Abstract
We evaluated the feasibility of the transradial coronary intervention (TRCI) in 85 consecutive patients with chronic total occlusion (CTO). Clinical, angiographic and procedural factors were compared between the success and failure groups. An overall success rate of 65.5% (57 of 87 lesions) was achieved with TRCI, and the most common cause of failure was an inability to pass the lesion with a guidewire. A multivariate analysis demonstrated that the most significant predictor of failure was the duration of occlusion (OR 1.064 per month, 95% CI 1.005 to 1.126, p = 0.03). The procedural success rate improved with use of new-generation hydrophilic guidewires. The 6 Fr guiding catheters were used in the majority of the 70 cases (81%). Five cases were crossed over to a femoral artery approach due to engagement failure of the guiding catheter into the coronary ostium because of severe subclavian tortuosity and stenosis in two cases, radial artery looping in one case, and poor guiding support in two cases. There were no major entry site complications. In conclusion, the radial artery might be a feasible vascular route in coronary interventions for CTO, with comparable procedural success and no access site complications.
Percutaneous coronary intervention (PCI) for chronic total occlusions (CTO) has been limited due to a low success rate and a high restenosis rate. However, the complication rate of PCI is low and the success rate has increased in recent years due to improved procedural techniques and devices.1,2 Successful recanalization improves clinical symptoms and cardiac function and increases the long-term survival rate in patients with CTO.3-5
The femoral artery is the usual vascular route used in PCI for CTO in most cardiac catheterization laboratories. However, when the femoral artery is used as the approaching vessel, local hemorrhage is a common complication.3 Accordingly, there has been growing interest in transradial PCI because of decreased complications at the puncture site, patient convenience, earlier discharge, and shorter hospitalization.6,7 Furthermore, the indications for transradial PCI are expanding due to the miniaturization of devices used, improvements in devices and techniques, and accumulated experience in transradial PCI.
Thus, we evaluated the feasibility of transradial coronary intervention in CTO by reviewing the success rate, selection of devices, such as guiding catheter and guide wires, and procedural complications in patients who underwent transradial PCI for CTO.
We examined 87 lesions in 85 consecutive patients, showing a positive Allen's test,8 who underwent transradial PCI for CTO from March 2000 to October 2003. Patients who had negative Allen's tests for both wrists, chronic renal failure requiring dialysis, or chronic renal failure that would require dialysis in the future were excluded from the study. All of these patients gave written informed consent, and the study was approved by the ethnics committee of the Wonju Christian Hospital.
Definition of Terminology: A CTO was defined as a lesion exhibiting a Thrombolysis in Myocardial Infarction (TIMI) flow grade of 0-1 in a native coronary artery, with a duration of occlusion of more than one month.9 The age of the CTO was determined, using clinical information, such as the past history of myocardial infarction, changes in the pattern of chest pain, or findings of total occlusion from previous coronary angiography. Early chronic occlusion was defined as total occlusion of a one to three month duration, and late chronic occlusion was defined as total occlusion with a duration longer than three months.9 The morphology at the point of occlusion was classified as either a tapered or abrupt end.10 The length of the occlusion was measured from the occlusion to the distal portion of the vessel filled by collateral flow or by the length of significant stenosis seen after passing the wire or predilated balloon catheter. The extent of collateral circulation was classified as grade 0 to 3, according to the classification of Cohen and Rentrop.11
Successful transradial PCI was defined as completion of the procedure via the radial artery without crossover to the femoral artery, with a residual stenosis of less than 30% and no major cardiovascular complications (Type C, D or E dissection, myocardial infarction, emergency CABG, or death). We divided the study period into initial and late period, according to the median value (1.9 years) of the study period.
PCI was performed via the left or right radial artery. The arterial sheath, a 7 Fr MAXIMUM sheath (Daig Corp., Minnesota) or 6 Fr RADIFOCUS sheath (Terumo Co., Tokyo, Japan) was selected before the procedure by considering the radial artery size and the guiding catheter selected for the lesion. All patients received 10,000 U of heparin through the arterial sheath. The CTO lesion was typically approached with a 1.5-mm or 2.0-mm over-the-wire (OTW) balloon catheter over 0.014-inch flexible guidewires. If the flexible guidewire was unable to cross the lesion, the guide wire was changed to a stiffer or more hydrophilic wire. When the distal course of the occluded coronary artery was unclear, simultaneous contralateral coronary angiography was performed via the femoral artery.12 The procedure was terminated if more than 400 mL of contrast agent was used, if the guide wire was placed in the false lumen with extravasation of contrast, or if the procedure lasted longer than one hour. The sheath was removed immediately after the procedure in the catheterization laboratory. A compression dressing with gauze was placed at the puncture site and maintained for at least six hours.
Data analysis: Statistical analysis was performed, using the SPSS 12.0 statistical program (SPSS Inc., Chicago, IL, USA). Continuous variables are expressed as mean ± SD. Continuous variables were compared, using the Student's t-test, and the differences between categorical variables were examined, using the chi-square test. A p-value < 0.05 was considered statistically significant.
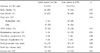
The baseline clinical characteristics of 87 cases in the success and failure groups are listed in Table 1. There were no significant differences in coronary risk factors, such as hypertension, diabetes, history of smoking, or low-density lipoprotein cholesterol level between the two groups. The clinical diagnosis was unstable angina pectoris in 36 cases (42%), heart failure in 26 cases (29%), and stable angina pectoris in 23 cases (27%). The duration of chronic occlusion was 4.8 ± 8.0 months in the success group and 13.5 ± 16.1 months in the failure group, showing a significantly longer duration in the failure group (p < 0.01). Success was seen in 27 of the 32 cases (84%) with early chronic occlusion and in 32 of the 55 cases (58%) with late chronic occlusion, revealing a significant difference according to the duration of occlusion (p = 0.017). The extent of coronary disease included single vessel disease in 42 cases (48%) and multi-vessel disease in 45 cases (52%) (Table 1). The site of CTO was the left anterior descending in 45 cases (52%), right coronary artery in 31 cases (36%), and left circumflex in 11 cases (13%), with no statistically significant difference between groups.
PCI was performed on an ad hoc basis immediately after the diagnostic angiography in most cases (97%), with 52 of 54 cases (96%) approached via the right radial artery and 32 of 33 cases (97%) approached via the left radial artery. The success rate of transradial PCI was 65.5% (57 of 87 cases), and the causes of failure included failure to pass the guidewire through the lesion in 24 of 30 failed cases (80%), failure of balloon passage in 1 case (3%), failure to pass the guiding catheter through the radial artery due to subclavian artery tortuosity or omega loops of the radial artery in 3 cases (10%), and failure due to poor guiding support in 2 cases (7%). In five cases, involving poor guiding support and subclavian/radial tortuosity cases, the PCI were crossed over to the femoral artery on the same day. Two cases of subclavian/radial tortuosity had successful outcomes. The lesion characteristics that correlated with successful PCI included a lack of side branches or bridging collateral vessels, occlusion of less than 15 mm, and a tapered occlusion morphology (Table 1).
A multivariate analysis of predictors of failure implicated only the duration of occlusion (OR 1.064 per month, 95% CI 1.005 to 1.126, p = 0.03).
Among 87 cases of transradial PCI, a 6 French guiding catheter was used in 70 cases (81%), and a 7 French guiding catheter was used in 15 cases (17%). The average number of guiding catheters used per case was 1.2 ± 0.5, and 68 (78%) procedures were done using only the initially selected guiding catheter. The types of guiding catheters used when the lesions were located at the left anterior descending artery are as follows: Judkins in 28 of the 45 cases (62%), KIMNY in 10 cases (22%), RAD in 2 cases, and Amplatz (AL1) in 5 cases. Among a total of 31 cases of PCI performed with the target lesion in the right coronary artery, Amplatz (AL1) guiding catheters were used in 16 of those cases (52%), KIMNY in 8 cases (26%), Judkins in 4 cases (13%), and Amplatz (AR1) in 3 cases (10%). When the target lesion was in the left circumflex artery, Judkins guiding catheters were used in 7 cases, KIMNY in 2 cases, and Amplatz (AL1) guiding catheters in 2 cases (Fig. 1). The average number of guidewires used per case was 1.5 ± 0.6. The most frequently used guidewire was the ACS Hi-Torque standard (Guidant, Santa Clara, CA, USA), which was used in 33 cases (38%), followed by a hydrophilic-coated guidewire - Choice PT (Boston Scientific, Watertown, MA, USA), Whisper MS (Guidant, Santa Clara, CA, USA), and Crosswire NT (Terumo Co., Tokyo, Japan) in 21 cases (24%). OTW balloon catheters or multifunctional probing catheters were used in 63 cases (72%).
Coronary stents were implanted in 52 of the 59 successful cases (88%). The indications for stent insertion were primary stent implantation in 44 cases and bailout stent implantation in 8 cases.
Procedure-related complications occurred in three cases: coronary perforation in two cases and one case of asymptomatic, non-ST elevation myocardial infarction with a CK-MB increase to 18 ng/mL. There were no Q-wave myocardial infarctions or deaths and no local vascular hemorrhagic complications related to the transradial intervention.
Successful transradial PCI was achieved in 57 of 87 cases (65.5%) and, in 5 cases, the catheters were crossed over to the femoral artery due to anatomical variations in the radial or subclavian arteries. The success rate of transradial PCI was similar to the success rates reported in the meta-analyses (53-68%)8 but lower than the 70-75% reported by a few authors,2,13-15 probably because the proportion of late chronic lesions was high in the present study, accounting for 63.2% (55 of 87 cases), compared with an average of 38.7% (15-57%) reported by other authors. Puma et al.,9 in their meta-analysis, reported that chronicity is the most important factor in successful intervention and that the success rate in late chronic occlusion was significantly lower (37%, 198 of 529 cases) than that in early chronic occlusion (75%, 623 of 836 cases). The success rate in early chronic occlusion in our study was 84% (27 of 32 cases), significantly different from the success rate of 58% (32 of 55 cases) in late chronic occlusion. Other factors affecting the success in PCI for CTO lesions include the presence or absence of side branches and bridging collateral vessels, occlusion length, reference diameter less than 3 mm, and occlusive morphology.9,10 In our study, the factors affecting the success of transradial PCI for CTO were also similar to these previous reports (Table 1). Although the success of a CTO intervention might dependent on experience, the lesion type, and indications for intervention, the devices used for the procedure are critically important to the outcome, particularly in the case of transradial intervention.
When the radial approach for CTO intervention is attempted, availability of sufficient guiding support becomes a major concern since it is generally not feasible to use a guiding catheter larger than 7 Fr. Accordingly, transfemoral coronary intervention is often preferred over transradial PCI for CTO because 7 or 8 Fr guiding catheters may be used to obtain greater back-up support, as compared to the 6 Fr guiding catheters frequently used in the transradial approach. However, because catheter materials have improved a great deal, and because special curvature is available to increase support, we were able to achieve sufficient guiding support with a 6 Fr guiding catheter in most cases.
Ikari et al. reported that a special guiding shape, such as the Ikari guiding catheter, achieved a similar level of backup force in both transradial and transfemoral approaches, indicating that support depends primarily on catheter shape and size, not approach site.16
In some cases, the "deep intubation technique" was applied to the guiding catheter to achieve greater back-up support.17
There is no data regarding the selection of the guiding catheters used for transradial PCI for CTO lesions. In this study, the selection of guiding catheters was based on the lesion characteristics and the radial artery size. A 6 Fr guiding catheter was most frequently used. The type of guiding catheters used for CTO was different from those needed for transradial PCI for other coronary lesions. In our study, transradial PCI for a CTO lesion was possible using Judkins guiding catheters in 62% when the lesion was in the left coronary artery and in 13% when in the right coronary artery. The Judkins right guiding catheter was used less often, compared with the results reported by Lotan et al.,7 who reported that Judkins (JL) guiding catheters were used in 49% of cases for the left coronary artery, while Judkins (JR) guiding catheters were used in 57% of cases for the right coronary artery in transradial PCI. These differences in the rates of using Judkins right catheters were probably due to the need for a guiding catheter with a special curve that could give sufficient backup support when performing PCI for CTO lesions in the right coronary artery. The results of the present study indicated that KIMNY or Amplatz guiding catheters would be excellent guiding catheter choices when performing transradial PCI for CTO lesions in the right coronary artery. Furthermore, guidewire selection and adoption of an OTW balloon catheter or a multi-probing catheter to get more stable backup support for the guidewire is an important technical point in the CTO intervention. In our study, conventional wire-balloon techniques were performed in most cases; over-the-wire (OTW) balloon catheters or multifunctional probing catheters were used in 72% of the cases.
We divided the study period into initial and late segments, according to the median length (1.9 years) of the study period. The reasons for improved success in the CTO intervention might include technical advances, such as more frequent use of hydrophilic wires or the simultaneous contralateral injection technique (Table 2). Guidewire selection has been modified over time. During the second half of the study period, second generation guidewires were more frequently tried (Table 2).18 The most frequent cause of failure in the present study was a failure to pass the guidewire through the lesion (80%), and an independent predictor of failure was the duration of CTO. Srivasta et al.19 observed that, histologically, newer CTO lesions are predominantly soft or lipid-laden, whereas older CTO lesions are typically hard or fibrocalcific and, therefore, less favorable to guidewire passage or dilatation. This suggests that the use of new types of guidewires or adjunctive devices may help to increase the success rate of patients with CTO lesions. Lafevre et al.13 reported successful guidewire passage in 73.8% and 34.8% of cases, using hydrophilic or conventional guidewires, respectively, showing a marked improvement in guidewire lesion passing with new generation guidewires in CTO lesions. The hydrophilic-coated guidewires, Choice PT, Whisper MS, and Crosswire NT, which are being used more frequently in recent years, were used in 20 cases (38%) in the later part of our study. Active selection of new generation guidewires should be an effective way of decreasing the passage failure rate. Various methods, such as using a ball-ended guidewire,14 a laser guidewire,20 applying optical coherent reflectometry for safe navigation of guidewire,21 and performing the procedure again after administering thrmobolytics through the coronary artery,22 have successfully been employed for guidewire passage. Recently, the blunt controlled intraluminal micro dissection catheter23 and radiofrequency ablation guidewire24 have been reported to improve the success rate in CTO.
In-hospital cardiovascular complications were seen in three cases (3.4%); coronary perforations in two cases, due to guidewire and balloon inflation, and non-Q wave myocardial infarction with a greater than three-fold CK-MB mass increase in one case. However, no Q-wave myocardial infarctions or deaths occurred, and no entry site complications, such as hemorrhage at the puncture site, were observed.
Suero et al.3 reported the rate of major cardiovascular complications in the hospital to be 3.8%, including myocardial infarction (2.4%) and death (1.3%), and the rate of local vascular complication to be 1.7%. No statistically significant difference in the rate of in-hospital complications between CTO and non-CTO lesions was found.3 The rate of complications was very low in the present study. In particular, there were no cases of entry site complications, because the arterial sheath was removed immediately after the procedure, and pressure application was facilitated by the superficial course of the radial artery. As a result, there were no cases of hemorrhage.
Although this study showed promising data, an important limitation of this study is its retrospective and observational nature, as well as the lack of comparison to the femoral approach. Further study, particularly of the randomized control type, will be required.
Despite these limitations, this study suggested that the radial artery might be a feasible vascular route for PCI of CTO, with comparable procedural success rates and no major site complications.
Figures and Tables
Fig. 1
Kinds of guiding catheters used in a radial approach among 87 chronic total occlusions. AL, Amplatz left; LCA, left coronary artery; RCA, right coronary artery.

Table 1
Clinical and Angiographic Characteristics of the Transradial PCI Success and Failure Groups

Values are mean ± SD.
*p value < 0.05.
BMI, body mass index; LVEF, left ventricular ejection fraction; MI, myocardial infarction; CTO, chronic total occlusion; DM, diabetes mellitus; Mo, months; LAD, left anterior descending artery; LCx, left circumflex artery; RCA, right coronary artery; TO, total occlusion; RD, reference diameter; PCI, percutaneous coronary intervention.
References
1. Meier B. "Occlusion angioplasty" Light at the end of the tunnel or dead end? Circulation. 1992. 85:1214–1216.
2. Bahl VK, Chandra S, Goswami KC, Manchanda SC. Crosswire for recanalization of total occlusive coronary arteries. Cathet Cardiovasc Diagn. 1998. 45:323–328.
3. Suero JA, Marso SP, Jones PG, Laster SB, Huber KC, Giorgi LV, et al. Procedural outcomes and long term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J Am Coll Cardiol. 2001. 38:409–414.
4. Ivanhoe RJ, Weintraub WS, Douglas JS, Limbo NJ, Furman M, Gershony G, et al. Percutaneous transluminal coronary angioplasty of chronic total lesions. Primary success, restenosis, and long-term clinical follow-up. Circulation. 1992. 85:106–115.
5. Isobe N, Sugawara M, Taniguchi K, Oshima S, Hoshizaki H, Toyama T, et al. Delayed recovery of left ventricular regional work after coronary angioplasty in patients with opposite wall old myocardial infarction. Heart Vessels. 2003. 18:61–66.
6. Kiemeneij F, Laarman GJ, Slagboom T, van der Wieken R. Outpatient coronary stent implantation. J Am Coll Cardiol. 1997. 29:323–327.
7. Lotan C, Hasin Y, Mosseri M, Rozenman Y, Admon D, Nassar H, et al. Transradial approach for coronary angiography and angioplasty. Am J Cardiol. 1995. 76:164–167.
8. Safian RD, Freed MS. The manual of interventional cardiology. 2001. 3rd ed. Michigan: Physicians' Press;36–37.
9. Puma JA, Sketch MH Jr, Tcheng JE, Harrington RA, Phillips HR, Stack RS, et al. Percutaneous revascularization of chronic coronary occlusions: an overview. J Am Coll Cardiol. 1995. 26:1–11.
10. Tan KH, Sulke N, Taub NA, Watts E, Karani S, Sowton E. Determinants of success of coronary angioplasty in patients with a chronic total occlusion: a multiple logistic regression model to improve selection of patients. Br Heart J. 1993. 70:126–131.
11. Rentrop KP, Cohen M, Blanke H, Phillips RA. Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol. 1985. 5:587–592.
12. Grolier G, Commear P, Foucault JP, Potier JC. Angioplasty of chronic totally occluded coronary arteries: usefulness of retrograde opacification of the distal part of the occluded vessel via the contralateral coronary artery. Am Heart J. 1987. 114:1324–1328.
13. Lafevre T, Louvard Y, Loubeyre C, Dumas P, Piechaud JF, Krol M, et al. A randomized study comparing two guidewire strategies for angioplasty of chronic total coronary occlusion. Am J Cardiol. 2000. 85:1144–1147.
14. Allemann Y, Kaufmann UP, Meyer BJ, Gunnes P, Urban P, Mulhauser B, et al. Magnum wire for percutaneous coronary balloon angioplasty in 800 total chronic occlusions. Am J Cardiol. 1997. 80:634–637.
15. Kinoshita I, Katoh O, Nariyama J, Otsuji S, Tateyama H, Kobayashi T, et al. Coronary angioplasty of chronic total occlusions with bridging collateral vessels: immediate and follow-up outcome from a large single-center experience. J Am Coll Cardiol. 1995. 26:409–415.
16. Ikari Y, Nagaoka M, Kim JY, Morino Y, Tanabe T. The physics of guiding catheters for the left coronary artery in transfemoral and transradial interventions. J Invasive Cardiol. 2005. 17:636–641.
17. Hamon H, Fadden E. Trans-radial approach for cardiovascular interventions. 2003. Carpiquet: Europa Stethoscope Media;181–196.
18. Saito S, Tanaka S, Hiroe Y, Miyashita Y, Takahashi S, Satake S, et al. Angioplasty for chronic total occlusion by using tapered-tip guidewires. Catheter Cardiovasc Interv. 2003. 59:305–311.
19. Srivasta SS, Edwards WD, Boos CM, Grill DE, Sangiorgi GM, Garratt KN, et al. Histologic correlates of angiographic chronic total coronary artery occlusions: influence of occlusion duration on neovascular channel patterns and intimal plaque composition. J Am Coll Cardiol. 1997. 29:955–963.
20. Hamburger JN, Serruys PW, Scarbra-Gomes R, Simon R. Recanalization of total coronary occlusions using a laser guidewire (The European TOTAL surveillances study). Am J Cardiol. 1997. 80:1419–1423.
21. Cordero H, Warburton KD, Underwood PL, Heuser RR. Initial experience and safety in the treatment of chronic total occlusions with fibroptic guidance techno logy: Optical Coherent Reflectometry. Catheter Cardiovasc Interv. 2001. 54:180–187.
22. Cecena FA. Urokinase infusion after unsuccessful angioplasty in patients with chronic total occlusion of native coronary arteries. Cathet Cardiovasc Diagn. 1993. 28:214–218.
23. Whitbourn RJ, Cionocotta M, Mossop P, Selmon M. Intraluminal blunt micro dissection for angioplasty of coronary chronic total occlusions. Catheter Cardiovasc Interv. 2003. 58:194–198.
24. Chen WH, William N, Lee PY, Lau CP. Recanalization of chronic and long occlusive in-stent restenosis using optical coherence reflectometry-guided radiofrequency ablation guidewire. Catheter Cardiovasc Interv. 2003. 59:223–229.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download