Abstract
In the present study, we examined the relationship between average fish consumption, as well as the type of fish consumed and levels of mercury in the blood of pregnant women. We also performed follow-up studies to determine if blood mercury levels were decreased after counseling and prenatal education. To examine these potential relationships, pregnant women were divided into two groups: a study group was educated to restrict fish intake, whereas a control group did not receive any prenatal education regarding fish consumption. We measured blood mercury level and performed follow-up studies during the third trimester to examine any differences between the two groups. Out of the 63 pregnant women who participated in our study, we performed follow-up studies with 19 pregnant women from the study group and 12 pregnant women from control group. The average initial blood mercury level of both groups was 2.94 µg/L, with a range of 0.14 to 10.75 µg/L. Blood mercury level in the group who ate fish more than four times per month was significantly higher than that of the group who did not consume fish (p = 0.02). In follow-up studies, blood mercury levels were decreased in the study group but slightly increased in the control group (p = 0.014). The maternal blood mercury level in late pregnancy was positively correlated with mercury levels of cord blood (r = 0.58, p = 0.047), which was almost twice the level found in maternal blood. Pregnant women who consume a large amount of fish may have high blood mercury levels. Further, cord blood mercury levels were much higher than that of maternal blood. Because the level of fish intake appears to influence blood mercury level, preconceptual education might be necessary in order decrease fish consumption.
Mercury is an accumulative harmful material that is not required for normal human physiological functions and is capable of damaging the nervous systems of humans and animals.1 In the nature, mercury exists as elemental mercury, inorganic mercury, and organic mercury. Humans can be exposed to mercury in the form of air pollution, pesticides, medical materials, such as thermometers and amalgam, or food that we consume everyday.
Elemental mercury is used in such objects as thermometers, sphygmomanometers, and dental amalgam; it is also present in workplaces, such as gold refinement facilities. When consumed orally, elemental mercury is hardly absorbed; however, upon vaporization, absorption becomes possible. Inorganic mercury is present in corrosive sublimates, pesticides, explosives, and as a preservative in some medicinal preparations. While coal oxidizes mercury in thermal power plants, it may still pollute the air, eventually accumulating in streams and oceans. Inorganic mercury itself is not readily absorbed by either the digestive tract or the skin, and it does not penetrate the placenta. However, microorganisms can convert inorganic mercury to organic mercury, which is toxic. Such organic mercury can be consumed by small animals, and, thus, it may be incorporated into the food chain. Indeed, concentrations of mercury are highest in large, predatory fish. Organic mercury is a lipid-soluble substance that is predominantly in the form of methyl or ethyl mercury. Organic mercury is distributed to all tissues and becomes more concentrated in the blood and brain than other forms of mercury. Organic mercury is readily absorbed by the digestive tract and excreted through bile rather than urine; however, its half-life is approximately 70 days, and its extracorporeal excretion is slow. Thus, it can readily accumulate in the body. Furthermore, organic mercury can readily penetrate the blood-brain barrier and the placenta and has a high affinity for the central and peripheral nervous systems. Initially, the symptoms of mercury poisoning are numbness of the hands and feet; however, in cases of severe poisoning, the development of nervous tissue may be impaired in growing children, and, in adults, severe neurotoxicity, such as dysphagia, defects in the visual field, and insanity, may emerge.
Organic mercury poisoning has developed from the consumption of fish containing of mercury (Japan 1953) and bread made from wheat treated with mercury-containing sterilizers (Iraq 1972).1,2 Methyl mercury, the predominant form of organic mercury, is bioaccumulated in the human body primarily by consuming seafood, freshwater fishes, and shellfish,3 Organic mercury concentration is high in long-lived, predatory fishes that have abundant opportunities for accumulating mercury.4-6 In fact, it has been reported that the concentration of mercury in the hair or blood is higher for those in island areas where fish consumption is high than for residents in mainland USA, despite the equivalence of mercury levels in fish in both areas.4 Indeed, the average concentration of mercury in pregnant women in Japan, where the consumption of fish is higher than the USA, is also significantly higher.6-8 Since fish have been increasingly reported as a health food, pregnant women tend to consume fish in a large quantities, and, consequently, the blood mercury concentration in pregnant women has increased. Further, it has been reported that, in such cases, the blood mercury concentration is low for the pregnant woman themselves, and, thus, they are asymptomatic. However, methyl mercury can penetrate the placental and blood-brain barrier, and, thus, the fetus, whose brain and the nervous development is ongoing, can be dangerously exposed. Consequently, after birth, while growth continues, mercury exposure may cause the impairment of central nervous system development, resulting in irreversible damage.9,10 A recent study has also suggested that prenatal exposure to mercury among a population with high fish consumption may cause development delays offspring.5 Furthermore, it has been reported that the mercury concentration in the umbilical cord blood is higher than the mercury concentration in the blood of the pregnant mother,7,11 and, thus, it is thought that the risk of the damage by mercury to the central nervous system of the fetus may be higher that after birth.
Given the potentially devastating effects of fetal exposure to mercury, the US Food and Drug Administration (FDA) provides advice to pregnant women and women of childbearing age who may become pregnant to reduce consumption of predatory fishes that contain a high concentration of mercury, such as swordfish, shark, king mackerel, or tile fish, and to avoid consuming more than 340g of other fishes. The FDA gives the same recommendation for nursing women and children, for whom development of the central nervous system is still active.12,13 Furthermore, the US Environment Protection Agency (EPA) recommends that the total blood mercury concentration remain lower than 5.8 µg/L for women of childbearing age.8 In addition to the USA, Canada and the British Standard Agency have also provided guidance.14,15
In Korea, the effects of the recent crises of mad cow disease, bird flu, hand, foot, and mouth disease, and so forth have produced a mentality whereby fish consumption is thought to be relatively safer. Further, as individuals obtain greater financial leeway, great numbers are consuming fish that was previously too expensive to purchase. Because of these issues, as well as the decreasing number of children, increased causality of neonatal central nerve damage and inexplicable developmental impairment in infancy had been previously ignored, the mercury poisoning of pregnant women has became a subject of interest. Interest in heavy metal poisoning, in general, includingthat by mercury, is increasing.
In our study, the correlation of the fish consumption rate of pregnant women, as well as the type of fish consumed, and the blood mercury level in pregnant women was examined. To assess the necessity of prenatal education in the future, we simultaneously examined blood mercury concentration with respect to basic knowledge of pregnant women in Korea and determined whether a decrease in fish consumption, as suggested by prenatal counseling and education, actually lowers the blood mercury levels relative to levels at early pregnancy. Lastly, we evaluated the relationship between mercury levels of maternal and cord blood.
This study was performed using pregnant women who visited the obstetrics outpatient clinic at our hospital from March to December in 2004. Women with abnormal pregnancies with complications, such as preclampsia, twin pregnancy, etc. were excluded from the study population.
During a patients first visit to our hospital, the aim and method of this study, as well as its usefulness, were explained. Subsequently, a survey questionnaire was taken only by patients who wished to participate in the study. The questionnaire included the frequency of fish consumption, type of fish consumed. To rule out other factors contributing to the blood mercury concentration in vivo, the questionnaire also asked about jobs that may cause exposure to mercury, and whether she had lived or was living in areas where the exposure to mercury was possible. The blood mercury concentration was measured for participating pregnant women visiting our hospital for the first time during early pregnancy, and the correlation of the routine fish consumption and the type of fishes consumed to the blood mercury concentration was examined. The study population was divided into a control group, who consumed fishes as usual, and an experimental group, who received prenatal educated to avoid consuming fishes. After collecting the blood for the first time, the date when the half-life of methyl mercury 70 days would be reached was determined, and during the triple test of mother's blood at the midtrimester of pregnancy or during the hospital visit for pregnancy diabetes test, follow up observations of the blood mercury levels were carried out. For pregnant women who visited our hospital for the first time during the midtrimester, taking into consideration the half-life of mercury, the follow up test was performed while they were hospitalized for the delivery. When pregnant women visited the hospital for delivery, maternal blood sampling was performed, and cord blood sampling was done at the time of delivery. A total 63 pregnant women participated in our study, and among them, follow up studies were performed on 12 cases of the control group and 19 cases of the study group. Also, 12 cord blood samples were obtained.
For blood collection during visits by pregnant women, we used tubes treated with EDTA (ethylenediaminetetraacetic acid) and a whole blood 5 mL vacutainer (Beckton & Dicktion, Los Angeles, CA, USA). Venous blood was drawn directly, temporarily stored in dry ice, and stored at -70℃ until analysis. Immediately prior to the analysis, blood samples were thawed slowly at room temperature, and the vacutainer tube was shaken sufficiently to mix the blood and EDTA. Next, a 0.5 mL sample was removed, to which 5 ml HNO3 was added, and then pretreated in a microwave oven. The total volume was adjusted to 50 mL with deionized water, and to determine mercury concentration, a mercury analyzer equipped with deoxidation of vapor (CETAC technologies inc, M-600A, Omaha, Nebraska, USA) was used. The determined blood mercury concentration included all mercury such as metal mercury, inorganic mercury, organic mercury, etc.; the detection limit was 10 ppt (10-12 gm/L). Analysis conditions of the blood mercury analyzer were as follows: lamp wavelength was 253.7 nm, lamp temperature was 125℃, argon main pressure was 60 Psi, and gas flow was 60 mL/min. The detection limit of the analyzer is 0.0051 Ug/L (limit of quantity) and in this case the reference value was 1.27 (0.76-1.77) µg/L and 2.76 (1.91-3.61) µg/L, and the analysis data was 0.83-1.34 µg/L and 2.21-3.21 µg/L, respectively.
Due to the small sample number, Kruskal-Wallis and Mann-Whitney tests were used for statistical analysis of the two groups. For the comparison of relationship of between the two groups, Spearman correlation coefficients were used. A p value less than 0.05 was considered to be a significant.
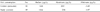
A total 63 pregnant women participated in our study. For the study participants, the initial blood mercury concentration was determined; spontaneous abortion occurred in 4 cases during the follow up period, and at the end of the study, followed up blood mercury concentrations were obtained for 12 cases of the control group and 19 cases of the study group. Pregnant women who worked or lived in an area that may expose them to mercury were not included in our study. The mean age of the pregnant women was 31 years (24-40 years), and at the first visit, the blood mercury concentration of the pregnant women was 2.94 µg/L (range: 0.14-10.75 µg/L). Upon examination of the the blood mercury concentration with respect to the level of fish consumption, regardless of the type of fishes, the blood mercury level for pregnant women who consumed fish more than 12 times a month was higher than that of the others groups. The difference between groups was statistically significant (Table 1, p = 0.02).
The concentration of mercury according to the type of fish consumed was not statistically significant; however, there was a tendency for an increased blood mercury level for pregnant women who consumed a large quantity of mackerel or big fish compared to women who ate seashell or shrimp (Table 2, p = 0.384).
For the follow up results, blood mercury levels were decrease in the study group who were educated to avoid consumption of fish, but slightly increased in the control group; this difference was statistically significant. (Table 3, p = 0.014). Fig. 1 and 2 show the change in blood mercury levels for the two groups.
The maternal blood mercury level in late pregnancy was positively correlated with cord blood (Table 4, r = 0.58, p = 0.047) and cord blood mercury level were almost twice that found in maternal blood.
Mercury is a well-established, cumulative neurotoxic agent that can have serious adverse effects on the development and functioning of the human central nervous system, especially when exposure occurs prenatally.16 Given the potential threat that methyl mercury poses to the optimal development of cognitive function, clinicians and regulatory agencies are concerned about the levels of methyl mercury that a pregnant women regularly ingests,16 and the levels organic mercury in diets, especially from fish containing methylmercury, which is a major source of mercury exposure to the general population. While cases in which treatment with dental amalgam resulting in elevated the blood mercury concentration have been reported, other clinicians have indicated this is not the case.17 Therefore, this issue remains controversial.
Fishes that are inexpensive and contain essential nutrients, as well as omega-3 fatty acids, are nutritious foods which we encounter frequently in daily life. Particularly, fish are a high-protein and fatty food source recommended to children, pregnant women, and the aged. Furthermore, it has been reported that the polyunsaturated fatty acids that are abundant in fish oils may actually confer benefits to the fetus, such as reduced risk of preterm delivery and enhanced infant cognition;18,19 these fatty acids have been shown to help in the prevention of cardiovascular disease, as well.20 Despite these health benefits, some fishes contain a very high concentration of mercury due to food chain bioaccumulation, and, consequently, in cases of large-quantity fish consumption, blood mercury levels can become high enough such that the cardioprotective effects of fish intake are decreased.21 In March 2004, the Department of Health and Human Services and the Environment Protection Agency of the USA published a repor,t entitled 'What You Need to Know about Mercury in Fish and Shellfish,' which showed that nearly all fish and shellfish contain trace amounts of mercury. Thus, to avoid mercury contamination, the report recommended limiting fish consumption to 12 ounces (approximately 340 gm) per week and eating a variety of fish and shellfish that are low in mercury. According to the report, the five most commonly consumed fish that are low in mercury, and thus recommended, are shrimp, canned light tuna, salmon, pollock, and catfish. In contrast to canned tuna that is made of small tunas, the mercury content of white tuna is high, and, thus, it was suggested that one should not consume more than 6 ounces (approximately 170 gm) per week.12 Furthermore, the British Food Standard Agency recommends that pregnant women, women of childbearing age, and children under 16 years of age avoid consuming swordfish because of its high mercury content. With respect to tuna, it is recommended that pregnant women and women of childbearing age should avoid consuming tuna steak more than twice per week.15
Health Canada recommends restricting the consumption of shark, swordfish, and tuna sashimi to less than once per week, and, if possible, less than once per month for pregnant women, women of childbearing age, and children.13 On the other hand, in Korea, special guidelines on the consumption of fish for pregnant women or women of childbearing age are not available, and the Department of Food and Drug Administration defines the standard of the total residual mercury in fishes as 0.5 mg/kg, excluding abyssal fishes and tunas.22 In April 2004, because of increased social interest in poisoning caused by mercury contained in fishes, the citizen's group, 'Consumer Korea,' performed the 'test on total mercury in fishes in Korea'.23 The test results showed that, in swordfish and Thennus obesus, a kind of tuna, mercury levels are higher than the standard level of 0.5 mg/kg, while levels in other fishes, such as flatfish, mackerel, and canned tuna, were below the standard level.23
In the present study, we measured, for the first time in Korea, the blood mercury concentration in pregnant women. We also showed, for the first time in Korea, that blood mercury levels are correlated with the frequency of fish consumption. According to blood samples taken from patients' first visits to the hospital, the blood mercury concentration in pregnant women was, on average, 2.94 µg/L. While the small sample size makes simple comparisons difficult, the average blood mercury concentration in pregnant Korean women, according to our data, was, indeed, higher than the women of childbearing age in the USA (2.94 vs 1.02 µg/L).8 Nevertheless, the Korean average was substantially lower, compared to Japanese women (18.2 ± 9.9, 19 ± 36 µg/L) who consume fish in a larger quantity.7, 8 In addition, the blood mercury concentrations of the study subjects were, in most cases, within a normal range; however, there were six (10%) cases of pregnant women with a concentration higher than the level recommended by the EPA (5.8 µg/L), which was also slightly higher than results from a USA survey (8 vs 10%).8 Among the six cases in which blood mercury levels were higher than the recommended concentration, four cases involved fish consumption more than 12 times per month. Follow-up blood mercury levels were decreased in the study group, and, thus, fish consumption was positively correlated with blood mercury level. This finding was likely influenced by prior maternal methyl mercury exposure. Among those with increased follow-up blood mercury levels, two women consumed more fish than usual due to antepartum anemia.
The maternal blood mercury level in late pregnancy was positively correlated with the cord blood level, which is consistent with previous findings by Vahter et al.11 and Tsuchiya et al.7 The cord blood mercury level was approximately twice as high as the maternal blood mercury levels. This may be due to previous findings indicating that there are relatively higher levels of red blood cells in cord blood and that most of mercury in the blood is found bound to red blood cells, where approximately 90% is slowly metabolized to mercury ions and then excreted into the bile. It has been consistently demonstrated that the blood mercury concentration in the umbilical blood is substantially higher, and this may lead to higher blood mercury levels in neonates born with a high cord blood mercury level. Such exposure may cause impairment of the central nervous system due to mercury poisoning, as the development of the central nerve system is rapid during the neonatal period.
The most limiting factor of our study was the small sample size. In addition to the small sample size, the frequency and amount of food consumption in the questionnaire was very difficult for subjects to generalize. Indeed, some individuals may consider their consumption of fish to be a small quantity and respond to the questionnaire accordingly, when, in reality, they may actually consume a large quantity. The reverse is also true, and, in other cases, while one rarely consumes fish, they may, for example, attend a dinner party and consume a large quantity of tuna sashimi in which the mercury concentration is high. Therefore, to more accurately assess the amount of the consumption of fish and shellfish, a thorough, individual interview with the subject would be required. Because this was not feasible for the present study, such topics were assessed only by a questionnaire, which may be considered problematic. However, it was thought that, in general, the intake amount was high in individuals who frequently consume fish, and, thus, the frequency of consumption was considered as the intake amount.
Based on our results, the blood mercury concentration in pregnant women was associated with the amount of fish intake. Additionally, restricting fish consumption through prenatal education of women of childbearing age and pregnant women can help to lower the blood mercury concentration in pregnant women. Furthermore, such prenatal education may also help to lower the potential impairment of the development of the peripheral and central nervous system of neonates.
In order to protect against mercury poisoning, the establishment of standards for fish consumption, including tuna, for women of childbearing age and pregnant women is required as soon as possible. Until the establishment of such standards, however, one can follow US EPA guidelines, which suggest that one should restrict the total consumption of fish and shellfish to less than 340 mg per week and not eat shark, swordfish, king markel, or tilefish, which have high mercury content. Lastly, a future, large-scale study that selects the control group and the study group by a more accurate method is warranted.
Figures and Tables
References
1. Lee KN, Kwon OH. VIII Heavy Metal. Clinical Pathology File. 2003. 3rd ed. Seoul: Publishing Company Medical Culture;484–486.
2. Amin-Zaki L, Elhassani S, Majeed MA, Clarkson TW, Doherty RA, Greenwood M. Intra-uterine methylmercury poisoning in Iraq. Pediatrics. 1974. 54:587–595.
3. US Environmental Protection Agency. Publication EPA-452/R-97-003. Mercury Study Report to Congress, Volume I: Executive Summary. 1997. Washington, DC: Environmental Protection Agency.
4. Myers GJ, Davidson PW, Cox C, Shamlaye CF, Palumbo D, Cernichiari E, et al. Prenatal methylmercury exposure from ocean fish consumption in the Seychelles child development study. Lancet. 2003. 361:1686–1692.
5. Grandjean P, White RF, Weihe P, Jorgensen PJ. Neurotoxic risk caused by stable and variable exposure to methylmercury from seafood. Ambul Pediatr. 2003. 3:18–23.
6. Yamamura Y, Yoshinaga Y, Arai F, Kishimoto T. Background levels of total mercury concentrations in blood and urine. Sangyo Igaku. 1994. 36:66–69.
7. Tsuchiya H, Mitani K, Kodama K, Nakata T. Placental transfer of heavy metals in normal pregnant Japanese women. Arch Environ Health. 1984. 39:11–17.
8. Schober SE, Sinks TH, Jones RL, Bolger PM, McDowell M, Osererloh J, et al. Blood mercury levels in US children and women of childbearing age 1999-2000. JAMA. 2003. 289:1667–1674.
9. Grandjean P, Weihe P, White RF, Debes F, Araki S, Yokoyama K, et al. Cognitive deficit in 7-year-old children with prenatal exposure to methylmercury. Neurotoxicol Teratol. 1997. 19:417–428.
10. Davidson PW, Myers GJ, Cox C, Axtell C, Shamlaye C, Sloane-Reeves J, et al. Effects of prenatal and postnatal methylmercury exposure form fish consumption on neurodevelopment: outcomes at 66 months of age in the Seychelles Child Development Study. JAMA. 1998. 280:701–707.
11. Vahter M, Akesson A, Lind B, Bjors U, Schutz A, Berglund M. Longitudinal study of methylmercury and inorganic mercury in blood and urine of pregnant and lactating women, as well as in umbilical cord blood. Environ Res. 2000. 84:186–194.
12. 2004 EPA and FDA Advice For: Women who might become pregnant, women who are pregnant, nursing mothers, young children. What you need to know about mercury in fish and shellfish: Food and Drug Administration. 2004. 03. Available from: URL: http://www.cfsan.fda.gov/~dms/admehg3.html.
13. Consumer advisory: An important message for pregnant women and women of childbearing age who may become pregnant about the risks of mercury in fish. Food and Drug Administration. 2001. Washington: FDA;Available from: URL: http://www.cfsan.fda.gov/~lrd/tphgfish.html.
14. Food safety facts on mercury and fish consumption. Canada Food Inspection Fact Sheet. Available from: URL: http://www.inspection.gc.ca/english/corpaffr/foodfacts/mercurye.shtml.
15. Agency updates advice to pregnant and breastfeeding women on eating certain fish. Food Standards Agency. Available from: URL: http://www.foodstandards.gov.uk/news/pressreleases/tuna_mercury.
16. Environment Health Criteria 101. Methylmercury. 1990. Geneva: World Health Organization.
17. Behrman RE, Kliegman R, Jenson HB. Heavy metal intoxification. Nelson Textbook of Pediatrics. 2004. 17th ed. Elsevier Science Saunders;702–703.
18. Olsen SF, Secher NJ. Low consumption of seafood in early pregnancy as a risk factor for preterm delivery: prospective cohort study. BMJ. 2002. 324:447.
19. Olsen SF, Grandjean P, Weihe P, Videro T. Frequency of seafood intake in pregnancy as a determinant of birth weight: evidence for a dose dependent relationship. J Epidemiol Community Health. 1993. 47:436–440.
20. Hu FB, Bronner L, Willett WC, Stampfer MJ, Rexrode KM, Albert CM, et al. Fish and omega-3 fatty acid intake and risk of coronary heart disease in women. JAMA. 2002. 287:1815–1821.
21. Guallar E, Sanz-Gallardo MI, van't Veer P, Bode P, Aro A, Gomez-Aracena J, et al. Mercury, fish oils, and the risk of myocardial infarction. N Engl J Med. 2002. 347:1747–1754.
22. An official telegram of food: Common standard about general food. Korea Food & Drug Administration. Available from: URL: http://www.kfda.go.kr.
23. Test on total meucury in fishes in Korea 2004. Consumer Korea. Available from: URL: http://www.cacpk.org.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download