Abstract
The etiology of biliary tract cancer is obscure, but there are evidences that bile acid plays a role in carcinogenesis. To find the association between biliary tract cancer and bile acid, this study compared the bile acid concentration and composition among patients with biliary cancer, biliary tract stones, and no biliary disease. Bile was compared among patients with biliary tract cancer (n = 26), biliary tract stones (n = 29), and disease free controls (n = 9). Samples were obtained by percutaneous transhepatic biliary drainage, endoscopic nasobiliary drainage, or gallbladder puncture, and analyzed for cholic, deoxycholic, chenodeoxycholic, lithocholic, and ursodeoxycholic acid composition. Total bile acid concentration was lower in the cancer group than the biliary stone and control groups; the proportions of deoxycholic (2.2% vs. 10.2% and 23.6%, p < 0.001 and p < 0.001, respectively) and lithocholic acid (0.3% vs. 0.6% and 1.0%, p = 0.065 and p < 0.001, respectively) were also lower. This result was similar when disease site was limited to bile duct or gallbladder. Analysis of cases with bilirubin ≤ 2.0 mg/dL also showed lower total bile acid concentration and deoxycholic acid composition in the cancer group compared to controls (5.7% vs. 23.6%, p = 0.003). Although the presence of bile duct obstruction explains some of the difference in total concentration and composition of bile acid, there are other contributing mechanisms. We suspect the alteration of bile acid transport might decrease bile acid excretion and cause the accumulation of carcinogenic bile acid in bile duct epithelium.
Bile duct cancer originates from the bile duct epithelium; it is divided into intrahepatic cholangiocarcinoma, extrahepatic bile duct cancer, and gallbladder cancer. Known risk factors include bile stasis, chronic inflammation, chronic hepatitis, carcinogenic exposures, choledochal cyst, liver fluke (especially in Asia), and, in Western countries, primary sclerosing cholangitis. However, in most cases, a risk factor is hard to find.1
Bile acid is a common denominator in all risk factors. Bile is composed of primary bile acids, such as cholic and chenodeocycholic acid, derived directly from cholesterol, secondary bile acids such as deoxycholic and lithocholic acid, and tertiary bile acids such as ursodeoxycholic acid. Physiologically, these acids are complexed with taurine or glycine.1 Hydrophobic acids such as deoxycholic acid are known to be associated with carcinogenesis. In contrast, hydrophilic acids such as ursodeoxycholic acid have protective effects such as prevention of gallstones through desaturation of bile and reduction of cellular changes seen in hepatic and biliary diseases.2-6 In animal models, cholic and deoxycholic acid have been implicated in the development of bile duct cancer.7,8 Increased levels of deoxycholic and lithocholic acid concentrations have also been reported in patients with choledochal cyst and anomalous union of the pancreaticobiliary duct.9 Although studies have shown that bile acid can be carcinogenic, there are few reports evaluating bile acid composition in biliary tract cancer, likely due to the rarity of this disease. Therefore, the role of bile acid in the development of biliary tract cancer remains elusive.
In this study, bile concentration and composition were compared among subjects with biliary tract cancer, biliary tract stones, and controls. In addition, subjects with gallbladder diseases and bile duct diseases were compared among them separately. Based on the difference of bile composition in patients with biliary cancer, biliary stone, and no biliary disease, we sought to elucidate the role of bile acid in the development of biliary tract cancer.
Between April 2003 and October 2004, patients with biliary tract cancer, diagnosed by tumor markers, endoscopic retrograde cholangiopancreatography (ERCP), computerized tomography (CT), or magnetic resonance image (MRI), and confirmed by clinical course, cytology, and tissue biopsy, were enrolled. Twenty-six patients with confirmed diagnosis who gave informed consent were consecutively enrolled.
For comparison, a biliary stone group, composed of patients with cholelithiasis, choledocholithiasis, or intrahepatic stone, and a control group, composed of liver transplant donors with no biliary disease, were included. Patients with chronic liver disease, including biliary cirrhosis, small bowel diseases, or diabetes mellitus, were excluded. All patients supplied informed consent, and approval was granted by the Ethical Committee for Clinical Research of the Institutional Review Board of Yonsei Medical Center, Korea.
Bile was collected post inflammation in cases who underwent percutaneous transhepatic bile drainage (PTBD) or endoscopic naso-biliary drainage (ENBD). Post inflammation was defined as the absence of fever and leukocytosis. However, since it was unethical for bile juice collection to interfere with the treatment, it was allowed to collect bile juice from patients with leukocytosis if they were under antibiotics treatment and did not have fever. Surgical cases had bile (10 cc) collected via gallbladder puncture. Samples were stored at -70℃ immediately after collection until analysis. Prior to collection, all patients had serum chemistries and complete blood cell counts.
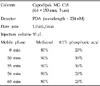
Bile acids were separated by high pressure liquid chromatography (HPLC), and analyzed using the Nanospace SI-2 HPLC system (Shiseido Co., Ltd, Tokyo, Japan) and Photodiodearray detector (Thermo Electron Co., Ltd, Waltham, MA, USA). Other HPLC conditions are summarized in Table 1.
Among bile acids, cholic acid (CA), chenodeoxycholic acid (CDCA), deoxycholic acid (DCA), lithocholic acid (LCA), and ursodeoxycholic acid (UDCA) were analyzed. Standard reagents were obtained from Sigma-Aldrich (St Louis, MO, USA). Acetonitrile was combined with both triethyamine and 2,4-dibromoacetophenone to make TEA and derivatization reagent, respectively. Standard solution of each acid was made by heating a mixture of diluted, commercially purchased acid with TEA and derivatization reagent at 80℃ for 40 minutes; each solution was then cooled at room temperature and filtered with a 0.45-µm membrane filter. To evaluate bile composition, test solution was created. NaOH (4 N, 3 mL) was added to the bile sample (1 mL), hydrolyzed at 100℃ for 3 hours, cooled at room temperature, then mixed with HCl (6 N, 3 mL) and compounded with ether (6 mL). Dried supernatant (3 mL), was then dissolved in methanol (2 mL), and eluate (1 mL) was mixed with TEA (1 mL) and derivatization reagent (1 mL) and heated by water bath at 80℃ for 40 minutes. It was then cooled at room temperature and filtered with a 0.45 µm membrane filter. The solution was analyzed by HPLC, and each bile acid concentration was measured. The proportion of each bile acid relative to the sum of total bile acid was computed.
Results were presented as means (± standard deviation) and ranges. Results of serum chemistries, total bile acid concentration, and component bile acid proportions among each study group were compared using the Mann-Whitney U test. SPSS (Windows 11.0) was used for statistical analysis; a p value less than 0.05 was considered significant.
Of 64 total patients, 26 had biliary tract cancer, 29 had biliary stone disease, and 9 were controls. The male to female ratio was 34:30; average age was 56 ± 16 years. Among the 26 patients with a biliary tract cancer, 20 had bile duct cancer and 6 had gallbladder cancer; surgery, PTBD, and ENBD was performed in 3 (11.5%), 18 (69.2%), and 5 (19.2%) cases, respectively. Fourteen out of 26 patients had cytological or histologic confirmation of cancer diagnosis. Among the 29 patients with biliary stones, surgery, PTBD, and ENBD was performed in 17 (58.6%), 5 (17.2%), and 7 (24.1%), respectively. All 9 controls underwent surgery (Table 2).
Significant differences in liver function test were found between both the biliary stone patients and controls when compared to the cancer cases. Bilirubin, alkaline phosphatase, aspartate transaminase, and alanine aminotransferase levels were significantly higher in the cancer group than in patients with biliary stones and controls. Albumin levels were lower in the cancer group compared to controls. There were no differences in white blood cell count or cholesterol levels among subjects (Table 3).
Comparison of bile acid concentration among biliary tract cancer, biliary tract stone, and normal control groups
Total concentration of bile acid and the proportion of DCA in the biliary tract cancer, biliary stone, and control groups were 1800.7 ppm, 4005.4 ppm, and 12569.1 ppm, and 2.2%, 10.2%, and 23.6%, respectively. The cancer group had both significantly lower total bile concentration (p = 0.001, p < 0.001) and DCA proportion (p < 0.001, p < 0.001). The proportion of LCA was also significantly lower in the cancer group compared to controls (0.3% vs. 1.0%, p < 0.001) (Table 4).
Analysis was repeated limiting biliary tract disease to the gallbladder site for the cancer and stone groups. Both total bile acid concentration and DCA proportion were found to be lower in the cancer group compared to the stone and control groups; concentrations and proportions were 1346.3 ppm, 5125.5 ppm, and 12569.1 ppm (p = 0.073, p = 0.001), and 6.2%, 14.2%, and 23.6% (p = 0.047, p = 0.031) respectively. LCA was significantly lower in the cancer group compared to controls (0.2% vs. 1.0%, p = 0.016) (Table 5).
Results from analysis limiting biliary tract diseases to the bile duct were 1936.9 ppm, 2805.3 ppm, and 12569.1 ppm for the total bile concentration in the cancer, stone, and control groups, respectively. The cancer group had significantly lower total concentration (p = 0.006, p < 0.001). The proportion of CA in the cancer group was significantly higher than controls (45.0% vs. 33.8%, p = 0.021). DCA was lower in the cancer group compared to the stone and control groups (1.0% vs. 5.8% vs. 23.6%, p = 0.027, p < 0.001, respectively). LCA was also significantly lower in the cancer group than control group (0.3% vs. 1.0%, p < 0.001) (Table 6).
To exclude the effect of bile duct obstruction, cases with bilirubin ≤2.0 mg/dL, without support of bile drainage procedures, were analyzed. Analysis included 3 gallbladder cancer cases, 13 cholelithiasis cases, 7 bile duct cancer cases, 9 choledocholithiasis cases, and 9 controls. Between the cancer and stone group, only alkaline phosphatase was different. Comparison between the cancer and control groups was similar to the results before exclusion. (data not shown) Total bile acid concentration in the cancer, stone, and control groups was 3298.6 ppm, 4522.8 ppm, and 12569.1 ppm, respectively. The cancer group had significantly lower total concentration (p = 0.001), higher CA proportion (50.9% vs. 33.8%, p = 0.009), lower DCA proportion (5.7% vs. 23.6%, p = 0.003), and lower LCA proportion (0.3% vs. 1.0%, p = 0.009) compared to the normal control group (Table 7).
Bile is composed mostly of water along with bile acid, bile pigment, cholesterol, minerals, and fat. Bile acid is produced in hepatocytes via the metabolism of cholesterol, and contributes to formation of bile, excretion of cholesterol, and absorption of fatty meals and lipophilic vitamins.1
The most basic study to evaluate the role of hydrophobic bile acid in biliary tract cancer would be to measure each bile acid in the bile of patients with biliary tract cancer. However, there are few such studies. Strom et al. reported differences in bile composition among subjects with gallbladder cancer, cholelithiasis, and no disease, but found no significant difference in the suspected carcinogen, LCA.10 Lee et al. reported increased DCA in patients with bile duct cancer, yet found no significant difference from biliary stone patients.11 These studies, however, explored a limited spectrum of disease and had no proper controls. Our study analyzed the total bile acid concentration in biliary cancer, biliary stone, and control groups, and also evaluated differences based on disease sites (gallbladder and bile duct). Since DCA is associated with gallstone formation, bile from normal subjects was used as controls.12
We found that the proportion of secondary bile acids, the most strongly suspected carcinogens, were low in bile from subjects with biliary tract cancer. Theoretically, this is because primary bile acid cannot reach bowel sites where conversion to secondary bile acid occurs. However, there are evidences that this may not be the sole reason. Analysis which excluded duct obstruction cases also showed lower DCA proportions in the cancer group. Strom et al. found similar results of this decrease in bile acids in cancer cases, even after removal of clinical obstruction.10 In addition, the total bile acid concentration was lower in the cancer group. Contrary to this result, it is known that bile duct obstruction increases bile acid synthesis.13 In addition, the increase of bile acid in serum caused by obstruction should have increased bile acid level in bile.14 Therefore, obstruction alone can not explain the decrease of total and secondary bile acid.
Besides obstruction, decreased excretion of bile acids by bile duct epithelium might cause the differences seen.10 In vivo, both inflammation and obstruction are known to alter expression of the bile acid transporter.15 In animal models, ligation of the bile duct causes diminished expression of the bile salt export pump and multidrug resistance associated proteins, thereby diminishing bile salt output.16-18 Various endotoxin and inflammatory cytokines also decrease bile salt excretion.19 In addition, decreased bile acid is associated with liver bile acid accumulation.20 The alteration of the bile acid transport pathway may cause decreased excretion of bile acid, and accumulation of toxic and even carcinogenic bile acid in the bile duct epithelium.
As biliary epithelial cells constantly transport strongly cytotoxic components of bile, a chemical carcinogenesis in the bile duct system induced by bile composition changes likely exists. There are interesting reports that the secondary bile acid, DCA, does not cause dysplasia through cytotoxic process alone, but rather augments effects of carcinogens.3 For example, tauroursodeoxycholic acid has been found to promote carcinogenesis of intrahepatic bile duct cancer in hamster models, and taurocholic acid and DCA have been implicated in diisopropanolnitrosamine-induced biliary tract cancer.21,22 Also, the role of secondary bile acids, such as DCA and LCA, together with environmental and genetic factors, is well recognized in colon cancer.23,24 These indirect association, however, cause difficulty in proving a bile acid induced carcinogenic process.
Even though there are not many studies that actually measured bile acid in patients with biliary neoplasm, contrary to our study some reported increased secondary bile acid. The difference in methods might contribute to this discrepancy. First, Strom et al believed that there might be the difference of accuracy between old methods and high pressure liquid chromatography, which also measured bile acid in our study.10 There is also a concentration problem. Many factors could affect the concentration of bile acid. Just comparing the concentration of secondary bile acid between malignant and benign diseases might be not reliable. We rather compared the proportions of each bile acid. Finally, there is a matter of control group. Lee et al reported increased secondary bile acid in bile juice of patients with bile duct cancer.11 However, in that study patients with choledocholithiasis were control group. We did not think patients with biliary stone were good candidates for control group.
There was no significant difference of UDCA between cancer and benign disease observed. A previously reported proportion of UDCA in gallbladder disease was much higher than in our results.10 Association between cancer and UDCA seemed to contradict other studies.2-6 However, there is a study that demonstrated ursodeoxycholate further increased bile-duct cell proliferative response induced by partial bile-duct ligation in rats.25 More studies are needed to find a role of UDCA in carcinogenesis.
Although our study attempted to collect samples under controlled conditions, differences of liver function among groups could not be avoided due to rarity of biliary neoplasm.10 Whether the differences affected the concentration and proportion of bile acids is unknown. White blood cell count in cancer and stone group had rather large standard deviation because it was not always possible to collect bile juice after inflammation subsided completely. Also, control group was significantly younger than disease groups. Collection methods were varied among subjects, and bile collected by gallbladder puncture could be more concentrated than other methods. In addition, conditions such as non-functioning gallbladder, sphincteroplasty, fasting, etc could also affect the concentration of bile acid.26,27 Even though there were such limitations in this study, results were comparable to previous findings, which also showed that total bile concentration and DCA proportion were significantly lower in the cancer group.10 Even though it was not significant, comparison in non-obstructive diseases showed tendency for decreased total bile acid and DCA in the cancer group compared to stone group, and there was no difference of liver function test, except alkaline phosphatase.
In conclusion, in this study, total bile acid concentrations and compositions were measured and compared among subjects with biliary cancer, biliary stone pathology, and controls. Total bile concentration and DCA proportion were lower in the cancer group. Bile duct obstruction contributed but did not completely account for the differences in total bile concentration and composition. We suspect the alteration of bile acid transport might decrease bile acid excretion and cause the accumulation of carcinogenic bile acid in bile duct epithelium. Further studies are needed to prove association between bile acid composition and carcinogenesis.
Figures and Tables
References
1. Javitt NB. Bile acid synthesis from cholesterol: regulatory and auxiliary pathways. FASEB J. 1994. 8:1308–1311.
2. Cameron RG, Imaida K, Tsuda H, Ito N. Promotive effect of steroids and bile acids on hepatocarcinogenesis initiated by diethylnitrosamine. Cancer Res. 1982. 42:2426–2428.
3. Makino T, Obara T, Ura H, Kinugasa T, Kobayashi H, Takahashi S, et al. Effects of phenobarbital and secondary bile acids on liver, gallbladder, and pancreas carcinogenesis initiated by N-nitrosobis (2-hydroxypropyl) amine in hamsters. J Natl Cancer Inst. 1986. 76:967–975.
4. Thompson MB. Bile acids in assessment of hepatocellular function. Toxicol Pathol. 1996. 24:62–71.
5. Einarsson K. Effect of ursodeoxycholic acid on hepatic cholesterol metabolism. Scand J Gastroenterol Suppl. 1994. 204:19–23.
6. Oyama K, Shiota G, Ito H, Murawaki Y, Kawasaki H. Reduction of hepatocarcinogenesis by ursodeoxycholic acid in rats. Carcinogenesis. 2002. 23:885–892.
7. Kinami Y, Ashida Y, Seto K, Takashima S, Kita I. Influence of incomplete bile duct obstruction on the occurrence of cholangiocarcinoma induced by diisopropanolnitrosamine in hamsters. Oncology. 1990. 47:170–176.
8. Kinami Y, Ashida Y, Gotoda H, Seto K, Kojima Y, Takashima S. Promoting effects of bile acid load on the occurrence of cholangiocarcinoma induced by diisopropanolnitrosamine in hamsters. Oncology. 1993. 50:46–51.
9. Funabiki T, Sugiue K, Matsubara T, Amano H, Ochiai M. Bile acids and biliary carcinoma in pancreaticobiliary maljunction. Keio J Med. 1991. 40:118–122.
10. Strom BL, Soloway RD, Rios-Dalenz J, Rodriguez-Martinez HA, West SL, Kinman JL, et al. Biochemical epidemiology of gallbladder cancer. Hepatology. 1996. 23:1402–1411.
11. Lee JH, Park YH, Seo JH, Chung JB, Lee SJ, Chung JP, et al. Biliary bile acid analysis in the patients with bile duct cancer. Korean J Gastroenterol. 2000. 35:103–110.
12. Castleden WM, Detchon P, Misso NL. Biliary bile acids in cholelithiasis and colon cancer. Gut. 1989. 30:860–865.
13. Kinugasa T, Uchida K, Kadowaki M, Takase H, Nomura Y, Saito Y. Effect of bile duct ligation on bile acid metabolism in rats. J Lipid Res. 1981. 22:201–207.
14. Hong SK, Kim KH, Kim WJ. Effect of bile acids on biliary excretion of cholesterol in rabbits. Yonsei Med J. 1973. 14:109–115.
15. Trauner M, Wagner M, Fickert P, Zollner G. Molecular regulation of hepatobiliary transport systems: clinical implications for understanding and treating cholestasis. J Clin Gastroenterol. 2005. 39(4):Suppl 2. S111–S124.
16. Trauner M, Arrese M, Soroka CJ, Ananthanarayanan M, Koeppel TA, Schlosser SF, et al. The rat canalicular conjugate export pump (Mrp2) is down-regulated in intrahepatic and obstructive cholestasis. Gastroenterology. 1997. 113:255–264.
17. Lee JM, Trauner M, Soroka CJ, Stieger B, Meier PJ, Boyer JL. Expression of the bile salt export pump is maintained after chronic cholestasis in the rat. Gastroenterology. 2000. 118:163–172.
18. Paulusma CC, Kothe MJ, Bakker CT, Bosma PJ, van Bokhoven I, van Marle J, et al. Zonal down-regulation and redistribution of the multidrug resistance protein 2 during bile duct ligation in rat liver. Hepatology. 2000. 31:684–693.
19. Bolder U, Ton-Nu HT, Schteingart CD, Frick E, Hofmann AF. Hepatocyte transport of bile acids and organic anions in endotoxemic rats: impaired uptake and secretion. Gastroenterology. 1997. 112:214–225.
20. Shoda J, Kano M, Oda K, Kamiya J, Nimura Y, Suzuki H, et al. The expression levels of plasma membrane transporters in the cholestatic liver of patients undergoing biliary drainage and their association with the impairment of biliary secretory function. Am J Gastroenterol. 2001. 96:3368–3378.
21. Ikematsu Y, Tomioka T, Kitajima T, Inoue K, Tajima Y, Kanematsu T. Tauroursodeoxycholate and cholestyramine enhance biliary carcinogenesis in hamsters. World J Surg. 2000. 24:22–26.
22. Holzinger F, Z'graggen K, Buchler MW. Mechanisms of biliary carcinogenesis: a pathogenic multi-stage cascade towards cholangiocarcinoma. Ann Oncol. 1999. 10:Suppl 4. 122–126.
23. Tocchi A, Basso L, Costa G, Lepre L, Liotta G, Mazzoni G, et al. Is there a causal connection between bile acids and colorectal cancer? Surg Today. 1996. 26:101–104.
24. Nagengast FM, van den Ban G, Ploemen JP, Leenen R, Zock PL, Katan MB, et al. The effect of a natural high-fibre diet on faecal and biliary bile acids, faecal pH and whole-gut transit time in man. A controlled study. Eur J Clin Nutr. 1993. 47:631–639.
25. Barone M, Maiorano E, Ladisa R, Pece A, Berloco P, Strazzabosco M, et al. Ursodeoxycholate further increases bile-duct cell proliferative response induced by partial bile-duct ligation in rats. Virchows Arch. 2004. 444:554–560.
26. Antsaklis G, Lewin MR, Sutor DJ, Cowie AG, Clark CG. Gallbladder function, cholesterol stones, and bile composition. Gut. 1975. 16:937–942.
27. Cohn MS, Schwartz SI, Faloon WW, Adams JT. Effect of sphincteroplasty on gallbladder function and bile composition. Ann Surg. 1979. 189:317–321.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download