Abstract
Torsion of the gallbladder is a rare entity that is difficult to diagnose preoperatively. The condition occurs most often in the elderly. Although its etiology is unknown, a constant finding is the presence of the gallbladder on a mobile mesentery (floating gallbladder). Torsion, or volvulus, of the gallbladder occurs when it twists axially, with the subsequent occlusion of bile and/or blood flow. Herein, a case of torsion of the gallbladder is presented where preoperative computed tomographic scan and laparoscopy were successfully used to diagnose and treat this condition without the usual requirement of open exploration. Given the possibility of laparoscopic cholecystectomy and the increasing incidence with which torsion of the gallbladder is being witnessed today, the importance of a preoperative computed tomographic scan is emphasized when there is a high index of clinical suspicion.
Torsion of the gallbladder (GB) is an uncommon occurrence, the exact etiology of which is poorly understood.1-11 What is certain is that prompt surgical intervention is imperative with this condition to avoid the potential risk and catastrophic consequence of gangrene and perforation. The treatment of choice is an immediate cholecystectomy. Although most cases are diagnosed at the time of surgery, earlier diagnosis in light of the recent upward trend of reported cases is particularly important in the laparoscopic era, where the treatment strategies will be influenced. Here, the case of an elderly patient with torsion of the GB, presenting with symptoms of acute acalculous cholecystitis, is reported. In our case, a preoperative computed tomographic (CT) scan provided an important diagnostic clue, and a laparoscopy was successfully used to treat this condition without the usual requirement of open exploration. Torsion of the GB remains a benign condition if diagnosed rapidly and treated appropriately. Therefore, it should be included in the differential diagnosis of elderly patients presenting with symptoms of acute acalculous cholecystitis.
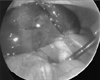
A 94-year-old female presented at the emergency room with a 1-day history of abdominal pain. She had a medical history of hypertension, for which she was being treated with anti-hypertensive agents. The abdominal pain had started as epigastric discomfort, which increased in intensity and then became more localized to the right lower quadrant. The pain was sharp and constant in nature. There was no history of nausea, vomiting, fever, chills, diarrhea or constipation. Physical examination revealed a thin elderly woman (body weight, 40 kg) with a temperature of 36.3℃, blood pressure of 200/90 mmHg and pulse of 94 beats/min. The abdomen was soft and mildly distended, with a palpable mass and diffuse tenderness in the right lower quadrant. No guarding and rebound tenderness were appreciated. An initial complete blood count revealed hemoglobin of 10.1g/dL, hematocrit of 30.3% and white blood cell count of 6,600/µL. Other blood chemistry parameters were unremarkable. Routine chest and abdominal radiographs were also unremarkable. A contrast-enhanced axial CT scan demonstrated a massively distended "floating GB", with a conical structure connecting the GB to the liver (Fig. 1). No stones were identified. A presumptive diagnosis of torsion of the GB was considered, with diagnostic laparoscopy performed to confirm the diagnosis. During the laparoscopic procedure, the GB was markedly distended, hemorrhagic and "floating" away from the liver bed (Fig. 2). The GB was twisted around its axis at the level of the cystic duct and artery, forming a complete torsion of the GB. Three-port laparoscopic cholecystectomy was performed without complications. A pathologic specimen showed features of a transmural hemorrhage and congestion, compatible with torsion of the GB. The postoperative course was uneventful and the patient was discharged on postoperative day 6.
Torsion of the GB is an uncommon occurrence, with a reported incidence of one in 365,520 hospital admissions.1-10 The condition can occur at any age and in either sex, but has a predilection for the elderly, with a 3 : 1 female-to-male ratio.1-10 The etiology is unknown; however, several factors are postulated as playing causative roles.1-10
There are two requirements for torsion of the GB: an anatomic configuration, allowing rotational GB mobility, and a triggering event that results in the GB twisting around the cystic duct as an axis point.1 The anatomic configurations necessary for torsion of the GB are well documented, but the triggering event is poorly understood.
Two types of anomalies have been implicated in the majority of cases, as well as a third, less common condition.1-3 The first may be related to the congenital deformity. Between the 4th and 7th weeks of embryological development, the pars cystica forms from the hepatic diverticulum. Abnormal migration, with an absence of a GB mesentery, creates a "free-floating GB". The second occurs by generalized visceroptosis. The mesentery of the GB and cystic duct relax and elongate, creating a mobile situation. Atrophy of the liver, loss of visceral fat and elasticity with aging, weight loss and spinal deformities may place the GB in a more dependent position, with a predisposition to torsion. Arteriosclerosis, tortuosity of the cystic duct, cholelithiasis with acute dilatation, violent movements and intense peristalsis of adjacent viscera may also contribute. The third and least common anatomic configuration involves a normal GB to liver attachment; however, the lobe of the liver itself lacks coronary and triangular ligaments, which allows the GB and liver lobe, as a unit, to undergo torsion around the cystic duct.
The two types of torsion that may occur are: complete torsion, with a greater than 180-degree rotation, and incomplete torsion, with a rotation of less than 180 degrees.1-3 Complete torsion occludes both the bile and blood flows, whereas incomplete torsion occludes only the bile flow. Intense peristalsis by the stomach or duodenum has been implicated in clockwise rotation, whereas the transverse colon is implicated in counterclockwise rotation.1-3
Nonspecific symptoms make the preoperative diagnosis of torsion of the GB difficult on the basis of history and physical examination alone.1-10 Laboratory investigations are usually unhelpful. In recent years, the preoperative diagnosis of this entity has been facilitated with the use of ultrasound and CT scan.4 Safadi et al. reported that the presence of the GB outside its fossa, and inferior to the liver, with an echogenic conical structure are specific sonographic signs of torsion.10 Merine et al. also proposed that a massively distended GB, resembling a fluid-filled loop of the bowel with a circular high attenuation structure to the right of the GB on CT scan, were specific signs of torsion of the GB.11 The diagnostic imaging criteria for torsion of the GB can be summarized as follows; fluid collection between the GB and the liver bed indicating a "floating GB", a GB positioned horizontally along its long axis indicating a free-lying GB, the presence of a well-enhanced cystic duct located on the right side of the GB visualized on CT scan and signs of inflammation, ischemia or necrotic change of the GB.4 In our case, a preoperative CT scan provided several important diagnostic clues; the presence of the GB outside its fossa and inferior to the liver, with a conical structure connecting the GB to the liver, fluid collection between the GB and the liver bed, indicating a "floating GB", and a massively distended GB with wall thickening.
When torsion of the GB is suspected, an emergency cholecystectomy should be performed. Laparoscopic cholecystectomy is recommended for treating torsion of the GB, as the GB is minimally adhered to the liver bed, so can be performed easily, with minimal invasion.5 In our case, laparoscopic surgery was successfully performed to confirm the diagnosis and treat this condition without the usual requirement of open exploration.
In conclusion, a preoperative CT scan can provide an important diagnostic clue, and laparoscopy successfully used to treat this condition without the usual requirement of open exploration. Torsion of the GB remains a benign condition if diagnosed rapidly and treated appropriately. Therefore, it should be included in the differential diagnosis when such findings are seen on a CT scan in elderly patients presenting with symptoms of acute acalculous cholecystitis.
Figures and Tables
References
1. Schroder DM, Cusumano DA 3rd. Laparoscopic cholecystectomy for gallbladder torsion. Surg Laparosc Endosc. 1995. 5:330–334.
2. Vosswinkel JA, Colantonio AL. Torsion of the gallbladder: laparoscopic identification and treatment. Surg Endosc. 1999. 13:1154–1156.
3. Losken A, Wilson BW, Sherman R. Torsion of the gallbladder: a case report and review of the literature. Am Surg. 1997. 63:975–978.
4. Kalimi R, Zarcone J 3rd, McNelis J. Acute necrotizing torsion of the gallbladder. Am Surg. 2001. 67:748–751.
5. Nakao A, Matsuda T, Funabiki S, Mori T, Koguchi K, Iwado T, et al. Gallbladder torsion: case report and review of 245 cases reported in the Japanese literature. J Hepatobiliary Pancreat Surg. 1999. 6:418–421.
6. Aibe H, Honda H, Kuroiwa T, Yoshimitsu K, Irie H, Shinozaki K, et al. Gallbladder torsion: case report. Abdom Imaging. 2002. 27:51–53.
7. Lyons KP, Challa S, Abrahm D, Kennelly BM. Floating gallbladder: a questionable preclude to torsion: a case report. Clin Nucl Med. 2000. 25:182–183.
8. Nguyen T, Geraci A, Bauer JJ. Laparoscopic cholecystectomy for gallbladder volvulus. Surg Endosc. 1995. 9:519–521.
9. Gonzalez-Fisher RF, Vargas-Ramirez L, Rescala-Baca E, Dergal-Baude E. Gallbladder volvulus. HPB Surg. 1993. 7:147–148.
10. Safadi RR, Abu-Yousef MM, Farah AS, al-Jurf AS, Shirazi SS, Brown BP. Preoperative sonographic diagnosis of gallbladder torsion: report of two cases. J Ultrasound Med. 1993. 12:296–298.
11. Merine D, Meziane M, Fishman EK. CT diagnosis of gallbladder torsion. J Comput Assist Tomogr. 1987. 11:712–713.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download