Abstract
Clinical results of minimally invasive mitral valve surgery were retrospectively reviewed, and two different surgical approaches were compared in this study. Between 1997 and 2004, a total of 86 patients with mitral valve disease underwent minimally invasive surgery at theYonsei University Cardiovascular Center. Age of patients averaged 41.6 ± 14.0 years and 69 patients were female. Surgical approach included lowsternal incisions with mini-sternotomy, and right parasternal or thoracotomy approach. Either direct aortic or femoral arterial and bicaval cannulations were used in all patients. Patients were divided into two groups according to the method of surgical approach (parasternal (P) vs low-sternal (L)), and the results were compared. Postoperative NYHA functional class improved to 1.1 ± 0.4 in all patients (no significant statistical difference between two groups). Mean wound length (P: 9.21 ± 1.10 vs L: 11.24 ± 0.82 cm, p<0.05), and mechanical ventilation time (P: 10.42 ± 4.36 vs L: 12.90 ± 5.00 min, p=0.04) was significantly shorter in parasternal group, and mean operation time(P:294.74 ± 59.41 vs. L:259.31 ± 54.36 min, p=0.03) was significantly shorter in low-sternal group. Mean cardiopulmonary bypass time, and aortic cross clamp time was also shorter in low-sternal group without statistical difference. There were 2 minor wound complications in all patients (p=NS), and no hospital death. Comparing the two different surgical approach of minimally invasive mitral valve surgery, parasternal approach is thought to be more beneficial in reducing postoperative scar, and intubation time.
Median sternotomy has been a standard method of approach for open heart surgeries for many decades since it provides a definitive view of the surgical field.1 However, as the patients' social life improves, and as the competitions among medical institutions become intensive, lesser postoperative pain, shorter hospital stay, and better cosmetic results are being considered, and many minimally invasive surgical methods are being developed to satisfy the patients' variable demands.2-4 The less invasive surgical procedures have been growing in popularity in the past decade, and incisions have become increasingly smaller as endoscopic techniques have been developed.
The purpose of this study is to report our overall experience with minimally invasive mitral valve surgery using parasternal or lower-sternotomy approach, and compare the results of the two methods.
Between March 1997 and March 2004, 86 patients underwent minimally invasive mitral valve repair or replacement in Cardiovascular center, Yonsei University College of Medicine. Mean (± SD) age was 41.6 (± 14.0) years (range, 17 to 70) and 69 patients were female (80%) (Table 1). Preoperative clinical diagnosis included 48 isolated mitral regurgitations, 26 isolated mitral stenoses, 5 mitral and tricuspid regurgitations, 4 mitral stenoses with tricuspid regurgitations, 2 mitral regurgitations with stenoses, and 1 mitral and aortic regurgitation (Table 2). Patients with previous open-heart surgery, pectus excavatum, and significant comorbid medical conditions were excluded from this approach. Preoperative concomitant medical conditions and the operations performed are expressed in table 3, and table 4. Among 9 patients who had received percutaneous mitral valvuloplasty, two patients had emergency valve replacement due to acute development of severe mitral insufficiency as a complication of the procedure.
The mean preoperative New York Heart Association (NYHA) functional class and mean left ventricular ejection fraction (%) were 2.8 ± 0.5 (range, 2 to 4), and 64.5 ± 8.5 (range, 37 to 84), respectively (Table 1). The follow up duration was estimated based on the date of the patients' last outpatient visit.
To compare the results of the two different methods, patients were divided into two groups. 22 patients were included in parasternal group, and 64 patients were included in low-sternal group.
The three different surgical approaches were performed during this study period. A right paramedian incision was performed in 17 patients, and right thoracotomy incision was performed in 5 patients. For these approaches, patients were positioned in semi-left lateral decubitus position with double-lumen endotracheal ventilation techniques. A right paramedian or anterolateral submammary minithoracotomy incision of approximately 8-12 cm was made, and the lung was retracted infero-laterally to expose the heart. Either the femoral or direct ascending aortic arterial cannulations were performed, and the pericardium was opened anterior to the phrenic nerve and retracted with retention sutures. Mitral valve operations were performed through vertical left atrial incision under cardiopulmonary bypass. When femoral arterial cannulation was used, another small incision was made in right or left groin.
Lower-sternal incision with J- or I- shaped ministernotomy was performed in 64 patients. Lower partial sternotomy was performed through a small 8 to 13 cm incision overlying distal aspect of the sternum. The sternotomy was extended from the sternoxiphoid junction upwards to the second intercostal space, and for J-sternotomy, it was extended further to the right intercostal space. Care was taken not to injure the right internal mammary artery. In most of the patients arterial cannulations were able to be placed into the ascending aorta. Femoral arterial cannulations were performed only in patients do not provide adequate exposure of ascending aorta. For all patients, venous cannulation was inserted through superior, and inferior vena cava.
For all patients, myocardial protection was performed via ascending aorta using antegrade method of cardioplegic delivery, and at the end of cardiopulmonary bypass, intra-cardiac air was actively removed with the aid of air-vent cannula placed in ascending aorta, and intraoperative transesophageal echocardiogram (TEE). Intraoperative TEE was performed in all patients to evaluate valvular function, myocardial performance, and to monitor the status of intracardiac deairing.
No patient was converted to the median sternotomy incision during the procedure.
All data were retrospectively collected, and statistical data were expressed as percent or mean ± standard deviation. Continuous data were analyzed using the Student's t test. A p value < 0.05 was considered to be statistically significant. The statistical package used was SPSS version 10 (version 10; SPSS Inc, Chicago, IL, USA).
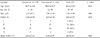
The summary of operative techniques, and patients' intraoperative data are shown in Table 5 and 6. For all patients, the mean length (cm) of skin incision was 10.3 ± 1.3 (range, 8 to 13). Mean operation time, cardiopulmonary bypass time, and aortic cross clamp time were 267.9 ± 57.3 (range, 107 to 425) minutes, 107.6 ± 26.1 (range, 60 to 212) minutes, and 73.1 ± 28.7 (range, 40 to 260) minutes, respectively. A mean amount of postoperative mediastinal bleeding on the first postoperative day was 438.6 ± 371.9 (range, 80 to 2080) mL. Mean duration of mechanical ventilator care, ICU stay, and hospital stay were 12.3 ± 4.9 (range, 4 to 28) hours, 35.3 ± 17.4 (range 17 to 96) hours, and 10.1 ± 6.6 (range 5 to 60 ) days. Postoperative NYHA functional class improved to 1.1 ± 0.4 (range 1 to 3). For those patients who had mitral valve repair, the grade of mitral regurgitation significantly decreased from 3.7 ± 0.46, preoperatively, to 0.6 ± 1.22, postoperatively. Eight patients (9%) required homologous blood transfusion, and mean amount of blood transfused were 2.5 ± 1.07 (range, 2 to 5) units. There was no hospital death, and early complications (5.8%) included superficial wound infection (2), re-exploration for bleeding (2), and prolonged ventilation due to pneumonia (1). There were no peripheral vascular complications related to femoral arterial cannulation. Mean follow up duration was 55.0 ± 25.7 (range 5 to 87) months, and follow up rate was 92%. Late complications occurred in 3 patients (3.5%). One patient had cerebral infarction that later died of infarct-related cerebral hemorrhage, and 2 patients who have had mitral valve repair had reoperations 51, and 63 months later because of significant residual mitral regurgitations. Two patients (2.3%) died of cerebral infarction, and multiple myeloma, respectively during follow up period.
The comparative results of the two different surgical approaches are shown in Table 6. Preoperative patients' profiles were not significantly different between two groups (Table 1). Mean wound length (9.21 ± 1.10 cm vs. 11.24 ± 0.82 cm, p < 0.05) was significantly shorter and mean operation time (294.74 ± 59.41 min vs 259.36 ±54.36 min, p = 0.03) was significantly longer in parasternal group. Mean cardiopulmonary bypass time (113.38 ± 30.39 min vs 105.78 ± 24.6 min, p = 0.31), and mean aortic cross clamp time (81.33 ± 28.69 min vs 70.42 ± 28.48, p = 0.14) were also longer in parasternal group, but not statistically different between two groups. Mean mechanical ventilation time (10.42 ± 4.36 hours. vs 12.9 ± 5.0 hours, p = 0.04) was significantly shorter, and mean amount of chest tube drainage was less in parasternal group with no significant difference. Mean follow duration was significantly longer in parasternal group, since we performed parasternal approach in the earlier period of this study.
Although cardiac surgery has been performed through a median sternotomy, traditionally, the left-sided approach had existed for cardiac procedures since 1910, when Alexis Carrel5 proposed it for a coronary artery bypass from the thoracic aorta, and in the 1960s, mitral valvuloplasties were commonly approached from the left side.6,7 In 1990s, the minimally invasive coronary bypass surgery began, stimulated by the increasing use of minimally invasive surgical techniques for all branches of surgery, the last being cardiac surgery.8 And in 1995, several groups began to explore the use of parasternal and ministernotomy incisions for aortic and mitral valve replacement and repair.2,4,9 To date, surgeons at the Cleveland Clinic have performed more than 2500 minimally invasive valve operations by combining direct vision with an upper hemisternotomy and modified perfusion techniques with less than a 1.0% mortality, reduced transfusions (< 10%), and earlier hospital discharge.1
The advantages of minimally invasive surgery are reducing surgical trauma, increasing patient's cosmetic satisfaction, less homologous blood transfusion, shorter hospital stay and cost, and faster recovery and returned to work.2-4,8,10,11 With these potential advantages, we started minimally invasive mitral valve operations in 1996, starting with right paramedian, or mini-thoracotomy incisions, and since 2000, we used lower sternotomy incisions, more often.
In our experience, right paramedian or thoracotomy incision brought about some difficulties in exposing the structures around the aorta, placing an arterial cannula directly into the ascending aorta, and cross-clamping the aorta. Thus most of the cases, another small incision on right or left inguinal area were necessary, and more patients complained of postoperative wound pain than the patients with lower sternotomy. Besides, this approach has more demerits including the difficulties to convert to midsternotomy, the possibility to injure the right internal mammary artery, and the possible development of asymmetric breasts.12 However, for female patients, the satisfaction for cosmetic result was superior, and most of the wound pains were well controlled with oral analgesics. Furthermore, the results of this study revealed that this patient group had more advantages including shorter wound length, and mechanical ventilator support required. On the other hands, lower ministernotomy provided a better view especially around the aorta, and in most of the cases, direct ascending aortic cannulations were feasible, and shorter operation time required. Since the two different methods of approaches have merits and demerits, now we provide the selected patients the informations about both methods, and decide which approach to perform, according to the patients' preference.
The overall results of this study showed low perioperative morbidity and mortality, and the late results also showed very low mortality, and reoperation rate. However, the mean hospital stay was slightly longer than that of other institutions, because of 3 patients operated for infective endocarditis. These patients had to stay longer for prolonged use of intravenous antibiotics, postoperatively (4 to 6 weeks).
Although minimally invasive techniques have been rapidly evolved, there are some elements limiting the extensive use of these techniques; 1) difficulties of recognizing the structures owing to the limited surgical view. 2) in patients with peripheral atherosclerotic disease with no access for femoral arterial or venous cannulations, 3) difficulties to decompress the heart during cardiopulmonary bypass, 4) difficulties to apply defibrillators, 5) difficulties for deairing, 6) limitation of surgical field for multiple valve operations, and 7) in patients with previous open heart surgery.13 Thus careful patients selection may be mandatory.
The major limitation of this study is that it is a retrospective study, although to prove the usefulness of a surgical procedure, the study should be prospective, randomized study. The second limitation is that there are no objective data to compare the patients' cosmetic satisfaction and the degree of postoperative wound pain.
In conclusion, the minimally invasive approach for isolated primary mitral valve operations with either parasternal or low-sternal approach provide the optimal surgical results and the high degree of patient's satisfaction which justify the application of the minimally invasive approach in a selected group of young and active patients.
Figures and Tables
Table 6
Comparison of Perioperative Results between Two Groups

*p<0.05, †p<0.01.
Pre-NYHA Fc, preoperative New York Heart Association functional class; CPB, cardiopulmonary bypass; ACC, aortic cross clamp; ICU, intensive care unit; Mech. Vent., mechanical ventilation; Post-EF, postoperative ejection fraction; F/u, follow up; Post-NYHA Fc, postoperative New York Heart Association functional class.
References
1. Nifong LW, Chitwood WR, Pappas PS, Smith CR, Argenziano M, Starnes VA, et al. Robotic mitral valve surgery: A United States multicenter trial. J Thorac Cardiovasc Surg. 2005. 129:1395–1404.
2. Cohn LH, Adams DH, Couper GS, Bichell DP, Rosborough DM, Sears SP, et al. Minimally invasive cardiac valve surgery improves patient satisfaction while reducing costs of valve replacement and repair. Ann Surg. 1997. 226:421–426.
3. Cosgrove DM, Sabik JF, Navia JL. Minimally invasive valve operations. Ann Thorac Surg. 1998. 65:1535–1539.
4. Navia JL, Cosgrove DM. Minimally invasive mitral valve operations. Ann Thorac Surg. 1996. 62:1542–1544.
5. Carrel A. On the experimental surgery of the thoracic aorta and the heart. Ann Surg. 1910. 52:83–95.
6. Clowes GHA, Neville WE, Sancetta SM. Results of open surgical correction of mitral valvular insufficiency and description of technique for approach from left side. Surgery. 1962. 51:138–154.
7. Austen WG, Wooler GH. Surgical treatment of mitral stenosis by the transventricular approach with a mechanical dilator. N Engl J Med. 1960. 263:661–665.
8. Greelish JP, Cohn LH, Leacche M, Mitchell M, Karavas A, Fox J, et al. Minimally invasive mitral valve repair suggests earlier operations for mitral valve disease. J Thorac Cardiovasc Surg. 2003. 126:365–373.
9. Gundry SR, Shattuck OH, Razzouk AJ, Rio MJ, Sardari FF, Bailey LL. Facile minimally invasive cardiac surgery via ministernotomy. Ann Thorac Surg. 1998. 65:1100–1104.
10. Saunders PC, Grossi EA, Sharony R, Schwartz CF, Ribakove GH, Culliford AT, et al. Minimally invasive technology for mitral valve surgery via left thoracotomy: experience with forty cases. J Thorac Cardiovasc Surg. 2004. 127:1026–1031.
11. Mihaljevic T, Cohn LH, Unic D, Aranki SF, Couper GS, Byrne JG. One thousand minimally invasive valve operations: early and late results. Ann Surg. 2004. 240:529–534.
12. Cooley DA. Minimally invasive valve surgery versus the conventional approach. Ann Thorac Surg. 1998. 66:1101–1105.
13. Chung SH, Yang JH, Nam HW, Kim KB, Ahn H. Minimally invasive cardiac surgery -three different approaches. Korean J Thorac Cardiovasc Surg. 1999. 32:438–441.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download