUS. However, it is necessary that IOUS be done by experienced investigators. It can identify tumors as small as 3 mm with special sensitivity for insulinomas. In addition, patients will undergo surgery without any further localization, relying on total pancreatic exploration with palpation and IOUS investigation.8 The IOUS is especially useful for the detection of an unexpected insulinoma in patients with multiple insulinomas. The IOUS provided sufficient information of tumor location in a case of recurrence after enucleation of the insulinoma and unexpected functioning neuroendocrine neoplasm was detected.
Percutaneous transhepatic portal venous sampling and selective arterial stimulation can also be of great help in the detection of functioning neuroendocrine neoplasms of the pancreas. However, these investigative tools are technically difficult and invasive. Therefore, they are not used as frequently as in the past. If other preoperative radiological modalities provide insufficient clues for tumor localization, especially in cases of recurrence after primary surgery, these alternate techniques would be helpful.
An analysis of several reported series suggests that gastrinomas, PPomas, and somatostatinomas show a 75% preference to an anatomic location to the right of the superior mesenteric arteries in peripancreatic tissue. In contrast, about 75% of insulinomas and glucagonomas were located in the body and tail of the pancreas to the left of the superior mesenteric artery.9 Our results show that functioning neuroendocrine neoplasms of the pancreas, especially insulinomas, were not uncommonly located in the neck of the pancreas around the superior mesenteric vein (SMV, 6 out of 13 tumors, 46.2%). In addition, one case of recurred insulinoma, which was detected by IOUS, was located at the neck area, on the right side of the SMV. We would like to emphasize that surgeons should investigate the total pancreas very carefully in the operative field to detect tumor location. In particular, the neck area of the pancreas around the SMV needs to be meticulously investigated by palpation or IOUS.
In this review, most functioning neuroendocrine neoplasms of the pancreas were safely enucleated with cautious dissection. Eleven patients (79%) underwent enucleation, and two patients underwent distal pancreatectomy with splenectomy without serious postoperative complications. Recently, with the advancement of laparoscopic skill and experience, laparoscopic pancreatic resections have been attempted with compatible results.10 In this study, the laparoscopic procedure was used for one patient who underwent distal pancreatectomy. With the help of laparoscopic equipment, such as laparoscopic IOUS, laparoscopic removal of functioning neuroendocrine neoplasms of the pancreas is expected to increase. Even robotic surgery in the pancreas is available in these days.11 In robotic surgery, fine dissection with a full range of motion of working arms and excellent vision would be a strong benefit in performing enucleation of pancreatic tumors.
Our experience with gastrinoma is very limited. One patient with gastrinoma who underwent enucleation of the tumor has been followed up for more than 50 months after surgery. No image studies or endoscopic gastroduodenoscopy revealed any tumor recurrence or metastasis. However, serum gastrin level has been recorded at more than 800 pg/mL. In considering most gastrinomas are malignant and tumor size is very small, the patient needs to be followed very carefully. The patient has been taking proton pump inhibitors on a regular basis for a long time. Another patient with gastrinoma who had initial metastasis and multiple tumors has been alive for more than 15 months after diagnosis. She refused to receive further diagnostic evaluation and treatment. The patient has also been taking oral proton pump inhibitors and expresses no specific complications until the end point of this study. As with this patient, more potent antisecretory medications, such as proton pump inhibitors, have diminished the clinical lethality of gastrinomas. Therefore, total gastrectomies are infrequently performed. Gastrinomas are always malignant but have a very variable prognosis. Approximately one-fourth of gastrinomas have shown markedly slow progression. Another fourth rapidly progress. The remaining may be something in between the two groups.12 The two cases we experienced here might be of the slowly progressing type.
Pancreatic endocrine neoplasms may occur sporadically or in conjunction with the MEN I syndrome. MEN I is characterized by tumors of the parathyroid, pituitary, pancreas, and occasionally the adrenal gland. This syndrome is associated genetically with the defect of chromosome 11 and is inherited in an autosomal dominant fashion. MEN I account for about 20% of patients with gastrinomas, 4% of those with insulinomas, and lesser percentages of those with other neuroendocrine neoplasms of the pancreas.13 In our data, one patient with insulinoma (8%, 1/12 insulinomas) is suspected to have MEN I syndrome. This 28-year-old female patient initially underwent enucleation because of a functioning insulinoma. After surgery, the symptoms of insulinoma developed again. CT and MRI scans revealed multiple hypervascular tumors spread over the pancreas. Additional glucagon suppression test, C-peptide suppression test, and long starvation test proved diagnosis of an insulinoma. Serum calcium and PTH were elevated. The sestamibi scan show diffuse enlargement of bilateral parathyroid glands, and Brain CT scans revealed a 5.9 × 6.1 mm sized pituitary tumor with an elevated serum level of prolactin. However, her family members showed no evidence of any syndrome of MEN I. She has been being followed up on an out-patient basis.
We need to keep in mind that it is necessary to investigate the possibility of MEN I in the case of gastrinoma which is known as the most common functioning neuroendocrine neoplasm associated with MEN I or in case of recurred insulinoma with multiplicity. Any patients with pancreatic endocrine neoplasms should have calcium levels measured to screen for MEN I, because most (70-90%) MEN I manifest hyperparathyroidism. If calcium levels are elevated, the parathyroid and pituitary glands need to be studied. Important emphasis should be placed on the fact that most pancreatic endocrine tumors related to MEN I are multiple and have malignant potential. Gastrinomas that developed in patients with MEN I are usually malignant, as indicated by the presence of lymph node or distant metastasis. Approximately 10% of insulinomas related to MEN I are malignant.14
The neuroendocrine neoplasms of the pancreas are rare pathologic conditions, which lead to delayed diagnosis and treatment even in functioning pancreatic endocrine neoplasms. Tumor localization and proper operative management is important from a clinical standpoint. Based on our results, the pancreatic tissue around the SMV needs to be carefully investigated, especially in cases of insulinoma. Sometimes the results of preoperative tumor localization might be negative. Resection of 80-90% of the pancreas can be best management in islet cell hyperplasia of the pancreas.15 Recognition of MEN I is also important because pancreatic neuroendocrine neoplasm related to MEN I can be malignant and have multiple distributions. The prognosis of almost every patient with surgery is very good, except in two cases of recurrence. Careful follow-up is mandatory in such cases.
References
1. Delcore R, Friesen SR. Gastrointestinal neuroendocrine tumors. J Am Coll Surg. 1994. 178:187–211.
2. Azimuddin K, Chamberlain RS. The surgical management of pancreatic neuroendocrine tumors. Surg Clin North Am. 2001. 81:511–525.
3. Matthews BD, Smith TI, Kercher KW, Holder WD Jr, Heniford BT. Surgical experience with functioning pancreatic neuroendocrine tumors. Am Surg. 2002. 68:660–666.
4. Phan GQ, Yeo CJ, Hruban RH, Lillemoe KD, Pitt HA, Cameron JL. Surgical experience with pancreatic and peripancreatic neuroendocrine tumor: review of 125 patients. J Gastrointest Surg. 1998. 2:472–482.
5. Akerstrom G, Hellman P, Hessman O, Osmak L. Surgical treatment of endocrine pancreatic tumors. Neuroendocrinology. 2004. 80:Suppl 1. 62–66.
6. Anderson MA, Carpenter S, Thompson NW, Nostrant TT, Elta GH, Scheiman JM. Endoscopic ultrasound is highly accurate and directs management in patients with neuroendocrine tumors of the pancreas. Am J Gastroenterol. 2000. 95:2271–2277.
7. Thompson NW, Czako PF, Fritts LL, Bude R, Bansal R, Nostrant TT, et al. Role of endoscopic ultrasonography in the localization of insulinomas and gastrinomas. Surgery. 1994. 116:1131–1138.
8. Grant CS, van Heerden J, Charboneau JW, James EM, Reading CC. Insulinoma: the value of intraoperative ultrasonography. Arch Surg. 1998. 123:843–848.
9. Howard TJ, Stabile BE, Zinner MJ, Chang S, Bhagavan BS, Passaro E Jr. Anatomic distribution of pancreatic endocrine tumors. Am J Surg. 1990. 159:258–264.
10. Gagner M, Inabnet WB, Biertho L, Salky B. Laparoscopic pancreatectomy: a series of 22 patients. Ann Chir. 2004. 129:2–10.
11. Melvin WS, Needleman BJ, Krause KR, Eliision EC. Robotic resection of pancreatic neuroendocrine tumor. J Laparoendosc Adv Surg Tech A. 2003. 13:33–36.
12. Yu F, Venzon DJ, Serrano J, Goebel SU, Doppman JL, Gibri F, et al. Prospective study of the clinical course, prognostic factors, causes of death, and survival in patients with long-standing Zollinger-Ellison syndrome. J Clin Oncol. 1999. 17:615–630.
13. Heitz PU, Kasper M, Polak JM, Kloppel G. Pancreatic endocrine tumours. Hum Pathol. 1982. 13:263–271.
14. Lairmore TC, Moley JF. Townsend CM, Beaychamp RD, Evers BM, Matthox KL, editors. The multiple endocrine neoplasia syndromes. Sabiston textbook of surgery: The Biological Basis of Modern Surgical Practice. 2004. 17th ed. Philadelphia: Elsevier Saunders;1071–1087.
15. Kim YW, Park YK, Park JH, Lee SH, Lee J, Ko SW, et al. Iselt cell hyperplasia of the pancreas presenting as hperinsulinemic hypoglycemia in an adult. Yonsei Med J. 2000. 41:426–429.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download