Abstract
The function of inspiratory muscles is crucial for effective cough as well as expiratory muscles in patients with Duchenne muscular dystrophy (DMD). However, there is no report on the correlation between cough and inspiratory muscle strength. To investigate the relationships of voluntary cough capacity, assisted cough techniques, and inspiratory muscle strength as well as expiratory muscle strength in patients with DMD (n = 32). The vital capacity (VC), maximum insufflation capacity (MIC), maximal inspiratory pressure (MIP), and maximal expiratory pressure (MEP) were measured. Unassisted peak cough flow (UPCF) and three different techniques of assisted PCF were evaluated. The mean value of MICs (1918 ± 586 mL) was higher than that of VCs (1474 ± 632 mL) (p < 0.001). All three assisted cough methods showed significantly higher value than unassisted method (212 ± 52 L/min) (F = 66.13, p < 0.001). Combined assisted cough technique (both manual and volume assisted PCF; 286 ± 41 L/min) significantly exceeded manual assisted PCF (MPCF; 246 ± 49 L/min) and volume assisted PCF (VPCF; 252 ± 45 L/min) (F = 66.13, p < 0.001). MIP (34 ± 13 cmH2O) correlated significantly with both UPCF and all three assisted PCFs as well as MEP (27 ± 10 cmH2O) (p < 0.001). Both MEP and MIP, which are the markers of respiratory muscle weakness, should be taken into account in the study of cough effectiveness.
Duchenne muscular dystrophy (DMD) causes progressive weakness of respiratory muscles, in common with other skeletal muscles, over the course of the disease.1 Vital capacity increases concomitantly with the physical growth until the early teens, however, it begins to decrease earlier in the DMD patients than the normal persons followed by plateau.2 As growth slows and muscle weakness progresses, the vital capacity enters a descending phase and declines at an average rate of 8-8.5% per year after 10-12 years of age.3 As a result, patients develop chronic alveolar hypoventilation in advanced stage.4
The weakened respiratory muscles can neither fully expand the lungs up to the maximal capacity nor compress them to the point of the smallest residual volume, leading to reduction of chest wall compliance through shortening and stiffening of the unstretched tissue and fibrosis of dystrophic muscles.5 The compliance of the lungs are also reduced by the spreading of microatelectasis in the lungs.6 This respiratory disability diminishes the lung capacity and causes impairment of the ability to cough.7 When the force of cough is diminished, airway secretion can not be sufficiently eliminated. Impaired secretion clearance results in the development of mucus plugging, leading to such complications as atelectasis or pneumonia. In fact, about 90% of respiratory failures develop suddenly as a result of impaired clearance of the airways during intercurrent chest colds due to the ineffective cough.8 Therefore, the most important aspect of the pulmonary hygiene therapy for these patients is to improve the effectiveness of coughing.
For an effective cough, subjects initially inspire a large amount of air and apply expiratory force against a closed glottis, generating high thoraco-abdominal pressures. At this point, the glottis opens, resulting in strong expiratory flow.9,10 Based on this cough mechanism, several cough assisting methods have been proposed for patients with respiratory muscle weakness, such as respiratory muscle training,11 functional electrical stimulation of abdominal muscles,12 and manual assist coughing following a maximum insufflation.13 As known in cough mechanism and assisted coughing techniques, the expiratory muscles play the most basic and important role in producing a functional cough flow. Therefore, a great deal of interests and researches focused on correlation between expiratory muscle strength and cough. Although expiratory muscle function is a crucial part of an effective cough, the lung volume attained prior to contraction of the expiratory muscle also plays an important part during cough. The function of inspiratory muscles is essential in inspiratory phase of cough, however, there is no report on the correlation between cough and inspiratory muscle strength.
In this study, therefore, we investigated the relationships of voluntary cough capacity, assisted cough techniques, and inspiratory muscle strength as well as expiratory muscle strength.
The study subjects were the patients who underwent general examinations such as medical history, physical findings, muscle enzyme study and electrodiagnostic study, and were finally diagnosed as DMD through muscle biopsy or DNA analysis. The study included 32 patients who were selected from the patients in the grade 5 or over of the functional level classification proposed by Swinyard et al.14 The study excluded those patients who had concomitant intrinsic lung disease or indwelling tracheostomy tube, and who were unable to cooperate because of mental or physical problem. The protocol of the study was approved by the Hospital Ethical Committee.
Vital capacity (VC) and maximum insufflation capacity (MIC) of the patients were measured in a sitting position using Wright spirometer (Ferraris Development & Engineering Co Ltd, Northants, UK). For measuring MIC, the patient was told to take a deep breath and then hold it. A volume of air is then delivered via a mouth piece or oronasal interface by using a manual resuscitator bag. The patient adds this air to what was already in the lungs and holds it with the glottis closed. The process was repeated until no more air could be held, and the lungs and chest wall were fully expanded. The maximally stacked volume of air was measured by having the patient blow the entire volume through the spirometer. This process was repeated at least three times and the highest value was selected as the MIC.
The maximal respiratory pressure reflecting the strength of respiratory muscles were measured by mouth pressure meter (Spirovis, Cosmed Srl, Rome, Italy) in a sitting position. To measure a maximal expiratory pressure (MEP), the subject performed a maximal expiratory effort after a maximal inspiration. Maximal inspiratory pressure (MIP) was measured by exerting a maximal inspiratory effort after a maximal expiration. The pressures measured should be maintained for at least one second. The highest positive value for MEP and the lowest negative value for MIP in three or more attempts were chosen. The absolute value of MIP was used for analyzing the data.
The peak cough flows (PCFs) were measured using a peak flow meter (Health Scan Products Inc, Cedar Grove, NJ, USA). Unassisted peak cough flow (UPCF) was measured by having the person cough as forcefully as possible through the peak flow meter. Three different techniques of assisted PCF were evaluated. To measure volume assisted peak cough flow (VPCF) which assists inspiratory phase of cough, patients were insufflated to the MIC and then coughed as forcefully as possible. Manual assisted peak cough flow (MPCF), which assists expiratory muscle function, was measured while abdominal thrust was timed to glottic opening. Both techniques were carried out simultaneously in the combined assisted cough technique as combined peak cough flow (CPCF). It consisted of manual abdominal compression during the expulsive phase of a maximal voluntary cough after insufflating to MIC. We compared the PCFs under four different conditions. The highest value in at least three trials was used in each tests, and the correlation between the MIP, MEP and PCFs under each condition was evaluated.
A paired t test was used for the comparison between VC and MIC, and repeated measure analysis of variance was used for the comparisons between UPCF and each assisted PCF. If repeated measure analysis of variance detect significance, a post hoc comparison test was performed by least significant difference (LSD). A relationship between the maximal respiratory pressures and the PCFs was analyzed through a coefficients of correlation. All data were analyzed by using SPSS 11.0 for Windows (SPSS Inc, Chicago, IL, USA).
Thirty-two male DMD patients were involved. Mean age was 17.6 ± 5.1 years old, mean height was 153.3 ± 8.8 cm, and mean weight was 44.9 ± 13.2 kg. The average values of VCs and MICs were 1474 ± 632 mL(45.2 ± 22.5% of predicted normal value15,16) and 1918 ± 586 mL, respectively, and the mean values of MIPs and MEPs were 34 ± 13 cmH2O (41.7 ± 16.9% of predicted normal value17) and 27 ± 10 cmH2O (21.6 ± 10.8% of predicted normal value17), respectively. The mean PCFs under different conditions were: UPCF, 212 ± 52 L/min; VPCF, 252 ± 45 L/min; MPCF, 246 ± 49 L/min; CPCF, 286 ± 41 L/min.
The mean value of MICs was higher than that of VCs (p < 0.001). All of three assisted cough methods showed significantly higher value than unassisted method (F = 66.13, p < 0.001), and CPCF significantly exceeded MPCF and VPCF (F = 66.13, p < 0.001) (Table 1). MEP correlated with voluntary cough capacity (UPCF) as expected (p < 0.001) (Fig. 1). Positive correlations between MEP and three different assisted cough methods were also evident (p < 0.001) (Fig. 2, 3, 4). In the relationship between absolute value of MIP and PCFs, MIP correlated significantly with both UPCF (Fig. 1) and all of three assisted PCFs (p < 0.001) (Fig. 2, 3, 4).
The maximal respiratory pressure is a useful marker of respiratory muscle weakness. Generally, the VC in DMD patients doesn't show an apparent decrement until 10 years old, and the maximal respiratory pressure begins to decline earlier in the course of the disease.18 It suggests that maximal respiratory pressure is more sensitive for the detection of weakness of respiratory muscles than pulmonary volumes.19 The weakness of the respiratory muscles induces restrictive lung disease and causes ineffective cough. Cough is an essential process to prevent pulmonary complications, such as pneumonia and atelectasis, by removing excessive pulmonary secretions from the airways.10,20 Weakened respiratory muscles in these patients cannot effectively expel the pulmonary secretions, particularly when secretions are increased by respiratory tract infections. The consequence of impaired secretion clearance is the development of mucus plugging, leading to such acute complications as atelectasis or pneumonia due to bronchial plugging.
To be an effective cough, three actions of normal cough (inspiration, compression, and expulsion) should properly be operated.9 In the inspiration phase, normal subjects increase pre-cough tidal volumes to about 85 to 90% of their inspiratory capacity and have a total cough volume of 2.3 ± 0.5 L to obtain optimal PCFs.20 During the compression phase, expiratory force against a closed glottis results in a rapid rise in pleural and alveolar pressures.9,10 The contraction of the expiratory muscles with the glottis open strongly expel the air from the lungs in the expulsion phase.9,10 When any of these phases is in an abnormal state, coughing becomes ineffective. If the sufficient amount of air cannot be voluntarily inspired due to the weakness of the inspiratory muscles, the cough capacity is diminished despite the normal contraction of the expiratory muscles.7 A glottis plays a crucial role in the compression phase, and its function is considerably impaired in the amyotrophic lateral sclerosis because of involvement of bulbar muscle.21 However, it doesn't become an issue in DMD. The expiratory muscle plays an important role in the compression and expulsive phases, and its weakness of course reduces the effectiveness of cough.9,10 MEP typically deteriorates before MIP in patients with DMD.4 Thus, the declines in MEP correlate well with the voluntary cough capacity (UPCF), as shown in our present as well as other studies.4,10,22
Although the MIP, which reflects the strength of all inspiratory muscles, is expected to affect the inspiratory phase of cough, there is no study on the relation between cough capacity and MIP. Therefore, we examined the correlation between the MIP and the cough capacity, and found that the UPCF had significant correlations with not only MEP, but also MIP. The positive correlations between maximal respiratory pressures and three different assisted cough methods were also seen. As anticipated, the correlation between MIP/MEP and UPCF was relatively strong. However, the correlation between MIP/MEP and two assisted PCFs was lower and the correlation between MIP/MEP and CPCF was lower still, most likely because of the extrinsic factors of volume and manual assisted cough methods becoming more important in generating peak cough flow. In DMD patients accompanied with reduced pre-cough inspiration volume, an assisted coughing method to assist only the expiratory muscles may not be sufficient to induce strong cough flow. Therefore, both manual compression and mechanical insufflation should be considered to assist expectoration of secretions in patients with respiratory muscle weakness. As seen in the present study, patients can get the highest cough flow in CPCF technique. This result together with such relationship between maximal respiratory pressures and two different assisted cough methods suggest that both MEP and MIP, which are the markers of respiratory muscle weakness, should be taken into account in the study of cough effectiveness.
Deep inspiration expands the more distal airways, improve the expiratory muscle function, and increases pulmonary recoil pressure of the respiratory system.23-25 Forced expiration during cough normally starts with maximum inflation of the lungs and greater expiratory pressures, and flows can be produced at high lung volumes by optimizing the length-tension relationship of the expiratory muscles.24,25 Therefore, cough flow is reduced by the inspiratory muscle weakness as well as expiratory muscle weakness.10,25 As the strength of inspiratory muscle declines, patients lose the ability to take spontaneous periodic deep breaths, which normally stimulate surfactant production and distribution, and reopen collapsed peripheral airways.26 Without deep insufflations, these patients first develop microatelectasis, and long-term inability to take deep breaths or chronic hypoinflation results in permanent pulmonary restriction. Thus, decreased pulmonary compliance results initially from microatelectasis, and ultimately from increased stiffness of the chest wall and lung tissues themselves.27 An effective cough relies on the generation of sufficient dynamic airway compression to produce high airflow velocities. In contrast, the diminished lung compliance may limit dynamic airway compression and can be an another factor to cause weak coughing.7 Theses various kinds of factors are correlated with the MIP and can affect the cough capacity.
In conclusion, a reduced cough capacity due to respiratory muscles weakness is one of the main causes of morbidity and mortality in DMD. It is generally believed that MIP is correlated with cough capacity. In reality, the function of inspiratory muscle is often overlooked when coughing methods are used and no study has analyzed the correlation between MIP and cough flow using numerical data. We adduced evidence of relationship between MIP and cough flow to emphasize the importance of inspiratory muscle strength. The factors to affect a cough should thoroughly be analyzed to effectively assist weakened cough. As shown in the present study, not only MEP but also MIP should be considered in the research of voluntary or assisted cough capacity.
References
1. Inkley SR, Oldenburg FC, Vignos PJ Jr. Pulmonary function in Duchenne muscular dystrophy related to stage of disease. Am J Med. 1974; 56:297–306. PMID: 4813648.

2. Lynn DJ, Woda RP, Mendell JR. Respiratory dysfunction in muscular dystrophy and other myopathies. Clin Chest Med. 1994; 15:661–674. PMID: 7867281.

3. Hahn A, Bach JR, Delaubier A, Rinardel-lrani A, Guillou C, Rideau Y. Clinical implications of maximal respiratory pressure determinations for individuals with Duchenne muscular dystrophy. Arch Phys Med Rehabil. 1997; 78:1–6. PMID: 9014949.

4. Bach JR, O'brien J, Krotenberg R, Alba AS. Management of end stage respiratory failure in Duchenne muscular dystrophy. Muscle Nerve. 1987; 10:177–182. PMID: 3547120.

5. Estenne M, Heilporn A, Delhez L, Yernault JC, De Troyer A. Chest wall stiffness in patients with chronic respiratory muscle weakness. Am Rev Respir Dis. 1983; 128:1002–1007. PMID: 6228174.
6. Gibson GJ, Pride NB, Davis JN, Loh LC. Pulmonary mechanics in patients with respiratory muscle weakness. Am Rev Respir Dis. 1977; 115:389–395. PMID: 842952.
7. Smith PE, Calverley PM, Edward RH, Evans GA, Campbell EJ. Practical problems in the respiratory care of patients with muscular dystrophy. N Engl J Med. 1987; 316:1197–1205. PMID: 3553943.

8. Bach JR, Rajaraman R, Ballanger F, Tzeng AC, Ishikawa Y, Kulessa R, et al. Neuromuscular ventilatory insufficiency: the effect of home mechanical ventilator use vs. oxygen therapy on pneumonia and hospitalization rates. Am J Phys Med Rehabil. 1998; 77:8–19. PMID: 9482374.
9. Scanlan C, Myslinski MJ. Scanlan CL, Wilkins RL, Stoller JK, editors. Bronchial hygiene therapy. Egan's fundamentals of respiratory care. 1999. 3rd ed. St. Louis: Mosby;p. 792–793.
10. Schramm CM. Current concepts of respiratory complications of neuromuscular disease in children. Curr Opin Pediatr. 2000; 12:203–207. PMID: 10836153.

11. Estenne M, Knoop C, Vanvaerenbergh J, Heilporn A, De Troyer A. The effect of pectoralis muscle training in tetraplegic subjects. Am Rev Respir Dis. 1989; 139:1218–1222. PMID: 2712449.

12. Linder SH. Functional electrical stimulation to enhance cough in quadriplegia. Chest. 1993; 103:166–169. PMID: 8417872.

13. Kang SW, Bach JR. Maximum insufflation capacity: vital capacity and cough flows in neuromuscular disease. Am J Phys Med Rehabil. 2000; 79:222–227. PMID: 10821306.
14. Swinyard CA, Deaver GG, Greenspan L. Gradients of functional ability of importance in rehabilitation of patients with progressive muscular and neuromuscular diseases. Arch Phys Med Rehabil. 1957; 38:574–579. PMID: 13459572.
15. Morris JF. Spirometry in the evaluation of pulmonary function. West J Med. 1976; 125:110–118. PMID: 969495.
16. da Costa JL. Pulmonary function studies in healthy Chinese adults in Singapore. Am Rev Respir Dis. 1971; 104:128–131. PMID: 5556227.
17. Wilson SH, Cooke NT, Edwards RH, Spiro SG. Predicted normal values for maximal respiratory pressures in Caucasian adults and children. Thorax. 1984; 39:535–538. PMID: 6463933.

18. McDonald CM, Abresch RT, Carter GT, Fowler WM Jr, Johnson Er, Kilmer DD, et al. Profiles of neuromuscular diseases: Duchenne muscular dystrophy. Am J Phys Med Rehabil. 1995; 74(Suppl 5):S70–S92. PMID: 7576424.
19. Griggs RC, Donohoe KM, Utell MJ, Goldblatt D, Moxley RT 3rd. Evaluation of pulmonary function in neuromuscular disease. Arch Neurol. 1981; 38:9–12. PMID: 7458733.

20. Leith DE. Brain JD, Proctor D, Reid L, editors. Cough. Lung biology in health and disease. 1977. New York: Marcel Dekker;p. 545–592.
21. Bach JR. Amyotrophic lateral sclerosis: predictors for prolongation of life by noninvasive respiratory aids. Arch Phys Med Rehabil. 1995; 76:828–832. PMID: 7668953.

22. Szeinberg A, Tabachnik E, Rashed N, McLaughlin FJ, England S, Bryan CA, et al. Cough capacity in patients with muscular dystrophy. Chest. 1988; 94:1232–1235. PMID: 3191765.

23. McCool FD, Tzelepis GE. Inspiratory muscle training in the patient with neuromuscular disease. Phys Ther. 1995; 75:1006–1014. PMID: 7480122.

24. Hadjikoutis S, Wiles CM, Eccles R. Cough in motor neuron disease: a review of mechanisms. QJM. 1999; 92:487–494. PMID: 10627867.

26. Schmidt-Nowara WW, Altman AR. Atelectasis and neuromuscular respiratory failure. Chest. 1984; 85:792–795. PMID: 6723392.

27. Estenne M, De Troyer A. The effects of tetraplegia on chest wall statics. Am Rev Respir Dis. 1986; 134:121–124. PMID: 2942066.
Fig. 1
Relationships between maximal respiratory pressures and UPCF. Both absolute value of MIP and MEP correlated significantly with UPCF. UPCF, Unassisted peak cough flow; MIP, Maximal inspiratory pressure; MEP, Maximal expiratory pressure.
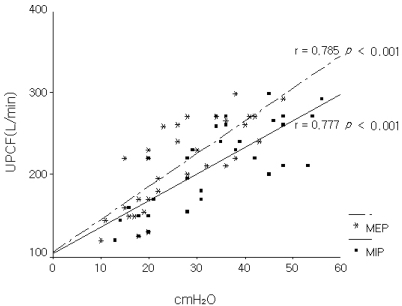
Fig. 2
Relationships between maximal respiratory pressures and VPCF. Both absolute value of MIP and MEP correlated significantly with VPCF. VPCF, Volume assisted peak cough flow; MIP, Maximal inspiratory pressure; MEP, Maximal expiratory pressure.

Fig. 3
Relationships between maximal respiratory pressures and MPCF. Both absolute value of MIP and MEP correlated significantly with MPCF. MPCF, Manual assisted peak cough flow; MIP, Maximal inspiratory pressure; MEP, Maximal expiratory pressure.
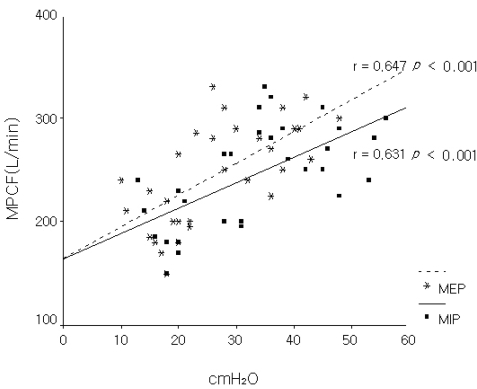
Fig. 4
Relationships between maximal respiratory pressures and CPCF. Both absolute value of MIP and MEP correlated significantly with CPCF. CPCF, Combined peak cough flow; MIP, Maximal inspiratory pressure; MEP, Maximal expiratory pressure.

Table 1
Comparisons between UPCF* and Each Assisted PCF† (n = 32)
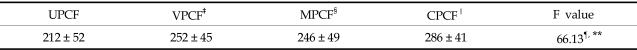
Mean values ± SD (liters/min).
*UPCF = unassisted peak cough flow; †PCF = peak cough flow; ‡VPCF = volume assisted peak cough flow; §MPCF = manual assisted peak cough flow; ∥CPCF = combined peak cough flow, ¶p < 0.001, **Both the values of VPCF and MPCF, which were similar, were higher than that of UPCF but lower than that of CPCF.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download