Abstract
Primary gastrointestinal lymphoma is a common presentation of non-Hodgkin's lymphoma. The main controversy arises when many aspects of its classification and management are under discussion, particularly regarding roles for surgical resection. The aim of this study was to evaluate clinicopathologic characteristics and the therapeutic outcome of primary gastrointestinal non-Hodgkin's lymphoma. We carried out a retrospective analysis of 74 patients who were presented to our center with histopathological diagnosis of primary gastro-intestinal non-Hodgkin's lymphoma between 1990 and 2001. All patients have been staged according to Lugano Staging System. For histopathological classification, International Working Formulation was applied. The treatment choice concerning the surgical or non-surgical management was decided by the initially acting physician. Treatment modalities were compared using the parameters of age, sex, histopathological results, stage, and the site of disease. Of the 74 patients, 31 were female and 43 were male, with a median age of 49 years (range 15-80). The stomach was the most common primary site and was seen in 51 of 74 patients (68.9%). The intermediate and high grade lymphomas constituted 91.9% of the all cases. In a median follow-up of 29 months (range 2-128), 20 out of 74 patients died. There was a three year overall survival rate in 65.4% of all patients. The three year overall survival rate was better in stage I and II1 patients who were treated with surgery plus chemotherapy (+/-RT) than those treated with chemotherapy alone (93.7% vs. 55.6%, p < 0.05). The stage and presence of B symptoms affected the disease free survival and overall survival significantly, but the histopathologic grade only affected the overall survival. On the basis of these results, we suggest that surgical resection is necessary before chemotherapy in early stage (stage I and II1) patients with gastrointestinal non-Hodgkin's lymphomas because of the significant survival advantage it would bring to the patient.
The gastrointestinal (GI) tract is the predominant site for extranodal non-Hodgkin's lymphoma (NHL). Some reports have proposed that 2% to 9% of all gastric malignancies are primary malignant lymphomas (MLs),1,2 while in the small bowel they constitute approximately 20% and in the large bowel, 0.5% of all malignancies of the remaining site.3 Primary extranodal lymphoma constitutes 25% of the NHL cases in North America and up to 50% in parts of Europe, Turkey, and Middle Eastern countries.3-5 The incidence of GI lymphoma is higher in Eastern Countries than Western Countries.4-6 High grade histopathologic types of gastric lymphomas are higher in Turkey and Middle East Countries than Western Countries.3-6
Treatment strategies for extranodal NHL are well established, but there still remains much debate and controversy regarding the optimal approach for GI-NHL, particularly for gastric lymphoma.7-12 Surgery, radiotherapy (RT), and chemotherapy (CT) have been used alone or in various combinations.13,14 Many studies have demonstrated sufficient tumor control with surgery alone especially for gastric lymphomas due to an apparent tendency of these lymphomas staying in a local stage for a prolonged time.15-20 Surgery had also been the only method for a long period in medical history where the histological diagnosis of GI-lymphoma can be established and an accurate staging of these lymphomas can be provided.21,22 This approach has generally been changed by the introduction of modern imaging techniques such as computed tomography, ultrasound, endoscopy, and endoscopic ultrasound including the technique of multiple biopsies from GI-organs for the last 25 years.
Some attempts have been made for the last 15 years to increase the survival results of surgery alone or by combining surgery and chemotherapy and/or radiation therapy23-25 as well as to preserve the stomach by a conservative treatment approach using RT and/or chemotherapy as the first treatment modality without operation.26,27 In a number of studies, some chemotherapy regimens have also been introduced for a curative intent, particularly for high grade lymphoma, and modern techniques of radiation therapy have been proven effective in lymphomas.28,29 Despite these studies, there is a debate on the necessity of any operation altogether, the requirement of completeness of operation6 and other prognostic factors, such as histological grading, thickness of tumor, intensity of chemotherapy, and radiation dose.23,30-35 To date, although several reports regarding treatment strategies of GI lymphomas have been published, only a few of them are randomized and prospective studies, and the sample sizes of these reports are not sufficiently big.13,36,38
The aim of this study is to evaluate clinicopathologic characteristics and therapeutic outcomes of primary GI-NHLs.
A retrospective study was carried out of patients who were presented to our center with a histopathological diagnosis of primary GI-NHL between 1990 and 2001. The medical charts of 92 patients were reviewed, and 74 of them were available for the analysis of clinical data (characteristics of all patients has been shown on Table 1). Treatment modalities have been compared with age, sex, histopathological grade, B and T cell histopathology, stage, and the site of disease. All patients were staged according to Lugano Staging System. For histopathological classification, International Working Formulation was applied.
An initial surgical treatment decision was made according to the surgeon's preference. In this decision, the hematologist and/or the radiation oncologist was not involved. Surgery (in which, out of 24 patients total or subtotal gastrectomy, 9 patients had Roux-en-Y resection [This is a choledocojejunostomy operation that performed for biliary by-pass], 14 patients had tumor resection, 8 patients had debulking surgery) was performed in 55 patients. Out of 55 patients, four underwent radical surgery alone. After an initial surgical resection, only chemotherapy (CT) was performed in 44 patients, chemotherapy + radiotherapy (RT) (3600 cGy total abdominal +/- 600 cGy boost RT to tumor bed) in two patients. CT + palliative surgery was performed in 5 patients. Sixteen patients received CT alone, one patient received CT + RT, and two patients got only supportive care due to their poor performance status.
(Ed: highlight - Fragment. Make this into a subtitle or into a sentence or erase altogether.)
If there was any residual disease and/or close-positive surgical margin after surgery or if lymph nodes that were ≥ 1 cm were detected by ultrasound, chemotherapy was administered additionally. If this regimen was not wholly successful, then radiation treatment was administered. Following this treatment, if there was no response with adjuvant treatment after surgery, a second line of chemotherapy was administered.
Cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) and other antracycline containing regimens are the most commonly used regimens in 65 patients (treatment modalities for all patients has been shown on Table 2). In general, we administered 6-8 cycles of the classical lymphoma regimen (CHOP-like regimens). In early stage patients, if the involved field radiation treatment was deemed necessary as a part of pretreatment in advance, chemotherapy was planned in 4 cycles.
Overall survival was computed by the life table method starting from diagnosis to the date of death or last follow-up alive. The statistical significance of observed differences was assessed by the Log-rank test. The prognostic value of different variables for the outcome was assessed by a univariate analysis and a multivariate analysis using the Cox regression model. A p value of < 0.05 was considered significant.
A total of 74 patients were evaluated, retrospectively. Of the 74 patients, 43 were male and 31 were female with a median age of 49 years (range 15-80). The median age of the patients having intestinal involvement was younger than those with gastric involvement (median 43 vs. 52 years). Stomach, small intestine, large intestine, and synchronize multiple gastrointestinal site involvement (ileocecal region was considered as small intestinal involvement) have occurred in 51 (68.9 %), 17 (23%), 2 (2.7%), and 4 (5.4%) patients respectively. According to the Lugano Staging System, 4 (5.4%) patients were in stage I, 19 (25.7%) in stage II1, 15 (20.3%) in stage II2, 16 (21.6%) in stage IIE, and 20 (27%) in stage IV (Table 1).
When our patients' initial symptoms were evaluated, we observed that most patients had gastrointestinal symptoms as seen in other series.1,5,11,13 Initial signs and symptoms were as follows: 64 patients had upper GI symptoms (nausea, vomiting and/or abdominal pain), one had jaundice, and another had diarrhea. Only eight patients were admitted in emergency circumstances (three patients with perforation, four with GI bleeding, and one with ileus). In most patients who were diagnosed endoscopically or surgically, a tumoral mass was detected, but solely gastric ulceration was detected in 14 patients. This finding shows that biopsy is critical in gastric ulcerations in terms of lymphoma diagnosis. At the time of diagnosis, 45.9% of the patients had B symptoms.
In 50 patients, endoscopic and surgical registries have been obtained. According to these registries, gastric ulceration was seen in 14 patients, vegetating masses in 12, ulcero-vegetating masses in 21, and multiple poliposis in three. Thirteen patients illustrated a bulky (> 10 cm) disease.
In the patient population, high grade and advanced stage disease were highly frequent. According to Working Formulation, six patients had low grade (8.1%), 54 had intermediate grade (73%), and 14 had high grade (18.9%). Diffuse large cell was the most frequent histopathological type (67.5%). B and T cell immunohistochemical staining had been performed in 66 patients and the T cell markers were positive in eight patients (Table 1).
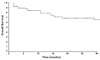
In a median follow-up of 29 months (range 2 - 128), 20 out of 74 patients died. The causes of mortality were perforation in four, ileus in four, hemorrhage in one, abdominal infection in one, acute myocardial infarction in one, and progressive disease in nine patients. A three-year overall survival rate (OS) was 65.4% in all patients (Fig. 1). A three-year OS was 83% in patients with low grade histopathology, 68% in intermediate grade patients, and 44% in high grade lymphoma patients (Fig. 2). While the three-year OS probability was 85.7% in stage I and II1 patients, this probability was only 25.5% in stage IV (Fig. 3).
We evaluated the effect of age, sex, stage, presence of B symptoms, histopathologic grade, and T cell markers positivity on survival. According to the univariate analysis, advanced stage, high grade histopathology, and the presence of B symptoms negatively affected the overall survival (OS) rate (p < 0.05) (Fig. 2 - 4). According to the Cox regression multivariate analysis, only the advanced stage was implicated in the overall survival rate (p = 0.01) (Table 3). According to the univariate analysis, the presence of B symptoms and the condition of being in the advanced stage have negatively affected the disease free survival (DFS) (p < 0.05). According to the Cox regression multivariate analysis, the advanced stage has significantly and negatively affected the DFS (p = 0.02), and the presence of B symptoms affected DFS almost to a significant extent (p = 0.04) (Table 4).
We searched the effect of surgery in patients with completely resectable early stage (stage I and II1) and unresectable-advanced stage (stage II2, IIE, IV) on overall survival and progression free survival. When observing the features of the two groups, there was no difference between the two groups in terms of histopathological and clinical variables (grade, age, and B symptoms).
Treatment related death was observed in four patients. Perforation was the cause of death in one (which was chemotherapy related in an early stage patient), and the remaining three died due to intestinal obstruction (one of them was a chemotherapy related complication in an early stage patient, one patient died from surgical complication, and the last one died from a chemotherapy complication which was in an advanced stage patient).
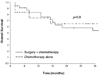
The three-year OS rate was better in stage I and II1 patients who were treated with surgery plus chemotherapy (+/-RT) than those treated with chemotherapy alone (93.7% vs. 55.6%, p = 0.027) (Fig. 5). In advanced stage diseases, performing surgery seemed to be a disadvantage, but there was no statistically significant difference (53.5% vs 64.8%, p = 0.9)(Fig. 6).
In the early stage, for those patients who underwent surgery in addition to chemotherapy, the overall response rate (complete response + partial response), 3-year DFS rate, and 3-year OS rate are statistically higher than those who received chemotherapy alone (Table 5). In the advanced stage, there were no differences in terms of 3-year DFS and OS between the two groups (Table 6).
Gastrointestinal lymphomas are the most common type of primary extranodal lymphomas.1,2,13,30,39 The stomach is the main affected site with a frequency ranging from 37.8% to 86% (mean, 59.8%).13,30,32,39 In our series of 74 patients who were reviewed retrospectively, the stomach is the main site in approximately 69% of the cases (Table 1), which is clearly higher than in other publications. But compared to the literature, the median age of the patients in our series with primary intestinal NHL is younger than that of gastric lymphoma (43 vs 52 years).5,38,40-42 Also, there is a higher male predominance in our series (male-to-female ratio: 1.3/1).
To describe the extent of the disease, most authors applied the Ann Arbor classification or its modification by Musshoff or Rohatiner.9,43 Localized stages (IE, IIE) are predominant in gastric lymphoma. Two authors report 84% and 87%,13,30 which is comparable to our data (73%), whereas published registry data are lower (68%).40 The rate for localized intestinal lymphoma is slightly lower with a range of 52% to 80% (in our series, this was 53%). Only one study states the distribution of stages in different sites of intestinal lymphoma 30 and reports a percentage in the localized disease (stages IE and IIE) of 78% for the small bowel and 80% for the ileocecal region.
The majority of GI lymphoma is of high grading in all series, but the usage of different histologic classifications makes the comparison difficult, especially in intestinal lymphomas. So far, the classification by Isaacson et al.44 has been used in only two publications,45,46 but both reports are restricted to localized gastric lymphoma. In only one published major prospective study, the Working Formulation had been primarily applied.13 In the retrospective analysis of the British National Lymphoma Investigation, the Working Formulation was used in most cases.14
Appropriate management of primary GI lymphoma is still controversial. The most controversial issue on the treatment of GI lymphomas is whether or not the surgical treatment approach is necessary. Although there are a lot of studies on the advantage of surgical treatment in stage I-II1 disease, most of these are non- randomized and have conflicting results.3,14,17-19,36 Another issue is to what extent surgery is necessary.47 On the other hand, surgery may delay the use of chemotherapy, causes some morbidity, and also has a mortality rate of up to 10%. Currently, several series have reported patients who have been treated with surgery and chemotherapy; with biopsy, chemotherapy, and irradiation; or with biopsy and irradiation.27,48,49 In an analysis by the Danish Lymphoma Study Group of 175 gastric lymphomas, 105 were localized.32 Sixty-seven of 105 patients had surgery. The authors found no role for surgery in altering the overall or relapse-free survival rates. In completely resectable early stage patients, surgery had more of an advantage. On the contrary, surgery had no survival advantage in advanced stage patients, and might even have some disadvantage. In our series, eight patients out of 20, died in the first four months of treatment. Four of them died due to surgical complications (one intraabdominal infection, two perforation, and one ileus), and the remaining four died because of chemotherapeutic complications (two perforation, two ileus). Although it was stated that surgery has the advantage of total tumor removal and limits the risk of hemorrhage and perforation,17-19 this was not supported by the analysis of our patients. If primary intestinal lymphoma is diagnosed at laparotomy, surgical resection can be preferred. In the advanced disease, where resection is not technically feasible, treatment consists of anthracycline-based chemotherapy followed, in some cases, by radiation therapy. However, due to the absence of randomized trials, the optimal treatment strategy is not known.47 In our series, 17 patients were diagnosed at laparotomy, and the tumors were resected in 14 of them.
Current clinical trials are being proposed in order to treat patients with clearly resectable disease with surgery plus chemotherapy versus chemotherapy plus radiation therapy. Patients with unresectable disease were randomly assigned to receive chemotherapy alone versus chemotherapy plus irradiation, and chemotherapy was more intense in these patients.50
The outcomes reported in the literature vary depending on the extent and histology of the disease. Most publications have stated a survival rate (SR) for all intestinal lymphomas together with a range of 24% to 67%, and the estimated 5-year SR was 67.1% in our series and 67% in another prospective study.13 In a large series of intestinal lymphomas, Domizio and co-workers 38 documented a 5-year SR of 75% for patients with low-grade B-cell lymphomas and only 25% for those with T-cell tumors; the poor outcome for intestinal T-cell lymphoma was also documented in the British and Danish experience.14,32 In all reports, the number of intestinal lymphomas is small. To allow for a better comparison, different parts of the intestine should be clearly defined which from our point of view is of importance especially for lymphomas of the ileocecal region that seems to have a prognosis comparable to that of gastric lymphoma. Ileocecal NHL can be diagnosed by endoscopy, and a fact raises the question of whether surgery is really necessary for a treatment. In conclusion, it seems that intestinal lymphomas has raised less interest in the past but should become the aim of prospective studies.36
In general, there is a demand for a standardized staging system. Therefore, we proposed to use the basic framework of the Ann Arbor classification 51, incorporating Rohatiner's subdivision of stage II (Lugano Staging System).11 Stage I included patients with lymphoma confined to the gastrointestinal tract as the single primary site or multiple, non-contiguous lesions. Stage II lymphoma was extended into the abdomen from the primary site involving local (perigastric/mesenteric) (stage II1) or distant (celiac, para-aortic, paracaval or retroperitoneal) (stage II2) lymp nodes or penetrated into serosa involving adjacent organs or tissues (stage IIE). Finally, stage IV patients had a disseminated extranodal involvement of lymphoma or a gastrointestinal lesion with supradiaphragmatic nodal involvement. Although the Revised European-American Lymphoma (REAL) classification and the World Health Organization (WHO) classification included extranodal lymphomas for the first time, the detailed subclassification of high-grade lymphoma of MALT type as published by Isaacson et al.8 has not been taken into account because of its clinical implications.52 However, even in WHO and REAL classifications, extranodal lymphomas are included, and there are no standard classifications for the high grade GI lymphomas.
In summary, GI-NHL is a heterogeneous disease depending on the site of origin within the GI tract. Primary gastric lymphoma is by far the largest group, which has its own distinct histopathologic and clinical features. Stage is the most important prognostic factor, with a significantly better survival for the localized disease. The frequency of gastric lymphoma in stages IE and IIE allows for an analysis of the treatment strategy that concerns the combined surgical and conservative treatment versus conservative treatment alone. As for the analysis of the advanced disease in lymphoma of the stomach, as well as in intestinal NHL, a larger number of patients is required.
In conclusion, this study shows that gastrointestinal complications are the most important cause of mortality in patients with GI lymphomas. Poor prognostic factors were more frequent in our patients than that of Western Countries. Surgical resection may be considered before chemotherapy in patients with early stage (stage I and II1) GI lymphomas because this leads to a good survival probability. On the other hand, it seems that surgery has no advantage in the advanced disease, and by contrast, due to the adverse effect of surgery in these patients, debulking surgery is also not suggested.
Figures and Tables
Fig. 2
The effect of histopathological grades on overall survival in low, intermediate and high grade gastrointestinal non-Hodgkin's lymphoma.

Fig. 5
The effect of surgery on the overall survival in stage I-II1 gastrointestinal non-Hodgkin's lymphoma.

Fig. 6
The effect of surgery on the overall survival in advanced stages of gastrointestinal non-Hodgkin's lymphoma.
References
1. Freeman C, Berg JW, Cutler SJ. Occurence and prognosis of extranodal lymphomas. Cancer. 1972. 29:252–260.
2. Lee Y-TN, Spratt JS. Malignant Lymphoma, Nodal and Extranodal Diseases (Modern Surgical Monograph). Gastrointestinal malignant lymphomas. 1974. New York: Grune and Stratton;229–260.
3. Dincol D, Icli F, Erekul S, Gunel N, Karaoguz H, Demirkazik A. Primary gastrointestinal lymphomas in Turkey: a retrospective analysis of clinical features and results of treatment. J Surg Oncol. 1992. 51:270–273.
4. Sarpel SC, Paydas S, Tuncer I, Varinli S, Koksal M, Akoglu T. Non-Hodgkin's lymphomas in Turkey. Cancer. 1988. 62:1653–1657.
5. Otter R, Bieger R, Kluin PM, Hermans J, Willemze R. Primary gastrointestinal non-Hodgkin's lymphoma in a population-based registry. Br J Cancer. 1989. 60:745–750.
6. Salem P, Anaissie E, Allam C, Geha S, Hashimi L, Ibrahim N, et al. Non-Hodgkin's lymphomas in the Middle East. A study of 417 patients with emphasis on special features. Cancer. 1986. 58:1162–1166.
7. Stansfeld AG, Diebold J, Noel H, Kapanci Y, Rilke F, Kelenyi G, et al. Updated Kiel classification for lymphomas. Lancet. 1988. 1:292–293. (letter).
8. Isaacson P, Wright DH. Extranodal malignant lymphoma arising from mucosa-associated lymphoid tissue. Cancer. 1984. 53:2515–2524.
9. Musshoff K. Klinische Stadieneinteilung der Nicht-Hodgkin-Lymphome. Strahlentherapie. 1977. 153:218–221.
10. Schmidt WP, Schmitz N, Sonnen R. Conservative management of gastric lymphoma: the treatment option of choice. Leuk Lymphoma. 2004. 45:1847–1852.
11. Rohatiner A, d'Amore F, Coiffier B, Crowther D, Gospadarowicz M, Isaacson P, et al. Report on a workshop convened to discuss the pathological and staging classifications of gastrointestinal tract lymphoma. Ann Oncol. 1994. 5:397–400.
12. Shimodaira M, Tsukamoto Y, Niwa Y, Goto H, Hase S, Hayakawa T, et al. A proposed staging system for primary gastric lymphoma. Cancer. 1994. 73:2709–2715.
13. Ruskone-Fourmestraux A, Aegerter P, Delmer A, Brousse N, Galian A, Rambaud JC, et al. Primary digestive tract lymphoma: A prospective multicentric study of 91 patients-Groupe d'Etude des Lymphomes Digestifs. Gastroenterology. 1993. 105:1662–1671.
14. Morton JE, Leyland MJ, Vaughan Hudson G, Vaughan HB, Anderson L, Bennett MH, et al. Primary gastrointestinal non-Hodgkin's lymphoma: A review of 175 British National Lymphoma Investigation cases. Br J Cancer. 1993. 67:776–782.
15. Dawson IMP, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Br J Surg. 1961. 49:80–89.
16. Lim FE, Hartmann AS, Tan EGC, Cady B, Meissner WA. Factors in the prognosis of gastric lymphoma. Cancer. 1977. 39:171–172.
17. Baildam AD, Williams GT, Schofield PF. Abdominal lymphoma-the place for surgery. J R Soc Med. 1986. 82:657–660.
18. Feil W, Wenzl E, Radaskiewicz T, Schiessel R. Non Hodgkin lymphoma of the stomach: Surgical therapy and prognosis. Klin Wschr. 1987. 99:426–430.
19. Verreet PR, Borchard F, Stöltzing H, Thon K, Röher HD. Status of gastrectomy in the multi-modality therapy concept of primary non-Hodgkin's lymphoma of the stomach. Langenbecks Arch Chir. 1990. 375:151–155.
20. Brands F, Monig SP, Raab M. Treatment and prognosis of gastric lymphoma. Eur J Surg. 1997. 163:803–813.
21. Brooks JJ, Enterline HT. Primary gastric lymphomas: A clinicopathologic study of 58 cases with long-term follow-up and literature review. Cancer. 1983. 51:701–711.
22. Nakamura S, Matsumoto T, Lida M, Yao T, Tsuneyoshi M. Primary gastrointestinal lymphoma in Japan: a clinicopathologic analysis of 455 patients with special reference to its time trends. Cancer. 2003. 97:2462–2473.
23. Dragosics B, Bauer P, Radaskiewicz T. Primary gastrointestinal non-Hodgkin's lymphomas. A retrospective clinicopathologic study of 150 cases. Cancer. 1985. 55:1060–1073.
24. Gospodarowicz MK, Bush RS, Brown TC, Chua T. Curability of gastrointestinal lymphoma with combined surgery and radiation. Int J Radiat Oncol Biol Phys. 1983. 9:3–9.
25. Chung HC, Roh JK, Koh EH, Kim JH, Hahn JS, Park IS, et al. Comparison of adjuvant radiotherapy and chemoradiotherapy following surgery in stage IE and IIE primary gastrointestinal tract non-Hodgkin's lymphoma. Yonsei Med J. 1990. 31:144–155.
26. Maor MH, Maddux B, Osborne BM, Fuller LM, Sullivan JA, Nelson RS, et al. Stages IE and IIE non-Hodgkin's lymphoma of the stomach: Comparison of treatment modalities. Cancer. 1984. 54:2330–2337.
27. Maor MH, Velasquez WS, Fuller LM, Silvermintz KB. Stomach conservation in stages IE and IIE gastric non-Hodgkin's lymphoma. J Clin Oncol. 1990. 8:266–271.
28. Gobbi PG, Dionigi P, Barbieri F, Corbella F, Bertoloni D, Grignani G, et al. The role of surgery in the multimodal treatment of primary gastric non-Hodgkin's lymphomas. Cancer. 1990. 65:2528–2536.
29. Sonnen R, Calavrezos A, Grimm HA, Kuse R. Combined conservative treatment of localized stomach lymphoma. Dtsch Med Wochenschr. 1994. 119:863–868.
30. Azab MB, Henry-Amar M, Rougier P, Bognel C, Theodore C, Carde P, et al. Prognostic factors in primary gastrointestinal non-Hodgkin's Lymphoma. A multivariate analysis, report of 106 cases, and review of the literature. Cancer. 1989. 64:1208–1217.
31. Herrmann R, Panahon AM, Barcos MP, Walsh D, Stutzman L. Gastrointestinal involvement in non-Hodgkin's lymphoma. Cancer. 1980. 46:215–222.
32. Lewin KJ, Ranchod M, Dorfman RF. Lymphomas of the gastrointestinal tract: A study of 117 cases presenting with gastrointestinal disease. Cancer. 1978. 42:693–707.
33. Shiu MH, Karas M, Nisce L, Lee BJ, Filippa DA, Lieberman PH. Management of primary gastric lymphoma. Ann Surg. 1982. 195:196–202.
34. Shiu MH, Nisce LZ, Pinna A, Straus DJ, Tome M, Filippa DA, et al. Recent results of multimodal therapy of gastric lymphoma. Cancer. 1986. 58:1389–1399.
35. Steward WP, Harris M, Wagstaff J, Scarffe JH, Deakin DP, Todd DH, et al. A prospective study of the treatment of high-grade histology non-Hodgkin's lymphoma involving the gastrointestinal tract. Eur J Cancer Clin Oncol. 1985. 21:1195–1200.
36. Koch P, del Valle F, Berdel WE, Willich NA, Reers B, Hiddemann W, et al. Primary gastrointestinal non-Hodgkin's lymphoma: I. Anatomic and histologic distribution, clinical features, and survival data of 371 patients registered in the German Multicenter Study GIT NHL 01/92. J Clin Oncol. 2001. 19:3861–3873.
37. Krugmann J, Dirnhofer S, Gschwendtner A, Berresheim U, Greil R, Krugmann K, et al. Primary gastrointestinal B-cell lymphoma. A clincopathological and immunohistochemical study of 61 cases with an evaluation of prognostic parameters. Pathol Res Pract. 2001. 197:385–393.
38. Haber DA, Mayer RJ. Primary gastrointestinal lymphoma. Semin Oncol. 1988. 15:154–169.
39. Liang R, Todd D, Chan TK, Chiu E, Lie A, Kwong YL, et al. Prognostic factors for primary gastrointestinal lymphoma. Hematol Oncol. 1995. 13:153–163.
40. D'Amore F, Brincker H, Gronbaek K, Thorling K, Pedersen M, Jensen MK, et al. Non-Hodgkin's lymphoma of the gastrointestinal tract: A populationbased analysis of incidence, geographic distribution, clinicopathologic presentation features, and prognosis-Danish Lymphoma Study Group. J Clin Oncol. 1994. 12:1673–1684.
41. Hansen PB, Vogt KC, Skov RL, Pedersen-Bjergaard U, Jacobsen M, Ralfkiaer E, et al. Primary gastrointestinal non-Hodgkin's lymphoma in adults: A population-based clinical and histopathologic study. J Intern Med. 1998. 244:71–78.
42. Gurney KA, Cartwright RA, Gilman EA. Descriptive epidemiology of gastrointestinal non-Hodgkin's lymphoma in a population-based registry. Br J Cancer. 1999. 79:1929–1934.
43. Mafune KI, Tanaka Y, Suda Y, Izumo T. Outcome of patients with non-Hodgkin's lymphoma of the stomach after gastrectomy: clinicopathologic study and reclassification according to the revised European-American lymphoma classification. Gastric Cancer. 2001. 4:137–143.
44. Isaacson PG, Spencer J, Wright DH. Classifying primary gut lymphomas. Lancet. 1988. 2:1148–1149. (letter).
45. Radaszkiewicz T, Dragosics B, Bauer P. Gastrointestinal malignant lymphomas of the mucosa-associated lymphoid tissue: Factors relevant to prognosis. Gastroenterology. 1992. 102:1628–1638.
46. Cogliatti SB, Schmid U, Schumacher U, Eckert F, Hansmann ML, Hedderich J, et al. Primary B-cell gastric lymphoma: A clinicopathological study of 145 patients. Gastroenterology. 1991. 101:1159–1170.
47. Gospodarowicz MK, Wasserman TH. Perez CA, Brady LW, editors. Non-Hodgkin's Lymphoma. Principles and practice of radiation oncology. 1998. New York: Lippincott-Raven;2000–2001.
48. Valicenti RK, Wasserman TH, Monyak DJ, Kucik NA. Non-Hodgkin Lymphoma: Whole- abdomen irradiation as an adjuvant to chemotherapy. Radiology. 1994. 192:571–576.
49. Taal BG, Burgers JM, van Heerde P, Hart AA, Somers R. The clinical spectrum and treatment of primary non-Hodgkin's lymphoma of the stomach. Ann Oncol. 1993. 4:839–840.
50. Willich NA, Reinartz G, Horst EJ, Delker K, Reers B, Hiddemann W, et al. Operative and conservative management of primary gastric lymphoma: Interim results of a German multicenter study. Int J Radiat Oncol Biol Phys. 2000. 46:895–901.
51. Koch P, Hiddemann W. Mason DY, Harris NL, editors. Therapy of gastric lymphoma of MALT type, including antibiotics. Human lymphoma: Clinical implications of the REAL classification. 1999. London: United Kingdom, Springer-Verlag;201–208.




 PDF
PDF ePub
ePub Citation
Citation Print
Print










 XML Download
XML Download