Abstract
Increasing evidence suggests an association between elevated serum aminotransferase level and the metabolic syndrome. However, the significance of relatively low levels of aminotransferase in relation to the metabolic syndrome has not been fully investigated in the general population. We investigated the association between serum amiontransferase level and the metabolic syndrome using data from a nationwide survey in Korea. We measured serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels and metabolic conditions among 9771 participants aged 20 or more in the 1998 and 2001 Korean National Health and Nutrition Examination Surveys. Metabolic syndrome was defined according to NCEP-ATP III criteria with a modified waist circumference cutoff (men > 90 cm; women > 80 cm). Serum aminotransferase level, even within normal range, was associated with the metabolic syndrome independent of age, body mass index, waist circumference, smoking, and alcohol intake. Compared with the lowest level (< 20 IU/L), the adjusted odds ratios (95% CI) for an AST level of 20-29, 30-39, 40-49 and ≥ 50 IU/L were 1.10 (0.85-1.42), 1.37 (1.02-1.83), 1.62 (1.08-2.43), and 2.25 (1.47-3.44) in men, and 1.18 (0.99-1.41), 1.43 (1.29-1.83), 1.71 (1.09-2.68), and 2.14 (1.20-3.80) in women, respectively. Corresponding odds ratios for ALT levels were 1.27 (0.99-1.63), 1.69 (1.28-2.23), 2.17 (1.58-2.99), and 2.65 (1.96-3.58) in men, and 1.44 (1.22-1.70), 1.65 (1.26-2.15), 2.94 (1.93-4.47), and 2.25 (1.54-3.30) in women, respectively. In conclusion, elevated serum aminotransferase levels, even in the normal to near normal range, are associated with features of the metabolic syndrome.
Non-alcoholic fatty liver disease (NAFLD) is an increasingly recognized condition that has accompanied the recent increase in obesity.1-3 and is also known to be associated with various cardiovascular risk factors including central obesity, type 2 diabetes, dyslipidemia, and high blood pressure.2,4-9 Moreover, it has been suggested that NAFLD can be considered a hepatic consequence of the metabolic syndrome.10-14 Patients with fatty liver disease usually have elevated serum aminotransferase activity, and so aminotransferase assays are widely used to monitor liver function in people with metabolic syndrome.1,2 It has been suggested, however, that the use of current definitions of normal serum aminotransferase levels may underestimate the prevalence of liver disease, because normal aminotransferase levels cannot rule out the existence of liver disease.15-17 The significance of serum amiontransferase level, including within the normal to near normal range, needs to be reviewed in relation to the metabolic syndrome, and the need for a full investigation in the general population still remains. Accordingly, we investigated the independent association between serum aminotransferase level and the metabolic syndrome in a representative Korean population.
The Korean National Health and Nutrition Examination Surveys were conducted in non-institutionalized Korean civilians in 1998 and 2001. A stratified multistage probability sampling design was used, with selection made from sampling units based on geographical area, sex, and age groups using household registries. A total of 13,451 individuals (7945 in 1998 and 5506 in 2001) aged 20 years or more completed the health examinations. Among them, 11,282 people fasted for at least eight hours before their blood samples were obtained. We excluded 549 people who tested positive for Hepatitis B (HBsAg), and 95 pregnant women. We also excluded 389 people who reported consuming at least 50 g of alcohol per day. In the end, 9771 people (4019 men and 5752 women) were eligible for our analyses.
Anthropometric measurements including height, weight, and waist and hip circumference were conducted by well-trained examiners on individuals wearing light clothing. Waist circumference was measured to the nearest 0.1 cm at the midpoint between the lower borders of the rib cage and the iliac crest. A standard mercury sphygmomanometer was used to measure the blood pressure of each individual in a sitting position after a 10-minute rest period. Systolic and diastolic blood pressures were measured at phase I and V Korotkoff sounds, respectively. Two readings of systolic and diastolic blood pressure were recorded and the average was used for data analysis. Blood samples were obtained after an overnight fasting period and subsequently analyzed at a central certified laboratory. Serum glucose, total cholesterol, triglyceride, high density lipoprotein (HDL)-cholesterol, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) levels were measured by an autoanalyzer (Hitachi 747, Tokyo, Japan). Smoking and alcohol consumption habits and current medication status were determined by a self-administered questionnaire. Non-drinkers were people who reported that they never or almost never (less than once a month) consumed alcoholic beverages. For drinkers, daily alcohol intake was calculated by multiplying the frequency of drinking and the amount consumed in one sitting.
The metabolic syndrome was defined according to the National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III), except for abdominal obesity by waist circumference.18 We used a modified waist circumference cutoff of > 90 cm in men and > 80 cm in women.19 Hence, in the present study, individuals having three or more of the five following criteria were defined as having the metabolic syndrome: 1) high blood pressure (≥ 130/85 mmHg) or anti-hypertensive medication, 2) elevated fasting blood glucose (≥ 6.1 mmol/L) or anti-diabetic medication, 3) hypertriglyceridemia (≥ 1.7 mmol/L), 4) low HDL-cholesterol (men, < 1.0 mmol/L; women, < 1.3 mmol/L), and 5) abdominal obesity by waist circumference (men, > 90 cm; women, > 80 cm).
We compared clinical and biochemical characteristics between men and women using student's t-test or χ2 test. Spearman correlation coefficients among the metabolic risk factors and aminotransferase levels were calculated in men and women separately. The sex-specific prevalence of abnormal metabolic conditions and the metabolic syndrome were calculated by the level of AST and ALT. Independent association between serum aminotransferase level and the metabolic syndrome was investigated using serial logistic regression models. First, we estimated the age-adjusted odds ratio for the metabolic syndrome by serum aminotransferase levels. Second, we adjusted for age, body mass index, cigarette smoking and alcohol intake. Finally, waist circumferences were adjusted in addition to all of the variables in the second model. In order to assess the possible confounding effects of alcohol intake, we investigated the association between ALT and the metabolic syndrome by drinking status.
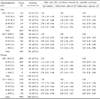
Clinical characteristics and laboratory data of the 4019 men and 5752 women are shown in Table 1. Mean age was 44.7 years for men and 45.6 years for women (p = 0.009), but mean body mass index was the same for both sexes. Compared with women, men had higher waist circumference, blood pressure, fasting glucose, triglyceride, AST and ALT levels, but lower HDL-cholesterol levels. Among the study participants, 6.6% were taking anti-hypertensive medications, and 2.6% were taking anti-diabetic medications. Of men, 61.5% were current smokers, as were 5.7% of women. Regular alcohol drinkers comprised 64.8% of men and 28.1% of women.
Serum aminotransferase levels were correlated with most metabolic risk factors, except there was no association (p = 0.982) between AST level and HDL-cholesterol level in women. Compared to AST level, serum ALT level was more closely associated with body mass index, waist circumference, and fasting blood glucose level (Table 2). Prevalence of central obesity, high blood pressure, high fasting blood glucose, and hypertriglyceridemia increased according to the increase of serum AST level. The prevalence of low serum HDL-cholesterol was negatively associated with AST level in men, but not in women. On the contrary, serum ALT level was positively associated with all five metabolic abnormalities in both sexes (Table 3).
Age-adjusted odds ratios for the metabolic syndrome increased progressively according to serum aminotransferase levels. The positive association between aminotransferase level and the metabolic syndrome was observed even within the normal range of aminotransferase levels. When adjusted for age, body mass index, smoking and alcohol intake, the association between aminotransferase level and metabolic syndrome was attenuated but still highly significant. Even after additional adjustment for waist circumference, the association between aminotransferase level and metabolic syndrome still remained (Table 4). We assessed the association between ALT and the metabolic syndrome in non-drinkers and drinkers separately. The positive association between serum ALT level and the metabolic syndrome was not different by alcohol intake (Fig. 1).
In a further analysis, we compared the relative significance of individual liver enzymes by including AST and ALT in the same model. In that model, the metabolic syndrome was significantly associated only with ALT level (p < 0.001 for both sexes), but not with AST level (p = 0.272 for men and 0.240 for women).
We found a positive association between serum aminotransferase level and the metabolic syndrome in Korean adults. Recent epidemiologic studies have also reported an association between aminotransferase elevation and the metabolic syndrome.20-30 This association has been observed in various populations, including obese people,26,27 elderly men,28 postmenopausal women,29 and even adolescents.30 Although similar findings have already been reported in some Korean populations,22,29,30 the present study showed a significant association between aminotransferase level and the metabolic syndrome in a nationally representative Korean population. Another more important finding of this study is that the association was observed even in the normal to near normal range of aminotransferase levels, in a dose-related manner.
The most probable explanation for the association between serum aminotransferase level and the metabolic syndrome is NAFLD. NAFLD is the most common cause of unexplained aminotransferase elevations in Western populations, and even in some Asian populations.2,31 A growing body of evidence supports an association between NAFLD and the metabolic syndrome.3,7,10-14,30-35 Recent studies have added evidence that insulin resistance, a key component of the metabolic syndrome, may contribute to the development of NAFLD.7,13,36,37 Central obesity may be an underlying cause of insulin resistance and can also contribute to the development of NAFLD.11,37-39 Compared with adipose tissue in other sites, visceral adipose tissue is more resistant to insulin, and the associated relative hyperinsulinemia promotes lipogenesis in the liver.40,41 Visceral adipose tissue is also known to be a potent modulator of insulin action on hepatic glucose production and gene expression.42 In the present study, serum aminotransferase levels had a dose-related association with metabolic syndrome even after adjustment for body mass index and waist circumference. The significance of central obesity in the connection between liver dysfunction and the metabolic syndrome may differ by ethnicity, as differences in the adverse effects of obesity between different ethnicities have been reported.43,44 Further studies are required to investigate ethnic and regional differences in the relationship between liver disease and the metabolic syndrome.
Other conditions which can increase aminotransferase activity may also be associated with the metabolic syndrome.31 The serum aminotransferase assay is a sensitive screening tool for the detection of liver disease, but it cannot provide information on the underlying causes of liver damage. Alcohol-related liver disease can be associated with the metabolic syndrome. Heavy drinkers tend to have an adverse cardiovascular risk profile, including high blood pressure, central obesity, and unhealthy lifestyle. We did not include current heavy drinkers for the analysis, and past history of alcohol consumption was also not considered. We could not exclude other causes of aminotransferase elevation, such as C-viral hepatitis and iron overload. It is unlikely that other causes of liver disease severely affected the relationship between aminotransferase levels and the metabolic syndrome. A recent study found that the association between metabolic risk factors and ALT elevation was similar in subjects with and without identifiable causes of chronic liver disease, including viral hepatitis, excessive alcohol use, and increased iron saturation.45 Some systemic diseases and medications may also elevate serum aminotransferase levels. Accordingly, we performed further analysis after excluding 963 people who were receiving hormone replacement therapy or medications for hypertension, diabetes mellitus, liver disease, and/or renal disease during the month before examinations. We still found a strong association between serum aminotransferase level and the metabolic syndrome, even in the normal to near normal range of aminotransferase. Compared with levels below 20 IU/L, the adjusted odds ratios for an ALT level of 20-29, 30-39, 40-49 and ≥ 50 IU/L were 1.38, 1.76, 2.24 and 3.01 in men and 1.49, 1.73, 3.05 and 2.40 in women, respectively (p < 0.05 for all). These results demonstrate that other causes of aminotransferase elevations did not alter the outcomes of this study.
In the present study, serum ALT level was more closely associated with the metabolic syndrome than AST level. In addition to that, only ALT level was significantly associated with the metabolic syndrome when both enzymes were simultaneously investigated in a single model. This finding is in agreement with previous studies, and can be explained by higher specificity of ALT to liver disease.
Serum aminotransferase assays have been widely used to identify NAFLD and other liver diseases. But the cutoff level that discriminates between healthy and diseased livers has not been clearly defined. The upper normal limit of serum aminotransferase is set on average at 40 IU/L, ranging from 30-50 IU/L.17,46 However, this normal range was calculated from a supposedly healthy reference population, which probably included people with mild to moderate chronic liver disease. Several previous studies have demonstrated that serum aminotransferase level, even within the normal range, may be associated with morbidity and mortality.15-17,22,29,47 The progressive linear association between serum aminotransferase level and the metabolic syndrome suggests that people with high normal aminotransferase levels may need further investigation for the presence of fatty liver disease. Adjustment of the normal limit of serum amiontransferase should be considered for the monitoring of liver function in people with the metabolic syndrome. In most Western regions, the aminotransferase assay has been less useful as a mass-screening tool, because the prevalence of liver disease is lower than in East Asian or African countries. However, considering the increasing prevalence of the metabolic syndrome and its association with liver dysfunction, the significance of the serum aminotransferase assay needs to be reevaluated.
The present study also has several possible limitations. First, we had only one measurement of aminotransferase. Aminotransferase activity is a sensitive marker of liver dysfunction, but its specificity in detection of liver diseases is low because it can be elevated temporarily in various conditions. This limitation would serve to attenuate the magnitude of the association toward the null; thus, our results can probably be considered as conservative estimates. Second, there is the possibility of confounding effects by viral and alcoholic liver diseases. We excluded people who were positive for HBsAg, but could not rule out the effects of other types of viral hepatitis. We did not include heavy drinkers in the analysis and statistically controlled the effects of alcohol consumption, but the possibility of residual confounding influence still exists. Finally, this study could not investigate the causal relationship between serum aminotransferase levels and the metabolic syndrome because of its cross-sectional design. Further prospective studies are needed to establish the temporal relationship between aminotransferase level and the metabolic syndrome, and to discover the underlying mechanism of the relationship.
In conclusion, serum aminotransferase levels even in the normal or near normal range are associated with features of the metabolic syndrome in Korean men and women.
Figures and Tables
Fig. 1
Association between serum alanine aminotransferase level and metabolic syndrome by alcohol drinking status. Odds ratios with 95% confidence intervals (vertical lines) are adjusted for age, body mass index, waist circumference, and smoking status.

Table 2
Correlation Among Metabolic Risk Factors and Serum Aminotransferase Levels

Figures are Spearman correlation coefficients for men in the upper right of the table, for women in the lower left of the table.
BMI, body mass index; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; HDL, high density lipoprotein; FBS, fasting blood sugar; AST, aspartate aminotransferase; ALT, alanine aminotransferase.
All correlations were significant with p < 0.001, except for *p = 0.077; †p = 0.954; ‡p = 0.004; §p = 0.928.
ACKNOWLEDGEMENTS
We thank the members of the Korea Institute for Health and Social Affairs who contributed the Korean National Health and Nutritional Examination surveys.
References
1. James OF, Day CP. Non-alcoholic steatohepatitis (NASH): a disease of emerging identity and importance. J Hepatol. 1998. 29:495–501.
2. Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002. 346:1221–1231.
3. Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003. 37:917–923.
4. Wanless I, Lentz J. Fatty liver hepatitis (steatohepatitis) and obesity: an autopsy study with analysis of risk factors. Hepatology. 1990. 12:1106–1110.
5. Luyckx FH, Lefebvre PJ, Scheen AJ. Non-alcoholic steatohepatitis: association with obesity and insulin resistance, and influence of weight loss. Diabetes Metab. 2000. 26:98–106.
6. Bellentani S, Saccoccio G, Masutti F, Croce LS, Brandi G, Sasso B, et al. Prevalence and risk factors for hepatic steatosis in northern Italy. Ann Intern Med. 2000. 132:112–117.
7. Chitturi S, Abeygunasekera S, Farrell GC, Holmes-Walker J, Hui JM, Fung C, et al. NASH and insulin resistance: Insulin hypersecretion and specific association with the insulin resistance syndrome. Hepatology. 2002. 35:373–379.
8. Loguercio C, De Girolamo V, de Sio I, Tuccillo C, Ascione A, Baldi F, et al. Non-alcoholic fatty liver disease in an area of southern Italy: main clinical, histological and pathophysiological aspects. J Hepatol. 2001. 35:568–574.
9. Dixon JB, Bhathal PS, O'Brien PE. Non-alcoholic fatty liver disease: predictors of non-alcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology. 2001. 121:91–100.
10. Angelico F, Del Ben M, Conti R, Francioso S, Feole K, Maccioni D, et al. Non-alcoholic fatty liver syndrome: a hepatic consequence of common metabolic diseases. J Gastroenterol Hepatol. 2003. 18:588–594.
11. Cortez-Pinto H, Camilo ME, Baptista A, De Oliveira AG, De Moura MC. Non-alcoholic fatty liver: another feature of the metabolic syndrome? Clin Nutr. 1999. 18:353–358.
12. Marceau P, Biron S, Hould FS, Marceau S, Simard S, Thung SN, et al. Liver pathology and the metabolic syndrome X in severe obesity. J Clin Endocrinol Metab. 1999. 84:1513–1517.
13. Pagano G, Pacini G, Musso G, Gambino R, Mecca F, Depetris N, et al. Non-alcoholic steatohepatitis, insulin resistance and metabolic syndrome; futher evidence for and etiological association. Hepatology. 2002. 35:367–372.
14. Marchesini G, Forlani G. NASH: form liver diseases to metabolic disorders and back to clinical hepatology. Hepatology. 2002. 35:497–498.
15. Prati D, Taioli E, Zanella A, Della Tores E, Butelli S, Del Vecchio E, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med. 2002. 137:1–9.
16. Mofrad P, Contos MJ, Haque M, Sargeant C, Fisher RA, Luketic VA, et al. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology. 2003. 37:1286–1292.
17. Kim HC, Nam CM, Jee SH, Han KH, Oh DK, Suh I. Normal serum aminotransferase concentration and risk of mortality from liver diseases: prospective cohort study. BMJ. 2004. 328:983–986.
18. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001. 285:2486–2497.
19. WHO/IASO/IOTF. The Asia-Pacific perspective: redefining obesity and its treatment. 2000. Melbourne: Health Communications Australia.
20. Liangpunsakul S, Chalasani N. Unexplained elevations in alanine aminotransferase in individuals with the metabolic syndrome: results from the third National Health and Nutrition Survey (NHANES III). Am J Med Sci. 2005. 329:111–116.
21. Hanley AJ, Williams K, Festa A, Wagenknecht LE, D'Agostino RB Jr, Haffner SM. Liver markers and development of the metabolic syndrome: the insulin resistance atherosclerosis study. Diabetes. 2005. 54:3140–3147.
22. Jeong SK, Nam HS, Rhee JA, Shin JH, Kim JM, Cho KH. Metabolic syndrome and ALT: a community study in adult Koreans. Int J Obes Relat Metab Disord. 2004. 28:1033–1038.
23. Nannipieri M, Gonzales C, Baldi S, Posadas R, Williams K, Haffner SM, et al. Mexico City diabetes study. Liver enzymes, the metabolic syndrome, and incident diabetes: the Mexico City diabetes study. Diabetes Care. 2005. 28:1757–1762.
24. Yamada J, Tomiyama H, Yambe M, Koji Y, Motobe K, Shiina K, et al. Elevated serum levels of alanine aminotransferase and gamma glutamyltransferase are markers of inflammation and oxidative stress independent of the metabolic syndrome. Atherosclerosis. 2006. 01. 04. [Epub ahead of print].
25. Shen YH, Yang WS, Lee TH, Lee LT, Chen CY, Huang KC. Bright liver and alanine aminotransferase are associated with metabolic syndrome in adults. Obes Res. 2005. 13:1238–1245.
26. Finelli C, Conca P, Contaldo F, Pasanisi F. Non-alcoholic fatty liver disease in young adult severely obese non-diabetic patients in South Italy. Ann Nutr Metab. 2005. 49:289–295.
27. Marchesini G, Avagnina S, Barantani EG, Ciccarone AM, Corica F, Dall'Aglio E, Dalle Grave R, Morpurgo PS, Tomasi F, Vitacolonna E. Aminotransferase and gamma-glutamyltranspeptidase levels in obesity are associated with insulin resistance and the metabolic syndrome. J Endocrinol Invest. 2005. 28:333–339.
28. Wannamethee SG, Shaper AG, Lennon L, Whincup PH. Hepatic enzymes, the metabolic syndrome, and the risk of type 2 diabetes in older men. Diabetes Care. 2005. 28:2913–2918.
29. Choi KM, Lee KW, Kim HY, Seo JA, Kim SG, Kim NH, Choi DS, Baik SH. Association among serum ferritin, alanine aminotransferase levels, and metabolic syndrome in Korean postmenopausal women. Metabolism. 2005. 54:1510–1514.
30. Park HS, Han JH, Choi KM, Kim SM. Relation between elevated serum alanine aminotransferase and metabolic syndrome in Korean adolescents. Am J Clin Nutr. 2005. 82:1046–1051.
31. Clark JM, Brancati FL, Diehl AM. The prevalence and etiology of elevated aminotransterase levels in the United States. Am J Gastroenterol. 2003. 98:960–967.
32. Marchsini G, Brizi M, Morselli-Labate AM, Bianchi G, Bugianesi E, McCullough AJ, et al. Association of nonalcoholic fatty liver disease with insulin resistance. Am J Med. 1999. 107:450–455.
33. Knobler H, Schattner A, Zhornicki T, Malnick SD, Keter D, Sokolovskaya N, et al. Fatty liver-an additional and treatable feature of the insulin resistance syndrome. Q J Med. 1999. 92:73–79.
34. Kelley DE, McKolanis TM, Hegazi RA, Kuller LH, Kalhan SC. Fatty liver in type 2 diabetes mellitus: relation to regional adiposity, fatty acids, and insulin resistance. Am J Physiol Endocrinol Metab. 2003. 285:E906–E916.
35. Sattar N, Scherbakova O, Ford I, O'Reilly DS, Stanley A, Forrest E, et al. Elevated alanine aminotransferase predicts new-onset type 2 diabetes independently of classical risk factors, metabolic syndrome, and C-reactive protein in the west of Scotland coronary prevention study. Diabetes. 2004. 53:2855–2860.
36. Lee JH, Rhee PL, Lee JK, Lee KT, Kim JJ, Koh KC, et al. Role of hyerinsulinemia and glucose intolerance in the pathogenesis of nonalcoholic fatty liver in patients with normal body weight. Korean J Intern Med. 1998. 13:12–14.
37. Marchesini G, Brizi M, Bianchi G, Tomassetti S, Bugianesi E, Lenzi M, et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes. 2001. 50:1844–1850.
38. Omagari K, Kadokawa Y, Masuda J, Egawa I, Sawa T, Hazama H, et al. Fatty liver in non-alcoholic non-overweight Japanase adults: incidence and clinical characteristics. J Gastroenterol Hepatol. 2002. 17:1098–1105.
39. Farrell GC. Non-alcoholic steatohepatitis: what is it, and why is it important in the Asia-Pacific region? J Gastroenterol Hepatol. 2003. 18:124–138.
40. Kissebah AH, Krakower GR. Regional adiposity and morbidity. Physiol Rev. 1994. 74:761–811.
41. Haque M, Sanyal AJ. The metabolic abnormalities associated with non-alcoholic fatty liver disease. Best Pract Res Clin Gastroenterol. 2002. 16:709–731.
42. Barzilai N, She L, Liu BQ, Vuguin P, Cohen P, Wang J, et al. Surgical removal of visceral fat reverses hepatic insulin resistance. Diabetes. 1999. 48:94–98.
43. Wang J, Thornton JC, Russell M, Burastero S, Heymsfield S, Pierson RN Jr. Asians have lower body mass index (BMI) but higher percent body fat than do whites: comparisons of anthropometric measurements. Am J Clin Nutr. 1994. 60:23–28.
44. Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002. 3:141–146.
45. Ioannou GN, Weiss NS, Boyko EJ, Kahn SE, Lee SP. Contribution of metabolic factors to alanine aminotransferase activity in persons with other causes of liver disease. Gastroenterology. 2005. 128:627–635.
46. Sherman KE. Alanine aminotransferase in clinical practice. A review. Arch Intern Med. 1991. 151:260–265.
47. Mathiesen UL, Franzen LE, Fryden A, Foberg U, Bodemar G. The clinical significance of slightly to moderately increased liver transaminase values in asymptomatic patients. Scand J Gastroenterol. 1999. 34:85–91.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download