Abstract
By analyzing the data of 459 patients who completed the Supportive Care Needs Survey (SCNS), the prevalence, medical and non-medical predictors of unmet needs were investigated. Breast cancer patients in Korea experienced high levels of unmet needs across the needs domains, particularly in the health system and information domain (56.9%). Various medical and non-medical variables were identified as significant predictors of unmet needs in each domain. By multivariate analyses, several predictors were identified across the domains including; less education (≤ 9 years) in the psychologic, chemotherapy, short post-surgical interval, and less education in the physical and daily living, younger age (< 50 years) in the sexuality, larger tumor size (> 2 cm) and younger age in the health system and information, and more education (≥ 13 years) in the care and support domain. The results of this study suggest medical professional should consider the complexity and dynamics of meeting patients' needs in providing supportive care services.
Breast cancer has been increasing in Korea and is the most common type of cancer among women since year 2001 (16.1%). The crude incidence rate of breast cancer in 2002 was 31.4 per 100,000 women and 7,551 new cases were diagnosed in 2001.1 The incidence increased twice over 7 years, exceeding the world-wide annual increasing rate of 2%. Even though the incidence is still quite low compared with those in western countries, breast cancer is expected to keep increasing, considering westernizing life style, rapidly decreasing birth rate and breast feeding, and increasing concern for breast cancer with regular breast check ups.
The age distribution of breast cancer in Korea differs from that of western countries. The proportion of premenopausal breast cancer patients is 59.2% and the prevalence in terms of age is the highest in 40s (40.0%) followed by 50s (24.6%) and 30s (17.0%).1 Previous studies have demonstrated that a breast cancer diagnosis generates more anxiety than any other cancer.2 Moreover, Younger women with breast cancer could experience more distress associated with a life-threatening diagnosis and future health, as well as fears of potential disfigurement, disability and distress.3 Although the high psychosocial morbidity of breast cancer has been well studied,4-6 little research has been done addressing the concerns or the unmet needs that persist for breast cancer patients in Korea. Quality of life or psychosocial morbidity of breast cancer patients just began to be considered as an important aspect of cancer care in Korea.
In order to estimate the morbidity in cancer patients, quality of life assessment, satisfaction with care, and patients' needs assessment have been in use, and the relative strengths of needs assessment have been well documented.7 Needs assessment helps to identify specific issues or areas where patients require the most help. Also those patients with higher levels of need can be identified and then specifically targeted with appropriate early interventions and health services.7
According to several studies about satisfaction with care,8-10 breast cancer patients are less satisfied with the information received than with the clinical aspects of care. Also high levels of unmet needs were reported in the information area11-13 and the psychologic area.7
Even though breast cancer has become the most frequent type of cancer among women and the incidence is still increasing in Korea, there has not been any research about what kind of needs patients have or which patient group has higher need for help.
The purpose of this study was to assess the prevalence of unmet supportive needs among breast cancer patients after surgery, to determine the social and medical predictors of those needs in Korea and to compare this with other studies.
The subjects were randomly selected from breast cancer outpatients, who had surgery between June 1988 and August 2002 and were visiting the hospital for regular follow-up at Yonsei University Severance Hospital, Seoul, Korea. Eligibility criteria for the survey were ages between 20 and 80 years old and having been diagnosed with breast cancer and treated surgically. Patients with severe mental disorders or judged too ill to participate were excluded.
Eligible subjects were informed about the study at their outpatient visits by a member of the research team. They were provided written information about the study. Patients were told that participation in the study was entirely voluntary and the care they receive would not be affected by their decision whether they participate or not. Patients who provided informed consent to participate were given a questionnaire, SCNS, and asked to complete the survey in their waiting room. Present study started on November 2002 and ended on April 2003.
Socio-demographic background including patient's age, marital status, duration of marriage, income, children, people living with, education, and job were included in the questionnaire. Medical variables were collected by reviewing the patients' medical records.
SCNS,14 a modified version of the Cancer Needs Questionnaire (CNQ),11 was used to assess the unmet supportive care needs of breast cancer patients. It was designed to provide a direct and comprehensive assessment of the multidimensional impact of cancer on the lives of cancer patients.7 Since the SCNS includes issues about sexuality, it is considered to have more relevance for breast cancer patients than the CNQ. The survey's psychometric properties and the reliability and validity of this measure have been well documented.14
In this study, SCNS was translated in Korean language and the term 'cancer' was substituted by 'breast cancer'. It was pre-tested with a convenience sample of 20 patients who met the selection criteria. After completing the questionnaires, they were asked to evaluate the questionnaires in terms of comprehensibility and relevance of the instrument. As a result, a few items were modified to improve comprehension. It took about 15 to 20 minutes to complete the survey. Face validity was confirmed by 3 other medical professionals, two oncologists and an oncologic social worker. The overall reliability coefficient (Cronbach alpha) was 0.9649 in this study.
Basically, need items were composed of five needs domains7: psychologic, health system and information, physical and daily living, patient care and support, and sexuality. Each item of the questionnaire was asked, "In the last month, what was your level of need for help with...?" with rating scales of 1 to 5, ranging from "No need, not applicable", "No need, satisfied", "Low need", "Moderate need", to "High need". For statistical analysis, "No need, not applicable", "No need, satisfied", were given score 0, "Low need" 1, "Moderate need" 2, and "High need" 3, then total score of each domain was denominated by the number of items to get a mean score. It was defined as 'having needs (some needs)' if the mean score of the domain was greater than 1.
Descriptive statistics were generated for the social and medical background of the patient sample. The overall prevalence of perceived unmet needs was presented by calculating frequency of each response option of all items. Then, in order to examine the relative significance of the social and medical variables on each domain, univariate analysis of each variable was assessed by chi-square test. Finally, multivariate relationships among each independent variable were examined by forward logistic regression analysis. A p-value less than 0.05 was considered statistically significant.
Of 537 eligible patients, 487 (90.7%) consented to participate and returned the survey. Of 487 returned surveys, 28 were not complete and 459 surveys (94.3%) were used as appropriate for statistical analysis.
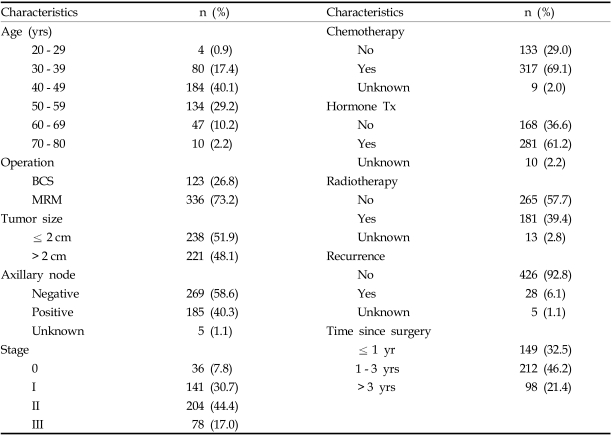
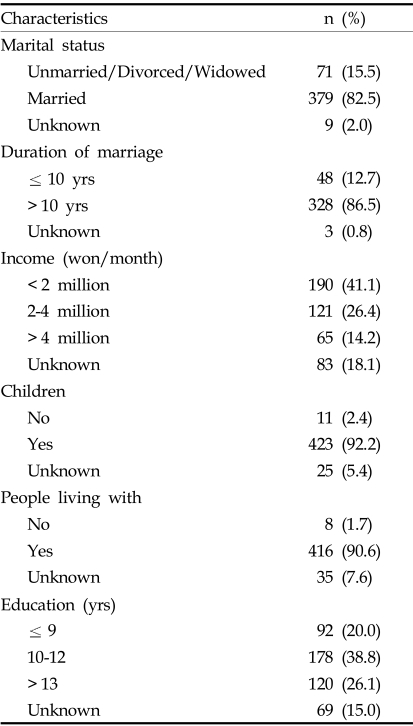
The demographic and medical characteristics of the patients are shown in Table 1 and 2. Since immediate reconstruction after total mastectomy was not popular, only 17 patients (5.0%) of 336 patients with total mastectomy received immediate reconstruction. The age distribution and medical characteristics of the sample patients are almost similar to those from the nationwide Korean Breast Cancer data.1
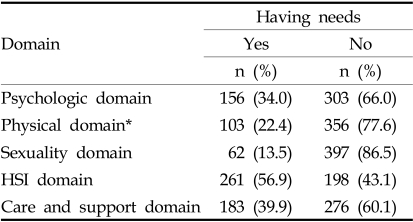
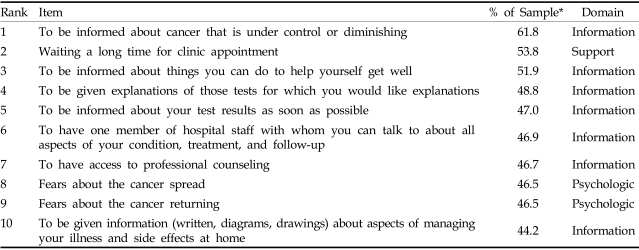
As shown in Table 3, patients had the greatest needs in the health system and information domain (56.9%) followed by the patient care and support (39.9%) and the psychologic domain (34.0%). The frequency of each response options of the 59 items was generated. The 10 items with the highest frequency of moderate to high needs for help are indicated in Table 4. Of the 10 highest needs items, 7 were related to health system and information needs domain, 2 were related to psychologic needs domain and 1 was related to patient care and support needs domain. As shown in Table 4, the overall percentages of ten highest needs were relatively high (44.2-61.8%).
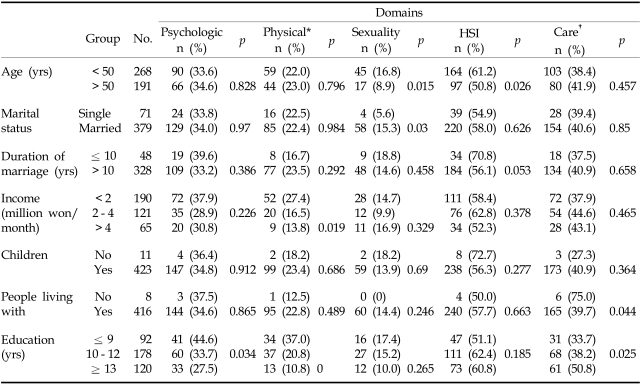
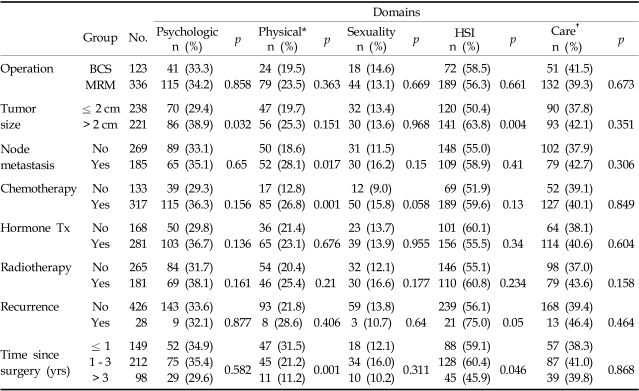
The results of univariate analysis of the social and medical variables according to each of the 5 domains are as follows (Table 5 and 6).
Lower level of education (≤ 9 years) (p = 0.034) and larger tumor size (> 2 cm) (p = 0.032) were found to be significant predictors in this domain.
Patients who had node metastasis were significantly more likely to report some need for help than those who did not (p = 0.017). Patients who were having or already had chemotherapy were more likely to report having need compared with those who did not (p = 0.001). Patients who had surgery more recently (< 1 year) were significantly more likely to report some need compared with those who had surgery more than 3 years ago (p = 0.001). Also, less income(less than 2 million won per month) (p = 0.019) or less education (≤ 9 years) (p < 0.001) were found to be significant predictors in this domain.
Younger patients (< 50) (p = 0.015) and married patients (p = 0.03) were significantly more likely to report having need for help than older patients (≥ 50 years) and singles, respectively.
In this domain, most patients showed a high level of needs. Four variables were identified as significant predictors: larger tumor size (> 2 cm) (p = 0.004), recurrence (p = 0.05), shorter time since surgery (p = 0.046), and younger age (< 50 years) (p = 0.026).
Patients without any people living with them were significantly more likely to report some need for help in the patient care domain compared with patients with any (p = 0.044). More education (> 9 years) significantly predicted reporting needs for help than less education (p = 0.025).
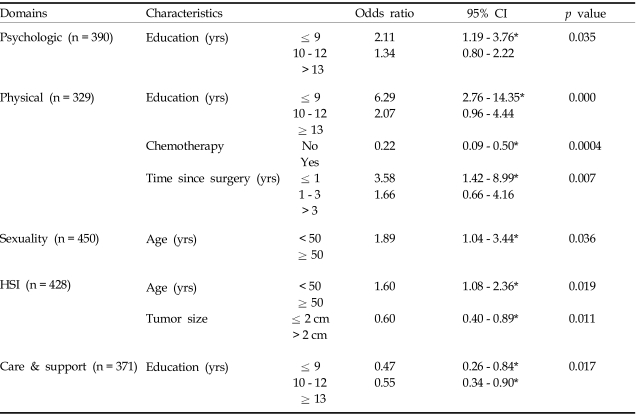
In order to identify the independent significance of each variable according to each domain, medical and social variables were put together in multivariate model.
In multivariate analysis, level of education (p = 0.035) was found to be an independent predictor in the psychologic need domain. Chemotherapy (p = 0.0004), time since surgery (p = 0.007), and education (p < 0.0001) strongly predicted reporting some needs in the physical and daily living domain. In the sexuality domain, age (p = 0.036) was a significant independent predictor. Tumor size (p = 0.011) and age (p = 0.019) were significant predictors in the health system and information domain. In the care and support domain, education (more education) (p = 0.017) was a significant predictor.
This study assessed the overall perceived unmet needs of breast cancer patients and also investigated the predictors of the needs in each domain. The prevalence of perceived unmet needs of participant patients in Korea was higher than those reported in other studies using similar needs assessment instrument.7,11 Also this study showed the highest moderate or high unmet needs were mainly in the health system and information domain, accounting for 7 needs items and the general prevalence of needs according to domain was also the highest in the health system and information domain. This finding is consistent with other studies11-13 which reported high levels of unmet needs in the information area in breast cancer patients. The two psychologic need items among top 10 highest needs items were "fears about the cancer spreading" and "fears about the cancer returning", which are consistent with other studies indicating a major concern of patients with breast cancer is the fear of recurrence.15-18
In univariate analysis for predictors, we expected the operation method would be significant especially in the psychologic and the sexuality domain because it is known that mastectomy has several adverse effects on overall body image and self-esteem.19,20 However, this factor did not differentiate patients' having unmet needs. This may reflect that a woman's persistent issues generally have less to do with the type of surgery received and more to do with her personal and social characteristics and the adjuvant therapy given.2
Tumor size was found to be significant in the psychologic domain and the health and information needs domain. Unlike other medical variables, tumor size is more of a symptom that patients can recognize easily and also by which they judge the severity of the disease. Therefore, the larger the tumor size is the more likely patients are to perceive some unmet psychological needs such as fear of recurrence, uncertainty about future, etc. Also they might have more unmet needs in the information and health system domain in order to find something that they can do.
Among the types of the treatment, patients receiving or having received chemotherapy were more likely to report some needs in the physical and daily living need domain, which is likely due to the side effects of chemotherapy. Node metastasis was also identified as a significant predictor in the physical and daily living domain, which is not surprising. Since most patients with node metastasis have chemotherapy, they might have the same unmet needs in this domain as those who had chemotherapy. This result is also consistent with a previous study.21 Recurrence was highly associated with some need in the health system and information domain. Patients with recurrence worry about the final outcome and may want to learn how to prevent further dissemination.
Patients who had surgery less than 1 year ago were more likely to report some needs in the physical and daily living domain and patients who were in-between 1 to 3 years after surgery were more likely to report some needs in the health system and information domain. This finding may reflect the treatment process that breast cancer patients normally go through; diagnosis, surgery, adjuvant therapy (chemotherapy, radiation therapy, endocrine therapy) and recovery or survivorship. While or until patients have postoperative adjuvant therapy after surgery, they might experience many physical side effects related to the treatments and be more likely to report some needs both in the physical and daily living domain and the information domain. After the treatment is over, patients do not see their physicians as often as they were receiving treatment and also the side effects are alleviated. Therefore, patients who are in-between 1 to 3 years since surgery might need information to manage their illness by themselves and also need professionals or groups of patients to talk with not as patients but more as survivors. Patients who survived longer than 3 years since surgery are moving into a relatively stable stage, therefore they had fewer needs across the domains than those who had surgery less than 3 years ago. This finding suggests more efforts should be devoted specifically that information and physiological care be consistently provided in many different forms as patients move across the disease continuum from diagnosis to treatment to recovery.
Younger age (< 50 years) was highly associated with some need in the sexuality domain and the health system and information domain. This finding is consistent with other studies that cancer and its treatment has a greater psychosocial impact on younger patients.7,11,12,22,23 It can be explained by the different attitudes toward reporting unmet needs between younger and older people7 but previous researches suggest that cancer actually imposes the greater stress and disruption on younger patients.24-27 Although sexuality needs are not discussed openly because of cultural values in Korea, considering the large proportion of premenopausal patients and the high association of younger age and the sexuality needs, health professionals should include sexuality issues as part of their routine care. Marital status makes difference only in the sexuality domain.
"People living with" was found to be a significant predictor in the patient care and support. This finding also supports that unmet need was primarily associated with patients' social support system (eg. children living nearby and perceived resilience of network helpers).21 Low income patients were more likely to report unmet needs in the physical and daily living needs. Low income patients may have limited resources to satisfy daily personal care and physical needs. There are researches indicating the combination of disease and limited financial resources has a cumulative effect on access to health care treatment, which in turn affects patients' health status.21
Education was a significant predictor in many domains but not in the same ways. Generally, education is considered to be highly related to socio-economic status in Korea and patients with less education, like patients with less income, may have limited resources to satisfy their immediate physical and daily living needs than those with more education. Furthermore, they may have more unknown fears because of less access to information about their disease and treatment than those with more education. However, there was a significant association of more education with reporting some unmet need in the patient care and support. This result seems to be contradictory and may not be easily explained. Compared with the items in the physical and daily living need domain, those in the patient care and support domain are not frontline care needs but more of secondary ones such as waiting a long time for clinical appointments, family or friends to be allowed with you in hospital whenever you want, etc. Therefore, it would be possible that patients with more education had their frontline needs satisfied and were more likely to report unmet needs in the patient care and support domain.
In the multivariate model where medical and social variables were put together, many social variables remained independent predictors while several medical variables became insignificant. These may be explained by the concept that medical variables are usually associated with acute phase needs such as those in the physical and daily living domain but the social variables are related to various domains affecting the patients for longer period across the disease continuum. This suggests that the health care teams should pay attention not only to patients' medical characteristics but also to social characteristics in order to provide services appropriately and effectively after surgery.
This study suggests that first of all, medical professionals should give priority to providing appropriate information and be more responsive to the needs of patients to know about their treatment procedures, prognosis, personal care, etc.
Secondly, the supportive care services should include psychologic support, social care and sexuality needs as well as physical or symptomatic support. Also they should be differentiated according to those factors such as education, length of time since surgery, age, etc. For example, for younger patients and patients with lower level of education, psycho-educational group program will be an appropriate option.
To our knowledge, the current study is the first to explore the unmet perceived needs of breast cancer patients in Korea. Also the current study yields the first data set to be accumulated and utilized for comparison between groups and across time, and our findings provide encouragement and a direction for future research in needs assessment. Also more social and medical variables were included than in other need studies and therefore this study results may be able to suggest specific target subgroup according to each need domain.
However, this study has a few limitations. Although this university hospital includes patients from all over the country, those from local area may be underrepresented. Therefore, this result cannot be generalized to all breast cancer patients in Korea. Also, the exact association between education and the unmet needs was not clearly explained. Further research is required including patients from nationwide sample and clarifying the association between the predictors and unmet care needs.
Notes
This work was poster-presented at the 9th St. Gallen Oncology Conferences on January 28, 2005 and was supported by the Brain Korea 21 Project for Medical Science, Yonsei University, and in part by a grant-in-aid from Dong-A Pharmaceutical Co., Ltd., CJ Corporation, and Aventis Pharmaceutical Co, Ltd, Korea.
References
1. The Korean Breast Cancer Society. Nationwide Korean breast cancer data of 2002. J Korean Breast Cancer Soc. 2004; 7:72–83.
2. Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. Prevalence of psychological distress by cancer site. Proc Am Soc Clin Oncol. 1996; 15:507.
3. Rowland JH, Massie MJ. Harris JR, Lippman ME, Morrow M, Osborne CK, editors. Psychosocial issues and interventions. Diseases of the breast. 2000. 2nd ed. Philadelphia: Lippincott Willams & Wilkins;p. 1009–1031.
4. Ganz PA, Coscarelli A, Fred C, Kahn B, Polinsky ML, Petersen L. Breast cancer survivors: psychosocial concerns and quality of life. Breast Cancer Res Treat. 1996; 38:183–199. PMID: 8861837.

5. Walker LG, Eremin O. Psychological assessment and intervention: future prospects for women with breast cancer. Semin Surg Oncol. 1996; 12:76–83. PMID: 8821413.

6. Spiegel D. Psychosocial aspects of breast cancer treatment. Semin Oncol. 1997; 24(1):Suppl 1. S1-36–S1-47. PMID: 9045314.
7. Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P. Supportive Care Review group. The unmet supportive care needs of patients with cancer. Cancer. 2000; 88:226–237. PMID: 10618627.

8. Girgis A, Foot G. Satisfaction with breast cancer care: a summary of the literature, 1984-1994. 1995. Sydney: NHMRC National Breast Cancer Centre.
9. Suominen T. Breast cancer patients' opportunities to participate in their care. Cancer Nurs. 1992; 15:68–72. PMID: 1544135.

10. Tierney AJ, Taylor J, Closs SJ. Knowledge, expectations and experiences of patients receiving chemotherapy for breast cancer. Scand J Caring Sci. 1992; 6:75–80. PMID: 1641535.

11. Foot G, Sanson-Fisher R. Measuring the unmet needs of people living with cancer. Cancer Forum. 1995; 19:131–135.
12. Harrison-Woermke DE, Graydon JE. Perceived informational needs of breast cancer patients receiving radiation therapy after excisional biopsy and axillary node dissection. Cancer Nurs. 1993; 16:449–455. PMID: 8111748.

13. Gustafson DH, Taylor JO, Thompson S, Chesney P. Assessing the needs of breast cancer patients and their families. Qual Manag Health Care. 1993; 2:6–17. PMID: 10131022.

14. Bonevski B, Sanson-Fisher R, Girgis A, Burton L, Cook P, Boyes A. Supportive Care Review Group. Evaluation of an instrument to assess the needs of patients with cancer. Cancer. 2000; 88:217–225. PMID: 10618626.

15. Halttynen A, Hietanen P, Jallinoja P, Lonnqvist J. Getting free of breast cancer. An eight-year perspective of the relapse-free patients. Acta Oncol. 1992; 31:307–310. PMID: 1622650.
16. Fredette SL. Breast cancer survivors: concerns and coping. Cancer Nurs. 1995; 18:35–46. PMID: 7866975.
17. Ferrell BR, Grant MM, Funk BM, Otis-Green SA, Garcia NJ. Quality of life in breast cancer survivors: implications for developing support services. Oncol Nurs Forum. 1998; 25:887–895. PMID: 9644705.
18. Mast ME. Survivors of breast cancer: illness uncertainty, positive reappraisal, and emotional distress. Oncol Nurs Forum. 1998; 25:555–562. PMID: 9568610.
19. Zabora JR. Bland KI, Copeland EM, editors. The Psychosocial consequences of breast cancer. The breast: comprehensive management of benign and malignant diseases. 1998. 2nd ed. Philadelphia: W.B. Saunders Company;p. 1539–1552.
20. Williams TR, O'Sullivan M, Snodgrass SE, Love N. Psychosocial issues in breast cancer. Helping patients get the support they need. Postgrad Med. 1995; 98:97–99. PMID: 7567726.
21. Mor V, Allen SM, Siegel K, Houts P. Determinants of need and unmet need among cancer patients residing at home. Health Serv Res. 1992; 27:337–360. PMID: 1500290.
22. Ganz PA, Lee JJ, Sim MS, Polinsky ML, Schag CA. Exploring the influence of multiple variables on the relationship of age to quality of life in women with breast cancer. J Clin Epidemiol. 1992; 45:473–485. PMID: 1588353.

23. Mor V, Masterson-Allen S, Houts P, Siegel K. The changing needs of patients with cancer at home. A longitudinal view. Cancer. 1992; 69:829–838. PMID: 1730132.

24. Ganz PA, Schag CC, Heinrich RL. The psychosocial impact of cancer on the elderly: a comparison with younger patients. J Am Geriatr Soc. 1985; 33:429–435. PMID: 3998352.

25. Roberts CS, Rossetti K, Cone D, Cavanagh D. Psychosocial impact of gynecologic cancer: a descriptive study. J Psychosoc Oncol. 1992; 10:99–109.
26. Vinokur AD, Threatt BA, Vinokur-Kaplan D, Satariano WA. The process of recovery from breast cancer for younger and older patients: changes during the first year. Cancer. 1990; 65:1242–1254. PMID: 2302673.

27. Moos R, Tsu V. Moos R, editor. The crisis of the physical illness: An overview. Coping with physical illness. 1997. New York: Plenum Medical;p. 3–21.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download